Abstract
In infants of diabetic mothers, maternal-fetal hyperglycemia induces fetal hyperinsulinemia, which may be sustained for several hours after birth. The inhibitory effect of insulin on glycogenolysis, gluconeogenesis, and lipolysis increases the risk of hypoglycemia in these infants. Eight term infants of diabetic mothers were studied between 3.9 and 8.5 h postnatally. The maternal diabetes was considered well controlled as judged by self-monitoring of blood glucose and Hb A1c. Neonatal plasma concentrations of glucose, glycerol, and insulin were monitored and averaged 2.7 ± 0.7 mM, 371 ± 116μM, and 15.9 ± 2.8 μU·mL-1, respectively. Stable isotope-gas chromatography/mass spectrometry techniques were used to determine glucose and glycerol turnover rates and gluconeogenesis from glycerol in the infants. The appearance rates of glucose and glycerol averaged 20.0 ± 5.4 μmol·kg-1·min-1 (3.6 ± 1.0 mg·kg-1·min-1), and 8.9 ± 2.3μmol·kg-1·min-1, respectively. The fraction of glycerol appearance rate converted to glucose was 68.2 ± 17.3%, which accounted for 15.5 ± 4.6% of glucose production. Thus, compared with healthy term infants studied previously under identical conditions, the infants of diabetic mothers had higher insulin concentrations and attenuated glucose production. Despite increased insulin concentrations, lipolysis was unimpaired, and the gluconeogenic contribution from glycerol was higher than in the healthy newborns.
Similar content being viewed by others
Main
After cessation of the transplacental flow of nutrients, most healthy term newborn infants promptly initiate hepatic glucose production and establish normal blood glucose concentrations(1). Because the glycogen stores can supply the infant's full need of glucose for only about 10 h(2), glycerol and other gluconeogenic carbon become increasingly important substrates for production of new glucose in the immediate postnatal period(3–5).
Fetuses of diabetic mothers often accumulate large substrate stores as a result of maternal-fetal hyperglycemia(6). Fetal hyperglycemia, in turn, induces hyperinsulinemia, which may be sustained for several hours after birth. The inhibitory effect of insulin on glycogenolysis, gluconeogenesis, and lipolysis increases the risk of neonatal hypoglycemia(6).
A few studies have assessed glucose production rates in IDMs over the last two decades(5, 7–11). The earliest study, performed in the late 1970s(7), reported attenuated glucose production rates in IDMs, whereas the following four did not show any differences between IDMs and healthy controls(5, 8–10). These findings were attributed to improved maternal diabetes care. However, a recent study(11) of IDMs, whose mothers were considered strictly controlled, reported lower neonatal glucose production rates compared with those of healthy control infants. This is in accordance with the results from studies of the neonatal outcome of pregnancies complicated by gestational diabetes, where despite tight maternal control, liberal and intensive insulin treatment, an increased incidence of perinatal complications, e.g. hypoglycemia and increased birth weights, was found(12, 13). Based on these data(11–13) we hypothesized that, even with careful maternal screening, diagnosis, treatment, and follow-up during pregnancy and delivery, some infants of diabetic mothers may have residual effects of functional hyperinsulinism. Because of insulin's antilipolytic effect, the principal objective of the present study was to determine whether lipolysis was impaired, thereby limiting glycerol's role as a gluconeogenic precursor. To the best of our knowledge the dynamics of glycerol metabolism has previously been addressed only by a single study of a small number of infants(5).
METHODS
Subjects. The subjects of the study were eight term newborn infants of diabetic mothers. The research was approved by the Human Ethics Committee of the Medical Faculty of the University of Uppsala. Parental consent was obtained after oral and written information was provided.
Six mothers had gestational diabetes (those of infants nos. 1-6)(Table 1). They were diagnosed at a mean gestational age of 31.3 ± 4.5 wk (Table 1) either by a 75-g oral glucose tolerance test showing a blood glucose concentration of >8 mM 2 h after the glucose load or repeated postprandial blood glucose concentrations of >7 mM. Four of the mothers (those of infants nos. 1-4) with a 2-h glucose value >9 mM after a 75-g oral glucose tolerance test, received insulin treatment for 1-13 wk (Table 1), whereas those of infants nos. 5 and 6 were managed by diet alone for 10 wk each(Table 1). These two mothers were subjected to repeated 24-h blood glucose profiles. The mother of infant no. 7 was classified as a type II diabetic and was treated with oral medication before pregnancy. The diabetic disease of the mother of infant no. 8 was diagnosed during a previous pregnancy. Because her need of insulin remained after delivery, she was classified as a type I diabetic. Both of these mothers received insulin throughout pregnancy. All insulin-dependent mothers were managed with three to six injections of insulin/d. Adjustments were based on self-monitored blood glucose values, 24-h blood glucose profiles, and Hb A1c. In five of six insulin-treated mothers, Hb A1c was normal, i.e. ≤5.2%, whereas Hb A1c in the mother of infant no. 8 was moderately increased (6.4%). The diet-treated mothers were followed by self-monitoring of blood glucose. Based on these data, the insulin as well as the diet-treated mothers were considered well controlled by the diabetologists and obstetricians.
All insulin-treated mothers, except for that of infant no. 7, remained normoglycemic throughout labor and delivery and received no insulin during the last 10-16 h before delivery. Due to elevated blood glucose values(Table 1), the mother of infant no. 7 received two doses of short-acting insulin at 7 and 1 h before delivery.
Seven of the infants were delivered vaginally and one by cesarean section(no. 1). The deliveries were uncomplicated, and all Apgar scores were >7 at 1, 5, and 10 min. None of the infants showed any signs of illness or malformation.
All infants were admitted to the neonatal unit at Uppsala University Children's Hospital. The gestational age of the infants ranged from 37 to 41 wk, as estimated by ultrasound examination during pregnancy and confirmed by maternal menstrual history and physical characteristics according to the method of Finnström(14). The birth weights averaged 4011 g, ranging from 3651 to 5153 g (Table 2). Thus, infants no. 1 and 3 were large for gestational age (>+2 SD according to the Swedish growth standard)(15). The infants were studied between 3.9 ± 1.5 h and 8.5 ± 1.4 h postnatally(Table 2). They were clothed and resting comfortably in neonatal cribs at ambient room temperature. All of them had normal axillary temperature, 36.5-37.5 °C, throughout the study. One infant (no. 2) was jittery at an age of 1.5 h, and was found to have a blood glucose concentration of 1.1 mM. This infant, as well as infant no. 3, who had no symptoms but a blood glucose concentration of 1.6 mM 0.5 h after birth, received parenteral glucose. Because normoglycemia (blood glucose concentrations ≥2.0 mM) in both infants was achieved and maintained at glucose infusion rates of 1.7 and 1.8 mg·kg-1·min-1, respectively, they were kept on these rather low infusion rates throughout the study period. The other six infants remained normoglycemic without exogenous glucose. None of the infants was fed orally. For comparison purposes, the results obtained in this study were matched with those of a previous study of eight healthy term infants born to nondiabetic mothers and studied under identical conditions in our nursery(3) (Tables 2 and 3).
Isotope tracers. The tracers used were[6,6-2H2]glucose (isotopic purity 98 atom% of 2H2) and [2-13C]glycerol (isotopic purity 98 atom% 13C), purchased from Cambridge Isotope Laboratories, Woburn, MA. The[6,6-2H2]glucose and [2-13C]glycerol were dissolved in 0.9% saline in concentrations of 4.5 and 1.2 mg·mL-1, respectively. The solutions were sterile in microbiologic cultures and pyrogen-free when tested by the Limulus lysate method(16).
Study design. The tracers were administered simultaneously as a primed constant rate infusion for 4.6 ± 1.3 h (3.5-7.5) via a peripheral vein catheter, whereas a second peripheral vein catheter, kept patent by intermittent flushing with saline, was used for blood sampling. The sampling site was kept warm by use of plastic bags, filled with warm water.
After a priming dose of 27.3 ± 0.7 μmol·kg-1 (4.9± 0.1 mg·kg-1), given over 5 min,[6,6-2H2]glucose was administered at a constant rate of 0.70± 0.11 μmol·kg-1·min-1 (0.13 ± 0.02 mg·kg-1·min-1). The [2-13C]glycerol was given at a constant rate of 0.37 ± 0.07μmol·kg-1·min-1 after a priming dose of 14.6± 1.0 μmol·kg-1. The tracers were delivered by a calibrated volumetric pump (IMED 965 micro, IMED, Oxford, England). After a baseline sample, 300 μL of blood were collected into ice-cold EDTA tubes every 30 min from 1 h after the start of the tracer infusion. Total blood loss was ≤3 mL.
Chemical procedures. Plasma was separated immediately by centrifugation, and the plasma glucose concentration was measured within 5 min by the glucose oxidase-peroxidase method in a glucose analyzer, Ames Minilab 1(Bayer AG, Leverkusen, Germany) as described previously(17). The remaining plasma was frozen at -70 °C pending further analysis. Using a RIA technique described previously(18), plasma insulin concentrations were measured at the beginning of the study by pooling plasma from the first two samples, and at the end of the study period by pooling the last two samples.
An internal standard of [1,1,2,3,3-2H5]glycerol purchased from Cambridge Isotope Laboratories was added to the plasma samples for quantitation of plasma glycerol as described previously(19). Plasma proteins were precipitated with acetone, and the pentaacetate derivative of glucose and triacetate derivative of glycerol were prepared by addition of a molar excess of pyridine and acetic anhydride in equal amounts. The isotopic enrichments of[6,6-2H2]glucose, [2-13C]glycerol, and[1,1,2,3,3-2H5]glycerol were determined by gas chromatography/mass spectrometry using standard curves as described previously(19). A Finnigan SSQ 70 mass spectrometer (Finnigan MAT, San José, CA) equipped with a Varian 3400 gas chromatograph (Varian Associates Inc., Sunnyvale, CA) with a nonpolar (DB 1) capillary column (15 m× 0.25 mm) was used. The temperature of the oven was set at 180 and 130°C for glucose and glycerol, respectively. Methane chemical ionization was used with selected ion monitoring of m/z 331, 332, and 333 reflecting unlabeled, 13C-enriched (M+1) and dideuterated glucose(M+2), respectively, and m/z 159, 160, and 164 corresponding to unlabeled glycerol, 13C-labeled glycerol (M+1), and the pentadeuterated internal standard (M+5)(20).
Calculations. During periods of approximate substrate steady state as defined below(21), glycerol concentrations in plasma were calculated from the ion current ratio 159/164, using inverse isotope dilution principles relative to the labeled internal standard(22). Plasma Ra of glucose and glycerol were derived from isotopic enrichments of[6,6-2H2]glucose and [2-13C]glycerol. The plasma Ra of glucose (i.e. hepatic glucose production, GPR) and glycerol (glycerol Ra) were calculated as follows: Ra = i × 100/IE; i is the infusion rate of the tracer and IE the molecular ratio of labeled/unlabeled substrate. In infants nos. 2 and 3 GPR was obtained by subtracting the exogenously given glucose from the plasma glucose Ra. The fraction of glycerol converted to glucose and the fraction of glucose derived from glycerol were calculated from13 C enrichment of glucose reflected by m/z 332/331 as described by Patel and Kalhan(5) and Bougnères et al.(21).
Statistical analyses. Data are presented as mean ± SD. Simple linear regression analyses were used to test for statistical significance of variables related to plasma Ra of glycerol and glucose as well as to fractions of glycerol converted to glucose and fraction of hepatic glucose production derived from glycerol. The t test was used for comparisons of results obtained in the infants of diabetic mothers included in this study and healthy term newborns investigated in a previous study(3).
RESULTS
Table 2 describes patient characteristics,i.e. gestational age, birth weight, and postnatal age at study of the IDMs as well as of the healthy control infants studied previously by us(3). From this table it appears that the birth weight of the IDMs averaged 4011 ± 491 g, which is significantly higher than that of the healthy control infants (mean 3271 ± 490 g; p < 0.05).
Plasma concentrations of glucose and glycerol remained relatively stable during the last 2.5 ± 1.4 h of the study periods designated as the“steady state” period(22). Plasma glucose averaged 2.7 ± 0.7 mM (coefficient of variation < 10% in five subjects and 10.7, 11.0, and 14.4% in the remaining three) in the IDMs and in the healthy control infants 2.9 ± 0.4 mM (Table 3)(3). In the IDMs plasma glycerol averaged 371 ± 116 μM (coefficient of variation < 10% in five subjects and 10.5, 14.5, and 16.5% in the remaining three) and in the healthy control infants 369± 89 μM (Table 3)(3). Plasma insulin during the steady state period averaged 15.9 ± 2.8μU·mL-1. Plasma insulin in healthy control infants averaged 9.4 ± 3.7 μU·mL-1(3), a value significantly lower than the level observed in the IDMs (p < 0.005).
GPR during the steady state period averaged 20.0 ± 5.4μmol·kg-1·min-1 (3.6 ± 1.0 mg·kg-1·min-1) in the IDMs and 25.0 ± 3.5μmol·kg-1·min-1 (4.5 ± 0.6 mg·kg-1·min-1) in the healthy control infants studied previously (Table 3)(3). Thus, GPR was significantly lower in the IDMs (p < 0.05). In contrast, glycerol Ra did not differ between IDMs and healthy control infants, averaging 8.9 ± 2.3μmol·kg-1·min-1 and 8.7 ± 1.2μmol·kg-1·min-1, respectively(Table 3)(3).
The relative amount of glycerol Ra converted to glucose was 68.2 ± 17.3% accounting for 15.5 ± 4.6% of hepatic glucose production (Table 3). The corresponding values for healthy control infants were 57.9 ± 8.4% and 11.1 ± 2.3%, respectively (Table 3)(3).
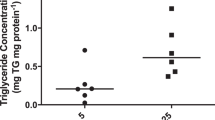
Thus, although the mean plasma concentration of insulin was significantly higher and hepatic glucose production was significantly lower in IDMs compared with the healthy control infants(3)(Table 3), glycerol contributed a larger proportion of hepatic glucose production in the IDMs (p < 0.05)(Table 3). When both groups of infants were analyzed together the gluconeogenic contribution from glycerol was inversely related to GPR (p < 0.05; r = -0.62) (Fig 1).
Relationship between hepatic glucose production and gluconeogenic contribution from glycerol. Infants of diabetic mothers (•) are analyzed together with healthy term infants (○) included in a previous study conducted in our laboratory(3).
Neither GPR nor glycerol Ra was related to plasma glucose concentration, glycerol concentration, birth weight, gestational age, postnatal age, duration of treatment of the maternal diabetes, or maternal blood glucose concentrations during delivery.
DISCUSSION
Although the maternal diabetes was considered well controlled, as judged by self-monitoring of blood glucose and Hb A1c, the insulin concentrations of our IDM infants were significantly higher and the hepatic glucose production rates lower than those found in healthy term infants studied previously under identical conditions in our nursery(3). Nonetheless, despite the higher insulin concentrations, lipolysis in term infants of diabetic mothers was of the same magnitude as that of healthy term infants within 4 h of birth. Further, as indicated by its larger contribution to hepatic glucose production compared with that of healthy newborns(3), glycerol was a more important source of gluconeogenic carbon in the IDMs.
In contrast to our findings in healthy newborns(3), plasma concentrations of glucose and glycerol were unrelated to the corresponding production rates. This suggests that the interrelation between substrate concentrations and production rates, normally established soon after birth(3), is delayed in infants of diabetic mothers.
Although attenuated glucose production is in accordance with insulin's inhibitory effect on glycogenolysis and gluconeogenesis, our finding of unimpaired lipolysis, despite increased insulin concentrations, is in contrast to the marked antilipolytic effect exerted by corresponding insulin concentrations in adults(23–26). On the other hand, our results are in agreement with those of Patel and Kalhan(5), who also reported glycerol turnover rates in IDMs close to those of healthy control infants despite increased concentrations of total insulin and C-peptide. One possible explanation for preserved lipolysis in IDMs, despite moderately increased insulin concentrations, may be that high concentrations of lipolytic hormones, e.g. thyroid-stimulating hormone and catecholamines(27, 28) counteract insulin's inhibitory effect. In vitro, TSH has been shown to have a more pronounced lipolytic effect on neonatal adipocytes than catecholamines(27). In vivo, Stern et al.(29) proved the lipolytic effect of catecholamines by demonstrating that exogenous administration of adrenaline to newborn IDMs increased the concentration of FFA(29). The combination of attenuated glucose production and unimpaired lipolysis would indicate that TSH has a more marked effect on lipolysis than catecholamines. However, there may also be a difference in sensitivity to insulin's inhibitory effect between adipose and hepatic tissue.
The role of glycerol as a gluconeogenic precursor has previously been determined only in two IDMs(5). These two infants had a gluconeogenic contribution from glycerol close to that found in healthy newborns, whereas our results show, in a larger group of infants, that in the IDMs, a significantly larger proportion of hepatic glucose output is derived from glycerol(3). The gluconeogenic contribution from glycerol was inversely related to hepatic glucose production (Fig. 1), suggesting that glycerol becomes a more important gluconeogenic substrate when hepatic glucose production is impaired. One may speculate that preserved lipolysis makes glycerol a readily accessible substrate for hepatic glucose production.
Previous studies of glucose kinetics in infants of diabetic mothers have shown diverging results(5, 7–11). Four of these studies were conducted in the same laboratory over a period of about 15 y(5, 8–10). The earliest one showed attenuated hepatic glucose production in IDMs(9), whereas the following two did not demonstrate any difference between IDMs and healthy control infants. This was attributed to improved maternal diabetes care(5, 8). On the contrary, and in agreement with our results, the most recent study showed lower GPR in IDMs, although the maternal diabetes was considered strictly controlled(11). The elevated insulin concentrations, attenuated neonatal hepatic glucose production, and higher birth weights in our IDMs, compared with our healthy control infants, indicate that the mothers were not strictly controlled. Thus, our data support the contention that, neither maternal Hb A1c nor self-monitoring of blood glucose are precise predictors of fetal glycemic control during late pregnancy(13, 30). The variation in severity of metabolic disturbance, as well as in onset of the diabetic disease and response to treatment, make it difficult to establish guidelines for screening, diagnosis, treatment, and follow-up during pregnancy. Although not severe, the metabolic derangement found in our IDMs indicate a need of more sensitive tools for evaluation of maternal/fetal control during pregnancy.
In conclusion, the results of the present study show that, in IDMs of mothers considered well controlled, neonatal insulin concentrations were increased. Despite increased insulin concentrations lipolysis was of the same magnitude as that of healthy infants, indicating that insulin's antilipolytic effect was attenuated. Further, the amount of glycerol carbon directed to glucose via gluconeogenesis was larger in the IDMs. We speculate that high postnatal levels of lipolytic hormones may counteract the antilipolytic effect of insulin. In addition, because hepatic glucose production was attenuated, whereas lipolysis was preserved in the IDMs, our results also suggest that the adipose tissue is less sensitive to insulin than is the liver.
Abbreviations
- GPR:
-
hepatic glucose production rate
- IDM:
-
infant of diabetic mother
- R a :
-
appearance rate
References
Ogata ES 1986 Carbohydrate metabolism in the fetus and neonate and altered neonatal glucoregulation. Pediatr Clin North Am 33: 25–45.
Bougnères PF 1987 Stable isotope tracers and the determination of fuel fluxes in newborn infants. Biol Neonate 52( suppl I): 87–96.
Sunehag A, Gustafsson J, Ewald U 1996 Glycerol carbon contributes to hepatic glucose production during the first eight hours in healthy, term infants. Acta Paediatr 85: 1339–1343.
Girard J 1986 Gluconeogenesis in late fetal and early neonatal life. Biol Neonate 50: 237–258.
Patel D, Kalhan S 1992 Glycerol metabolism and triglyceride- fatty acid cycling in the newborn: effect of maternal diabetes and intrauterine growth retardation. Pediatr Res 31: 52–58.
Cowett RM 1991 Infant of the diabetic mother. In: Cowett RM (ed) Principles of Perinatal-Neonatal Metabolism. Springer-Verlag, New York, pp 678–698.
Kalhan SC, Savin SM, Adam PAJ 1977 Attenuated glucose production rate in newborn infants of insulin dependent diabetic mothers. N Engl J Med 296: 375–376.
King KC, Tserng K-Y, Kalhan S 1982 Regulation of glucose production in newborn infants of diabetic mothers. Pediatr Res 16: 608–612.
Cowett RM, Susa JB, Giletti B, Oh W, Schwartz R 1983 Glucose kinetics in infants of diabetic mothers. Am J Obstet Gynecol 146: 781–786.
Baarsma R, Reijngoud D-J, van Asselt WA, van Doormaal JJ, Berger R, Okken A 1993 Postnatal glucose kinetics in newborns of tightly controlled insulin-dependent diabetic mothers. Pediatr Res 34: 443–447.
Kalhan SC 1993 Rates of urea synthesis in the human newborn: effect of maternal diabetes and small size for gestational age. Pediatr Res 34: 801–804.
Sunehag A, Berne C, Lindmark G, Ewald U 1991 Gestational diabetes-perinatal outcome with a policy of liberal and intensive insulin therapy. Upsala J Med Sci 96: 185–198.
Persson B, Hansson U 1996 Fetal size at birth in relation to quality of blood glucose control in pregnancies complicated by pregestational diabetes mellitus. Br J Obstet Gynaecol 103: 427–433.
Finnström O 1977 Studies on maturity in newborn infants. IX Further observations on the use of external characteristics in estimating gestational age. Acta Paediatr Scand 66: 601–604.
Niklasson A, Ericson A, Fryer J G, Karlberg J, Lawrence C, Karlberg P 1991 An update of the Swedish reference standards for weight, length and head circumference at birth for given gestational age (1977-1981). Acta Paediatr Scand 80: 756–762.
Guideline on validation of the Limulus amebocyte lysate test as an end-product endotoxin test for human and animal parenteral drugs, biological products, and medical devices. U.S. Food and Drug Administration, December 1987
Sunehag A, Ewald U, Larsson A, Gustafsson J 1993 Glucose production rate in extremely immature neonates (<28 wk) studied by use of deuterated glucose. Pediatr Res 33: 97–100.
Sunehag A, Gustafsson J, Ewald U 1994 Very immature infants (≤30 wk) respond to glucose infusion with incomplete suppression of glucose production. Pediatr Res 36: 550–555.
Sunehag A, Ewald U, Gustafsson J 1996 Extremely preterm infants (<28 weeks) are capable of gluconeogenesis from glycerol on their first day of life. Pediatr Res 40: 553–557.
Fjeld CR, Cole FS, Bier DM 1992 Energy expenditure, lipolysis, and glucose production in preterm infants treated with theophylline. Pediatr Res 32: 693–698.
Bougnères PF, Karl IE, Hillman LS, Bier DM 1982 Lipid transport in the human newborn. Palmitate and glycerol turnover and the contribution of glycerol to neonatal hepatic glucose output. J Clin Invest 70: 262–270.
Bougnères PF, Bier DM 1982 Stable isotope dilution method for measurement of palmitate content and labeled palmitate tracer enrichment in microliter plasma samples. J Lipid Res 23: 502–507.
Pei D, Chen Y-DI, Hollenbeck CB, Bhargava R, Reaven GM 1995 Relationship between insulin-mediated glucose disposal by muscle and adipose tissue lipolysis in healthy volunteers. J Clin Endocrinol Metab 80: 3368–3372.
Jahoor F, Klein S, Wolfe R 1992 Mechanism of regulation of glucose production by lipolysis in humans. Am J Physiol 262:E353–E358.
Nurjhan N, Consoli A, Gerich J 1992 Increased lipolysis and its consequences on gluconeogenesis in non-insulin dependent diabetes mellitus. J Clin Invest 89: 169–175.
Fanelli C, De Feo P, Porcellati F, Perriello G, Torione E, Santeusanio F, Brunetti P, Bolli GB 1992 Adrenergic mechanisms contribute to the late phase of hypoglycemic glucose counterregulation in humans by stimulating lipolysis. J Clin Invest 89: 2005–2013.
Marcus C, Ehrén H, Bolme P, Arner P 1988 Regulation of lipolysis during the neonatal period. Importance of thyrotropin. J Clin Invest 82: 1793–1797.
Lagercrantz H, Bistoletti P 1973 Catecholamine release in the newborn infant at birth. Pediatr Res 11: 889–893.
Stern L, Ramos A, Leduc J 1968 Urinary catecholamine excretion in infants of diabetic mothers. Pediatrics 42: 598–605.
Brans YW, Huff RW, Shannon DL, Hunter MA 1982 Maternal diabetes and neonatal macrosomia. I Postpartum maternal hemoglobin A1c levels and neonatal hypoglycemia. Pediatrics 70: 576–580.
Acknowledgements
The authors thank Elisabeth Söderberg, the staff of the NICU Uppsala University Children's Hospital, Anders Ingvast, and Ulf Bondesson, SVA Uppsala, for skillful assistance; Dr. Claes GöranÖstensson and Elvy Sandberg, Karolinska Institute, Stockholm, for insulin analyses; and Dr. Dennis M. Bier, Children's Nutrition Research Center, Houston, TX, for valuable, constructive discussions of this manuscript.
Author information
Authors and Affiliations
Additional information
Supported by grants from the Swedish Medical Research Council (Projects 4792 and 11282), Novo Nordisk Pharma AB, the Swedish Diabetic Association, the Ernfors Family Foundation, the Gillberg Foundation, the Jerring Foundation, Mutual Group Life Insurance Company, Stockholm, Sweden, and the Swedish Society for Medical Research.
Rights and permissions
About this article
Cite this article
Sunehag, A., Ewald, U., Larsson, A. et al. Attenuated Hepatic Glucose Production but Unimpaired Lipolysis in Newborn Infants of Mothers with Diabetes. Pediatr Res 42, 492–497 (1997). https://doi.org/10.1203/00006450-199710000-00012
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199710000-00012
This article is cited by
-
Care of the Infant of the Diabetic Mother
Current Diabetes Reports (2012)