Abstract
The role of an ATP-dependent K+ channel (K(ATP)+) relaxation in the porcine pulmonary vasculature from birth to adulthood was investigated in vitro using levcromakalim on isolated, prostaglandin F2α (30 μM)-precontracted conduit arteries (CA), resistance arteries (RA), and veins (PV). Vessels from neonatal pulmonary hypertensive piglets exposed to chronic hypobaric hypoxia (CHH, 51 kPa) for 3 d, either from birth or from 3 d of age were also studied. Levcromakalim relaxed all vessels in a concentration- and glibenclamide-sensitive manner. In normal CA, the maximal extent of relaxation and sensitivity (EC50) increased between birth and 17 d. Endothelium-removal increased EC50 at 17 d only. Indomethacin (10 μM), but not NG-monomethyl-L-arginine (L-NMMA) (30 μM), inhibited relaxation in CA from newborn, 3-d-old, and adult animals. In RA, levcromakalim-induced relaxations did not change during development and endothelium-removal attenuated relaxations in 3-d-old but not in adult animals. At both ages in RA, L-NMMA attenuated relaxations and subsequent addition of L-arginine (1 mM) restored them. In PV, maximal relaxation increased between birth and 6 d with no change of EC50. At all ages, relaxation was partially endothelium-dependent and inhibited by L-NMMA (except in the newborn). Indomethacin only attenuated relaxations in veins from 6- and 17-d-old animals. CHH did not influence relaxant responses in CA and PV but decreased EC50 in RA. Thus K(ATP)+ channel activation caused relaxation from birth onward in all vascular segments with varying endothelium dependence. CHH did not affect relaxation in the large vessels and up-regulated those in RA. These findings indicate a possible role for K(ATP)+ channels during normal adaptation and a potential therapeutic role in the management of pulmonary hypertensive newborn infants.
Similar content being viewed by others
Main
The pulmonary circulation changes abruptly at birth from a high resistance-low flow system to a low resistance-high flow vascular bed. The mechanisms responsible for this change are not clear. Endothelium-derived relaxing factor (NO) helps control pulmonary vascular resistance in the ovine fetus and contributes to the fall in resistance at birth(1). However, it appears that endothelium-dependent relaxations (through NO) are less effective immediately after birth than they are at about 1 wk of age in several species(2, 3). In isolated porcine pulmonary arteries, for example, the relaxant response to acetylcholine is absent at birth but present by 60 h of age(2–4). In addition, the endothelium-independent response to NO improves during the first days of life(4). Given the necessity of achieving a reduction in pulmonary vascular resistance immediately after birth, we investigated the in vitro efficacy of an alternative, putative endothelium-independent pulmonary vasodilator mechanism, namely ATP-sensitive potassium channel (K(ATP)+ channel)-stimulated relaxation(5, 6). Specific K(ATP)+ channel agonists and antagonists are available(7).
Failure of the pulmonary circulation to adapt normally to extrauterine life causes persistent pulmonary hypertension and structural remodeling of the pulmonary arteries with medial hypertrophy in both humans and experimental animals(8–11). Newborn pigs exposed to CHH from birth have persistent pulmonary hypertension, and the morphologic changes in the pulmonary arteries are accompanied by a delay in the establishment of endothelium-dependent relaxation to ACH and a reduced sensitivity to exogenous NO(10).
The hypothesis of the present study was therefore that K(ATP)+ channel activation could be important in pulmonary vasodilation, not only in the adult but also in the newborn. This hypothesis was investigated by studying the in vitro responses of isolated porcine intrapulmonary vessels to the K(ATP)+ channel agonist levcromakalim. Vessels were taken from pigs at birth, during early postnatal life (normal and after exposure to CHH) and from adults. Experimental studies on the regulation of pulmonary blood flow during the neonatal period indicate that the “midsection” of the pulmonary vascular bed, the small intrapulmonary arteries, largely control the resistance to flow(12–14). The participation of the pulmonary veins in resistance regulation seems to wane during adaptation to extrauterine life(12). Therefore, we studied the efficacy of K(ATP)+ channel activation in the isolated normal and hypertensive conduit pulmonary arteries, resistance arteries and veins. Because K+ channels have been described on the endothelium(15–17), the role of the endothelium in the levcromakalim-induced responses was studied together with the possible involvement of cyclo-oxygenase products and NO(18, 19).
METHODS
Experimental Design
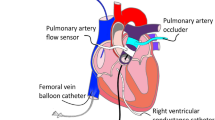
Piglets were produced by pregnant Large White sows which farrowed normally at term. Animals were killed at birth (less than 4 min old), and at the ages of 3, 6-7, and 14-17 d. In addition, other piglets were exposed to CHH (51 kPa) either from the moment of birth and then killed at 2.5 d, or exposed to CHH from 3 to 6 d of age. Within each age group, n indicates the total number of different animals studied. In the hypobaric chamber, the internal temperature (25-30 °C) and light were controlled, the animals could move about freely and were tube-fed (age ≤3 d) or fed ad libitum (age ≥3 d) with mashed feed and milk. The chamber was opened twice each day to quickly (20 min) clean and replenish food supplies. All the animals received humane care in compliance with British Home Office Regulations and with the “Principles of Laboratory Animal Care” formulated by the National Society of Medical Research and Guide for the Care and Use of Laboratory Animals prepared by the National Academy of Science and published by the National Institute of Health (National Institutes of Health, publication no 80/23, revised 1978). Animals were killed by means of a lethal intraperitoneal injection of sodium pentobarbitone (100 mg/kg). The heart-lung bloc was removed and placed in chilled PSS (composition in mM: NaCl 119, KCl 4.7, CaCl2 2.5, NaHCO3 25, Na2EDTA 0.026, KH2PO4 1.2, MgSO4 1.2, glucose 5.5, gassed with 95% O2/5%CO2). Heart-lung blocs from adult animals were obtained from the local abattoir as soon as possible after the animals were killed and transported to the laboratory in chilled PSS.
Biologic Material
Proximal intrapulmonary arteries (i.e. the axial artery, after the first major lower intralobar branch) were taken, and intrapulmonary veins were obtained from a comparable position within the lung. Vessels were cleaned of adhering connective tissue and cut into rings (dimensions given in Table 1). Endothelium removal was performed by inserting a pair of Dumont 5 tweezers in the lumen and gently rolling the preparation over a piece of filter paper. Rings were suspended in water-jacketed (35°C) glass organ baths filled with 5 mL of calcium-free PSS and mounted between two stainless steel hooks (120- or 500-μm diameter), one connected to a support, the other connected with a silk thread to a Grass FT.03 force transducer. Signals were recorded both on a grass polygraph and on a data acquisition system (MacLab for Macintosh LCII, AD-Instruments Ltd., UK).
Small muscular arteries (conventionally described and subsequently referred to as resistance arteries), approximately 800 μm in length, were isolated with standard ophthalmologic surgical instruments. In the large lungs of adult animals these vessels were obviously more peripheral than in the newborn lung. They were mounted in a small vessel myograph with two stainless steel wires(diameter 30 or 40 μm) through the lumen.
Experimental Protocols
Large vessels. Calcium-free PSS was exchanged with fresh, prewarmed, and preoxygenated calcium-containing PSS after an equilibration period (between 30 and 60 min). During this equilibration period, all vessels were transversely stretched. The conduit arteries were stretched to a level that corresponded to an effective transmural pressure of approximately 30 mm Hg (≅10 mN of stabile passive force). Veins were stretched until 2.5 mN of stabile passive force was obtained. All preparations were thus in a configuration that corresponded approximately to the circumference required to attain maximal isometric force development(4, 10). Table 1 summarizes the diameters calculated from the circumference measurements(20) of at least three preparations.
All preparations were challenged twice with K+ 40 mM (equimolar replacement of Na+) for 5 min to assess the viability of the preparations. The second challenge was used to test the presence and functional integrity of the endothelium. After the contraction had stabilized, ACH (1 or 10 μM) was added and only those preparations with endothelium that relaxed in response to ACH were included in the study. Preparations in which the endothelium had been removed either did not react to the addition of ACH or showed a slight potentiation of the K+-induced contraction. Preparations from newborn animals aged less than 3 d could not be tested this way as they do not yet possess the ability to relax in response to ACH(2, 3), but they were run through the same protocol. After testing endothelium integrity, wherever feasible, preparations were either equilibrated for another 15 min in control PSS or in PSS with glibenclamide (1 μM), L-NMMA (30 μM), indomethacin (10 μM), or the solvents distilled water, ethanol (final concentration 1%), or DMSO (final concentration, 0.2%). Preparations were subsequently challenged with 30 μM PGF2α. The choice of this contractile agonist was necessitated by the fact that, in CA, it proved to be one of the only vasoconstrictors which consistently showed contractile responses at all ages studied(21) which were ≅80-120% of K+ = 40 mM-induced contractions. In PV, PGF2α proved to have similar effects in relation to K+. After stabilization of the contraction, the responses to cumulative concentrations of levcromakalim (0.01 to 30 μM in half-log steps) were determined. After washout of PGF2α and levcromakalim, all preparations were exposed to papaverine (100 μM) to determine the maximal possible extent of relaxation. As a varying degree of spontaneous tone was present in every preparation studied(22), application of papaverine also served to normalize the concentration-response curves obtained. Each large pulmonary artery and vein was exposed to only one compound and only one complete cumulative range of levcromakalim concentrations. Interventions (endothelium removal, addition of antagonists) were studied in paired rings from the same animal with one ring serving as control. In some separate conduit arterial rings, the spontaneous, time-dependent decline of the PGF2α-induced contraction was evaluated. This amounted to 10-15% over a period of 30 min irrespective of age, normoxia, chronic hypoxia, or presence/absence of endothelium. Contractions in venous and resistance arterial preparations did not decline appreciably over the time course necessary to apply the different concentrations of levcromakalim.
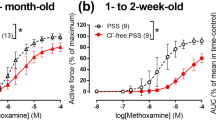
Small vessels. After mounting RA in calcium-free PSS, vessels were progressively stretched in 100-200-μm steps. Passive force recordings at each length were fitted to an exponential passive length-force curve used to determine the length corresponding to ≅30 mm Hg effective transmural pressure(23, 24). This corresponds to the optimal length for isometric force development in RA. After determination of the optimum length and challenge with high K+, endothelial integrity was verified by a challenge to 10 μM PGF2α followed by addition of 1 μM ACH (3 and 6-7 d old) or 1 nM bradykinin (adult). Failure to relax to either of these challenges was interpreted as absence of functional endothelium, and unresponsive preparations were discarded. After washout of PGF2α-ACH/bradykinin and a new challenge with high K+, preparations were exposed to 30 μM PGF2α, and a complete concentration-response curve to levcromakalim was obtained after stabilization. The amplitude of PGF2α-induced contractions was≅80-120% of K+-induced contractions. Resistance-sized pulmonary arteries were exposed to more than one complete concentration range of levcromakalim. The washout of PGF2α/levcromakalim was followed by one or two challenges to high K+, before repeating the protocol of exposure to PGF2α followed by cumulative additions of levcromakalim in the presence of either nothing (time control), after denudation of the endothelium, or after the addition of L-NMMA. This experimental protocol did not result in significant desensitization to levcromakalim as shown in Figure 1, B and D, for RA of 3-d-old and adult animals. Repeated challenges to PGF2α did not appreciably influence the contraction amplitude. In adult RA, this was 3.3± 0.8 mN/mm for the first PGF2α contraction, 2.8 ± 0.8 mN/mm for the second, and 3.6 ± 0.9 mN/mm for the third(n = 5, paired observations). Values for 3-d-old RA were 1.0± 0.2 mN/mm, 1.2 ± 0.1 mN/mm, and 1.2 ± 0.1 mN/mm respectively (n = 6, paired observations).
Effect of endothelium-removal in resistance-sized arteries on consecutively obtained concentration-response relations to levcromakalim. (A) Three-day-old piglets in which the endothelium was intact (○) or removed (▪), showing a significant difference in EC50, p = 0.023 and Rmax, p = 0.04; (n = 7). (B) Three-day-old piglets, time control: shows the reproducibility of two consecutive concentration-response relations without endothelium-denudation (○ = first exposure, • = second exposure, n = 7, paired observations). (C and D) Similar protocols for resistance arteries from adult pigs. Removal of endothelium in C did not significantly change the EC50(n = 5 for C and D).
Endothelium removal in RA was accomplished by repeatedly moving back and forth a human hair through the lumen of a myograph-mounted and stretched vessel after the first exposure to a complete range of levcromakalim concentrations. Another vessel of similar dimensions and mounted in parallel served as a time control. After denudation, the presence of functioning endothelium was tested by the application of 1 μM ACH (3-d-old animals) or 1 nM bradykinin (adult animals), with time control studies running in parallel. Denudation significantly inhibited the relaxation responses to ACH in 3-d-old animals (first response before denudation, 58 ± 7%; denuded, 5 ± 1%, n = 7, paired observations). In time control preparations, these responses were unaltered (first response, 58 ± 7%; second response, 56 ± 4%, n = 7, paired observations). The responses to high K+ and PGF2α (expressed as a fraction of the first response) were significantly reduced after endothelium removal(K+, 0.6 ± 0.1; PGF2α, 0.60 ± 0.07,n = 7). In the preparations serving as time controls, these responses (expressed as a fraction of the first response) were up-regulated for K+, but not for PGF2α (K+, 1.20 ± 0.05; PGF2α, 1.16 ± 0.09, n = 7). In adult animals(using bradykinin to obtain relaxant responses), similar changes were seen. Endothelial removal inhibited the relaxant response to bradykinin (first response before denudation, 79 ± 9%; denuded, 6 ± 2%,n = 5, paired observations). In time control preparations, these responses were unaltered (first response, 83 ± 3%; second response, 73± 5%, n = 5, paired observations). The responses to high K+, but not those to PGF2α (expressed as a fraction of the first response), were reduced after denudation (K+, 0.8 ± 0.1; PGF2α, 0.91 ± 0.09, n = 5). In the preparations serving as time controls, these responses (expressed as a fraction of the first response) were up-regulated (K+, 1.23 ± 0.06; PGF2α, 1.49 ± 0.06, n = 5). In experiments with L-NMMA, a third concentration-response study to levcromakalim was carried out. At the end of the experiment, all preparations were exposed to 100 μM papaverine.
Drugs
Levcromakalim (BRL38227) was a gift from Smith-KlineBeecham, and glibenclamide was obtained from Research Biochemicals. Both were freshly prepared as 10 mM stock solution in DMSO with subsequent dilutions in distilled water. Indomethacin (Sigma Chemical Co.) and PGF2α(Serva) were dissolved in absolute ethanol as stock solution of 0.01 M. All other drugs were obtained from Sigma Chemical Co.
Analysis of Data
The effect of levcromakalim was expressed as the percent relaxation in total active force (i.e. PGF2α-induced tone plus the spontaneous tone as determined by papaverine). All data are reported as mean± SEM. For each individual preparation, the data of the concentration-effect relation of levcromakalim were fitted to a logistic equation using Sigmaplot 2.03 for Windows 3.1(25) which determined the range or extent of relaxation (a), the steepness of the curve (slope, b), the concentration of the half-maximal effect(EC50, c) and the minimum of the curve (d, set to 0): equation 1 Other logistic functions(26) gave essentially identical results to the fitting .t test for paired observations (level of significance taken at p ≤ 0.05) was used to assess the effect of glibenclamide, endothelium-removal, L-NMMA and indomethacin in CA and PV. These data are presented as the results obtained from paired tissues (obtained from the same animal) with n indicating the number of tissue pairs obtained from different animals (see Tables 2–5, Fig. 3). The effect of CHH was evaluated with the t test for unpaired observations (level of significance taken at p ≤ 0.05;Fig. 5). The effects of L-NMMA and endothelium-removal in RA were analyzed with t test for paired observations (Figs. 1 and 2). The effects of age in one type of preparation (conduit arteries, resistance-sized arteries or veins) was tested with one way ANOVA (SPSS 6.1 for Windows). If p values (mentioned in the text), indicated a significant difference, a post hoc comparison was carried out on all pairs of data according to the Bonferroni method whereby statistical significance was taken at p ≤ 0.05(Fig. 4). Only significant differences are mentioned in the text. Last, two-way analysis of variance was carried out to evaluate the effects of age and type of vessel on the relaxations induced by levcromakalim. Differences were considered statistically significant if p ≤ 0.05.
Influence of indomethacin (10 μM) on the levcromakalim-induced relaxations in newborn (A, n = 4, paired tissues) and adult (B, n = 6, paired tissues) conduit pulmonary arteries. ○, indomethacin; •, control. In the newborn,Rmax but not ED50 were significantly inhibited by indomethacin (respectively, p = 0.02 and p = 0.16).Rmax and ED50 were significantly inhibited in the adult (respectively, p = 0.003 and p = 0.046).
Effect of chronic hypobaric hypoxia on the responses to levcromakalim in pulmonary vessels from piglets aged 3 d (A, B, and C) or 6 d (D, E, and F), in tissue from control(○) and hypoxic (▪) animals. A, conduit arteries, control n = 10, hypoxic, n = 6; B, resistance-sized arteries, control n = 12, hypoxic n = 4; C, veins, control n = 9, hypoxic n = 5; D, conduit arteries, control n = 7, hypoxic n = 11; E, resistance-sized arteries, control n = 6, hypoxic n = 8; and F, veins, control n = 11, hypoxic n = 12.
Influence of L-NMMA (30 μM) on responses to levcromakalim in pulmonary resistance-sized arteries of 3-d-old animals(A, n = 6) and adult animals (B, n = 6), all with functional endothelium present. Symbols are identical for both panels, •, control; ○, L-NMMA; ▵, L-arginine (1 mM). Both Rmax and ED50 of levcromakalim relaxations were inhibited by L-NMMA(3-d-old, p = 0.032 and p = 0.006, respectively; adult,p = 0.005 and p = 0.01, respectively).
RESULTS
Preliminary Experiments
Specificity of the responses. The specificity of the responses to levcromakalim in newborn and adult conduit pulmonary arteries and veins was checked with glibenclamide (1 μM). Application of glibenclamide before PGF2α application significantly (p < 0.05) attenuated the subsequent responses to levcromakalim in intrapulmonary conduit arteries and veins of the newborn piglet (Table 2). Glibenclamide had similar effects in arteries and veins of adult animals(Table 2). The addition of glibenclamide had no effect on the basal tone of large arteries and veins in either newborn or adult.
Influence of endothelium removal. In a second series of experiments, the influence of the endothelium on the responses to levcromakalim was tested in conduit pulmonary arteries and veins at various ages (Table 3). Removal of the endothelium did not influence the relaxation to levcromakalim in CA from newborn, 3-d-old, 6-7-d old, and adult animals. However, in CA from 14-17-d-old animals, the endothelium contributed to the levcromakalim-induced relaxations, as was evident by a small but significant change in EC50(Table 3). By contrast, endothelium-removal in PV always resulted in a significant rightward shift of the dose-response to levcromakalim. In veins from newborn and adult animals, this attenuation was accompained by a significant reduction of Rmax (a,Table 3). Effects of endothelium-removal on the slope of the concentration-response relation to levcromakalim were never significant except in the case of adult veins. Here, endothelium removal reduced the slope from 2.3 ± 0.3 to 1.6 ± 0.1 (n = 6, p = 0.04).
In RA, endothelium removal in 3-d-old animals resulted in a significant attenuation of the vasodilator properties of levcromakalim (Fig. 1A). Some attenuation of the levcromakalim responses was also observed in RA from adult animals (Fig. 1C), but the difference did not reach the level of statistical significance.
Influence of L-NMMA application. To address further the influence of the endothelium, we assessed the possible contribution of NO and cyclo-oxygenase products to the levcromakalim-induced relaxations.Figure 2 shows that L-NMMA (30 μM) attenuated the relaxation to levcromakalim in RA obtained from 3-d-old and adult animals. In RA, the concentration-effect curve after L-NMMA application almost superimposed with the curve obtained after endothelium removal (compare Fig. 2A and Fig. 1A). Application of L-arginine (1 mM) reversed the attenuated relaxation to levcromakalim in both 3-d-old and adult animals (Fig. 2, A and B). The concentration-response curves to levcromakalim in absence and presence of L-arginine nearly superimposed. L-NMMA had no influence on the relaxation induced in CA (Table 4). L-NMMA partially attenuated the relaxation induced by levcromakalim in the veins by a decrease of the EC50 without influencing the maximal relaxation obtained by levcromakalim. This response was seen in veins at all ages except in the newborn (Table 4). Thus, in the veins L-NMMA application mimicked the effect of endothelium removal on EC50 but not on Rmax.
Influence of indomethacin. In CA from newborn animals, indomethacin significantly inhibited the relaxant responses to levcromakalim (Fig. 3). The effect only persisted until the age of 3 d(results not shown). At the ages of 6 and 17 d, we could not observe an inhibitory effect of indomethacin on the relaxant response (results not shown). In the adult, the inhibitory effect of indomethacin on the levcromakalim-induced relaxations reappeared to a small but significant extent (Fig. 3). Denudation of the endothelium resulted in the disappearance of the small attenuation observed after application of indomethacin in intact adult CA (results not shown).
In PV, indomethacin had no effect on levcromakalim-induced relaxations in newborn, 3-d-old and adult vessels. At the ages of 6 and 14-17 d, indomethacin inhibited the relaxations slightly but significantly by reducing the sensitivity and the maximal relaxation respectively (Table 5).
Responses to Levcromakalim during Development
Figure 4 shows the response to levcromakalim in CA, RA, and PV at different ages, all with endothelium. In CA, one-way analysis of variance followed by Bonferroni post hoc testing indicated that both the EC50 values and the extent of maximum relaxation elicited by levcromakalim changed significantly with age (p = 0.0003 for both variables). Post hoc testing indicated that significant differences in maximal relaxation existed between newborn and adult animals, between newborn and 17-d-old animals, and between 6-d-old and adult animals. The EC50 values also differed significantly between newborn and adult, between newborn and 17-d-old animals, and between 3-d-old and adult animals.Figure 4A indicates an increase in sensitivity and extent of relaxation in CA between 6 and 17 d of age. For the resistance-sized arteries, statistical analysis failed to demonstrate any significant difference with age, either for the maximal relaxation (p = 0.81), or for the EC50 values (p = 0.32, Fig. 4B). For the veins, statistical analysis revealed that age had a significant influence on maximal relaxation (p = 0.004) but not on EC50 values (p = 0.12). Post hoc testing showed that maximal relaxation in the veins was significantly smaller in 3-d-old and newborn animals when compared with 6-d-old animals. Figure 4C indicates that the relaxation induced by levcromakalim was maximal by 6 d, after which there was no significant change.
The maximum relaxation and the EC50 values of the response to levcromakalim appeared to differ according to the type of intrapulmonary vessel (Fig. 4, A-C). Two-way analysis of variance showed that both the type of intrapulmonary vessel and the age of the animal had a significant influence on the EC50 value (p = 0.0001 and 0.03, respectively). A significant interaction also existed between age and type of preparation for the EC50 values (p = 0.003). Thus the overall sensitivity differences between the pulmonary vessels (large arteries > veins ≅ resistance arteries) depended on age. It can be seen in Figure 4, A-C, that smaller differences were present in the newborn than in the adult. Similarly, two-way analysis of variance showed that Rmax was influenced by the type of intrapulmonary vessel(large arteries < resistance arteries ≅ veins) and age (p = 0.001 and 0.003, respectively). In addition, there existed again a significant interaction between age and type of preparation for the parameter of maximal relaxation (p = 0.014). The difference of Rmax between the different vessel types was larger in newborn than adult animals.
Response to Levcromakalim after Exposure to Chronic Hypobaric Hypoxia
Irrespective of the age at which newborn animals were exposed to CHH, the vessels still relaxed in response to levcromakalim (Fig. 5). The responses were normal and similar in CA and PV taken from animals exposed to hypoxia from birth (Fig. 5, A and C) and those exposed from 3 to 6 d of age (Fig. 5, D and F). The slight shift of the concentration-response curve in Figure 5F was not statistically significant. In contrast, the response of the RA to levcromakalim varied with CHH: EC50, but not Rmax, was significantly enhanced in animals exposed to hypoxia from birth(Fig. 5B, p = 0.026) and in those exposed from 3 to 6 d of age (Fig. 5E, p = 0.006). To delimit more exactly the size of vessels which were influenced by CHH in their ability to react to levcromakalim, additional studies were carried out in 6 d old control and hypoxic animals. Distal muscular arteries from control animals(n = 6) were studied in a myograph and subjected to the same mounting and conditioning protocol as described in “Methods” for the small vessels (diameter in vitro after stretch, 804 ± 102μm). Levcromakalim-induced relaxations in these distal muscular arteries were characterized by an ED50 and Rmax of 6.58± 0.17 and 60 ± 3%, respectively. After CHH, the relaxations in this type of preparation were not altered (6.61 ± 0.05 and 61 ± 5%, respectively, n = 6, diameter 915 ± 119 μm).
DISCUSSION
Evidence has accumulated that vasoconstrictor and vasodilator reactivity in the newborn pulmonary vascular bed is different from that in the adult(2–4, 10, 27). In comparison with the adult pulmonary circulation, it appears that the range and potency of vasodilator mechanisms available to the newborn pulmonary artery are considerably restricted. The relaxant pathways dependent on the intracellular generation of cGMP(28) appear to be underdeveloped. This is evident from the reduced relaxant responses to sodium nitroprusside and exogenous application of nitric oxide gas(2, 10). Endothelium-derived NO as a major stimulus for pulmonary smooth muscle intracellular cGMP generation appears to be less functional in the newborn when compared with effects in older animals(2, 3, 10). Alternative pathways for relaxing pulmonary vascular smooth muscle(29) include, among others, the generation of intracellular cAMP(30) or hyperpolarization through K+ channels(31).
In the present study the K(ATP)+ channel agonist levcromakalim-induced relaxations in all segments of the pulmonary vascular bed at birth. In the adult pulmonary and systemic circulations, potassium channels appear to help regulate vascular smooth muscle tone(5, 6) and K(ATP)+ channel activation helps regulate the resting potential in adult isolated pulmonary arterial cells(32). Administration of glibenclamide causes a slow increase in the perfusion pressure of isolated newborn porcine lungs(33). The failure of glibenclamide to increase the basal tension in the present study would seem to be at odds with the observation made in vivo. The findings in the present study indicate that the increase in tone in the isolated lung may have developed in preacinar or acinar pulmonary vessels or in small veins, but the small size of these vessels excludes in vitro experimentation. In the present study levcromakalim appeared to act as a specific K(ATP)+ channel agonist, causing relaxation of PGF2α-precontracted porcine conduit arteries, resistance arteries, and veins, a response that was attenuated by glibenclamide at a dose of 1 μM. The potency and sensitivity of levcromakalim in the conduit porcine intrapulmonary arteries of adult animals was similar to that seen in adult rat pulmonary arteries, both vessels being precontracted with PGF2α(34). The sensitivity and potency of cromakalim in the spontaneously contracting portal vein were larger than in the present study, whereas the relaxant effect of cromakalim on the methoxamine contracted aorta and its inhibition by glibenclamide was similar to that reported in the present study(35). Thus the response to K(ATP)+ channel activation in our preparation appears to be largely similar to that reported by other investigators.
The response to levcromakalim in vessels precontracted with PGF2α increased in CA to a small but statistically significant extent during the course of adaptation to extrauterine life and subsequent growth. The response of RA did not change with age, whereas the veins showed an increase in maximal relaxation between birth and 6 d. The times at which K(ATP)+ channel activity was investigated were those at which structural and functional changes had been shown to occur most rapidly in the porcine lung(8, 9, 36, 37). Pulmonary arterial pressure and vascular resistance fall rapidly between the first few minutes of life and 3 d. Adaptation is largely complete by the 14th d of life. We found that K(ATP)+ channel activation caused almost as great a relaxation in newborn as in adult vessels, in marked contrast to the gradual maturation of the NO pathway that takes several days(4, 10). In general, the postnatal maturation of K(ATP)+ channels has not been well studied, but our findings in large porcine pulmonary arteries are similar to those in the ovine cerebral circulation, where the sensitivity, but not maximal response, to levcromakalim increases with age(38). At all ages the relaxant response to levcromakalim was greater in RA than in CA, and the response in PV was similar to that in RA. These findings raise the possibility that K(ATP)+ channel activation may be important in instigating or maintaining vasodilatation at birth. Levcromakalim also caused marked relaxation of the pulmonary veins, and these vessels are thought to contribute to pulmonary vascular resistance in the fetal and newborn lung(12, 13).
At birth and in the adult lung the K(ATP)+ channels in the CA appeared to be confined to the smooth muscle cells as endothelial removal and exposure to L-NMMA had no effect on levcromakalim-induced relaxation. The endothelium appeared to have a small effect at 14-17 d of age. In contrast, in RA endothelium removal attenuated relaxations at 3 d by increasing EC50 and decreasing Rmax. Studies with L-NMMA confirmed that release of NO was indeed responsible for the increased sensitivity to levcromakalim observed in RA with an intact endothelium. K+ channels have been demonstrated on endothelial cells in vitro(15–17), and K+ channel stimulation in the ovine fetal pulmonary circulation causes endothelium-dependent (NO) relaxation(18). How K(ATP)+ channel stimulation causes NO release is not known, and it is possible that other relaxant factor(s), such as endothelium-derived hyperpolarizing factor, may be activated or released. A continuous basal synthesis of NO might facilitate the actions of levcromakalim(19). Recent work shows that the addition of L-NMMA increased the basal tone in newborn porcine RA (P. J. Boels, unpublished results). In the present study L-NMMA also attenuated the relaxation of adult RA, an attenuation reversed by L-arginine, as in the 3-d-old animals. Unlike in the RA obtained from 3-d-old animals, it proved not to be possible to mimic the effects of L-NMMA on levcromakalim-induced relaxations by the removal of the endothelium in adult RA. These results imply other sources of NO than the endothelium and a more complex relation between NO, K(ATP)+ channels and vasodilatation in the adult as compared with the newborn. This is currently further investigated.
In PV, endothelium removal attenuated levcromakalim-induced relaxation at all ages, as shown by the increase in EC50 and also by a decrease in Rmax in the newborn and adult. Unlike the RA, however, L-NMMA only attenuated the levcromakalim response in older animals by increasing the EC50, without decreasing Rmax. Cyclo-oxygenase inhibition with indomethacin had no effect on levcromakalim-induced relaxation at birth, at 3 d of age, or in the adult. These findings suggest that the endothelium dependence of levcromakalim-induced relaxation in newborn pulmonary veins may not depend primarily on either NO or on an endothelium-derived prostanoid relaxing factor. Like newborn porcine veins, ovine veins show endothelium-dependent relaxation during late fetal life and the first days of postnatal life(14, 39, 40) as did the newborn porcine veins in vitro in the present study.
Cyclo-oxygenase inhibition by indomethacin had a marked effect on the CA of newborn and 3-d-old vessels, although removal of the endothelium had no effect. This suggests the presence of a cyclo-oxygenase in these conduit arterial smooth muscle cells, leading to the synthesis of vasodilator prostaglandins, prostaglandin I2 and/or prostaglandin E(29, 41), which may facilitate the actions of levcromakalim. Active cyclo-oxygenase-1 has been demonstrated in the smooth muscle of ovine pulmonary arteries(42). Alternatively, the addition of levcromakalim might have stimulated the synthesis of vasodilator prostaglandins, although there is currently no evidence for this conjecture in the literature. These results indicate that routine inclusion of indomethacin in PSS for in vitro organ bath experiments(2–4, 10) could leave additional mechanisms of relaxations undetected.
We found that not only was K(ATP)+ channel activated relaxation present at birth but that in all segments of the porcine pulmonary vasculature it appeared to be resistant to chronic hypobaric hypoxia. Chronic hypoxia is a major cause of persistent pulmonary hypertension in the human infant. The effect of hypoxia on the smooth muscle of isolated adult pulmonary arteries resembles the effects of K+ channel blockers and drugs that block the K+ channels also potentiate the vasoconstrictor response to hypoxia(43). Acute hypoxia can suppress K+ channels in isolated pulmonary arterial smooth muscle cells(44, 45). The individual potassium channels that could be responsive to hypoxia and their gating mechanisms have not been defined. However, in systemic arteries, hypoxia causes an increase in current through ATP-dependent potassium channels and vasodilatation, whereas in the pulmonary arteries, hypoxia inhibits potassium current and causes vasoconstriction(46). In the present study, after exposure to CHH, the relaxant response to the K(ATP)+ channel agonist levcromakalim in large conduit pulmonary arteries and veins was preserved. The resistance arteries showed a significant increase in sensitivity to levcromakalim. Rodman(47) described augmentation of levcromakalim-induced relaxation in the isolated main branch pulmonary arteries of chronic hypoxic rat lungs. Similarly, Wanstall and O'Donell(48) reported that pinacidil-induced relaxation was increased in main pulmonary arteries of pulmonary hypertensive adult Wistar rats. But unlike pig and man, the extrapulmonary artery and intralobar conduit pulmonary arteries of the rat are muscular, not elastic, in structure. They are comparable in size and structure to vessels located more peripherally in the porcine and human lung. These observations highlight the possibility that during CHH in the porcine lung, only small muscular arteries are subjected to an up-regulated K(ATP)+ channel-dependent vasodilatation, whereas larger muscular and elastic arteries remain unaffected. Our study confirmed that up-regulation does only occur in arteries with diameters <0.8-0.9 mm. Struijker-Boudier et al.(49) noted that in systemic hypertension, levcromakalim preferentially relaxed the resistance arteries in rats. Thus, in both pulmonary and systemic hypertension the smaller resistance-sized arteries became more sensitive to K(ATP)+ channel activation.
This study has demonstrated that K(ATP)+ channel activation causes relaxation in all segments of the pulmonary vasculature at birth, to almost as great an extent as in the adult. Age-dependent heterogeneity in the way the response to K(ATP)+ channel activation is modulated by vasoactive substances from the endothelium is seen in the conduit arteries, resistance arteries and veins of both the normal and chronic hypoxic newborn lung. After exposure to CHH, the persistence of the relaxant response to K(ATP)+ channel activation in the newborn vasculature is in marked contrast to the attenuation of endothelium-dependent and independent relaxation mediated by nitric oxide(10). The presence of cromakalim-sensitive K(ATP)+ channels in the humman vasculature is implicated in one study(50) on adult patients with angina pectoris. No information on the presence and functional significance of these channels in human newborns is presently available. Our findings indicate a possible alternative relaxant pathway which might be amenable to therapeutic manipulation.

Abbreviations
- ACH:
-
acetylcholine
- CA:
-
intrapulmonary conduit arteries
- CHH:
-
chronic hypobaric hypoxia
- EC50:
-
concentration required to obtain half maximal relaxation
- K(ATP)+:
-
ATP-dependent K+ channel
- L-NMMA:
-
NG-monomethyl-L-arginine
- NO:
-
nitric oxide
- PGF2α:
-
prostaglandin F2α
- PSS:
-
physiologic salt solution
- PV:
-
intrapulmonary veins
- RA:
-
pulmonary resistance-sized arteries
- R max :
-
maximal extent of relaxation
References
Abman SH, Chatfield BA, Hall SL, McMurtry IF 1990 Role of endothelium-derived relaxing factor during transition of pulmonary circulation at birth. Am J Physiol 259:H1921–H1927.
Liu SF, Hislop AA, Haworth SG, Barnes PJ 1992 Developmental changes in endothelium-dependent pulmonary vasodilatation in pigs. Br J Pharmacol 106: 324–330.
Zellers TM, Vanhoutte PM 1991 Endothelium-dependent relaxations of piglet pulmonary arteries with maturation. Pediatr Res 30: 176–180.
Wilson LE, Levy M, Stuart-Smith K, Haworth SG 1993 Postnatal adrenoreceptor maturation in porcine intrapulmonary arteries. Pediatr Res 34: 591–595.
Standen NB, Quayle JM, Davies NW, Brayden JE, Huang Y, Nelson MR 1989 Hyperpolarizing vasodilators activate ATP-sensitive K+ channels in arterila smooth muscle. Science 245: 177–180.
Nichols C, Lederer W 1991 Adenosine triphosphate-sensitive potassium channels in the cardiovascular system. Am J Physiol 261:H1675–H1686.
Weston AH, Edwards G 1991 Latest development in K-channel modulator pharmacology. Z Kardiol 80( Suppl 7): 1–9.
Haworth SG, Hislop AA 1982 Effect of hypoxia on adaptation of the pulmonary circulation to extra-uterine life in the pig. Cardiovasc Res 16: 293–303.
Allen KM, Haworth SG 1986 Impaired adaptation of pulmonary circulation to extrauterine life in newborn pigs exposed to hypoxia: an ultrastructural study. J Pathol 150: 205–212.
Tulloh RMR, Hislop AA, Boels PJ, Deutsch J, Haworth SG 1997 Chronic hypoxia inhibits postnatal maturation of porcine intrapulmonary artery relaxation. Am J Physiol 272:H2436–H2445.
Haworth SG 1993 Pulmonary hypertension in childhood. Eur Respir J 6: 1037–1043.
Tod ML, Yoshimura K, Rubin LJ 1992 Ontogeny of neonatal pulmonary vascular pressure-flow relationships. Am J Physiol 262:H684–H690.
Tod ML, Sylvester JT 1989 Distribution of pulmonary vascular pressure as a function of perinatal age in lambs. J Appl Physiol 66: 79–87.
Gordon JB, Tod ML 1993 Effects of N omega-nitro-L-arginine on total and segmental vascular resistances in developing lamb lungs. J Appl Physiol 75: 76–85.
Olesen SP, Clapham DE, Davies PF 1988 Haemodynamic shear stress activates a K+ current in vascular endothelial cells. Nature 331: 168–170.
Bregestovski PD, Ryan US 1989 Voltage-gated and receptor-mediated ionic currents in the membrane of endothelial cells. J Mol Cell Cardiol 21( Suppl 1): 103–108.
Hutcheson IR, Griffith TM 1994 Heterogeneous populations of K+ channels mediate EDRF release to flow but not agonists in rabbit aorta. Am J Physiol 266:H590–H596.
Chang JK, Moore P, Fineman JR, Soifer SJ, Heyman MA 1992 K+ channel pulmonary vasodilation in fetal lambs: role of endothelium-derived nitric oxide. J Appl Physiol 73: 188–194.
Miyoshi H, Nakaya Y, Moritoki H 1994 Nonendothelial-derived nitric oxide activates the ATP-sensitive K+ channel of vascular smooth muscle cells. FEBS Lett 345: 47–49.
Boels PJ, Claes VA, Brutsaert DL 1990 Mechanics of K(+)-induced isotonic and isometric contractions in isolated canine coronary microarteries. Am J Physiol 258:C512–C523.
Levy M, Tulloh RM, Komai H, Stuart-Smith K, Haworth SG 1995 Maturation of the contractile response and its endothelial modulation in newborn porcine intrapulmonary arteries. Pediatr Res 38: 25–29.
Belik J 1994 Large pulmonary arteries and the control of pulmonary vascular resistance in the newborn. Can J Physiol Pharmacol 72: 1464–1468.
Mulvany MJ, Halpern W 1977 Contractile properties of small arterial resistance vessels in spontaneously hypertensive and normotensive rats. Circ Res 41: 19–26.
Leach RM, Twort CH, Cameron IR, Ward JP 1989 A comparison of contractile function in large and small pulmonary arterial vessels of the rat. Q J Exp Physiol 74: 947–950.
Anonymous 1994 Sigmaplot Transforms and Curve Fitting. Jandel Scientific Software, San Rafael, CA, pp 9.8–9.18.
Kenakin T. 1993 Pharmacological analysis of drug-receptor interaction. In: Analysis of Dose-Response Data. Raven Press. New York, pp 176–220.
Perreault T, De Marte J 1993 Maturational changes in endothelium-derived relaxations in newborn piglet pulmonary circulation. Am J Physiol 264:H302–H309.
Lincoln TM, Komalavilas P, Cornwell TL 1994 Pleiotropic regulation of vascular smooth muscle tone by cyclic GMP-dependent protein kinase. Hypertension 23: 1141–1147.
Barnes PJ, Liu SF 1995 Regulation of pulmonary vascular tone. Pharmacol Rev 47: 87–131.
McDaniel NL, Rembold CM, Murphy RA 1994 Cyclic nucleotide dependent relaxation in vascular smooth muscle. Can J Physiol Pharmacol 72: 1380–1385.
Kozlowski RZ 1995 Ion channels, oxygen sensation and signal transduction in pulmonary arterial smooth muscle. Cardiovasc Res 30: 318–325.
Clapp LH, Gurney AM 1992 ATP-sensitive K+ channels regulate resting potential of pulmonary arterial smooth muscle cells. Am J Physiol 262:H916–H920.
Pinheiro JM, Malik AB 1992 K+ ATP-channel activation causes marked vasodilation in the hypertensive neonatal pig lung. Am J Physiol 263:H1532–H1536.
Ward JPT, Chappell LC, Leach RM 1991 Effects of BRL38227 and glibenclamide on small pulmonary arteries of the rat. In: Mulvany MJ, Alkjaer C, Heagerty AM, Nyborg NCB, Strandgaard S (eds) Resistance Arteries: Structure and Function. Excerpta Medica International Congress Series, pp 139–143.
Winquist RJ, Heaney LA, Wallace AA, Baskin EP, Stein RB, Garcia ML, Kaczorowski GJ 1989 Glyburide blocks the relaxation response to BRL 34915 (cromakalim), minoxidil sulfate and diazoxide in vascular smooth muscle. J Pharmacol Exp Ther 248: 149–156.
Haworth SG, Hislop AA 1981 Adaptation of the pulmonary circulation to extrauterine life in the pig and its relevance to the human infant. Cardiovasc Res 15: 108–119.
Haworth SG, Hall SM, Chew M, Allen K 1987 Thinning of fetal pulmonary arterial wall and postnatal remodelling: ultrastructural studies on the respiratory unit arteries of the pig. Virchows Arch A Pathol Anat Histopathol 411: 161–171.
Pearce WJ, Elliott SR 1994 Maturation enhances the sensitivity of ovine cerebral arteries to the ATP-sensitive potassium channel activator lemakalim. Pediatr Res 35: 729–732.
Steinhorn RH, Morin FC, Gugino SF, Giese EC, Russell JA 1993 Developmental differences in endothelium-dependent responses in isolated ovine pulmonary arteries and veins. Am J Physiol 264:H2162–H2167.
Gao Y, Zhou H, Usha-Raj J 1995 Endothelium-derived nitric oxide plays a larger role in pulmonary veins than in arteries of newborn lambs. Circ Res 76: 559–565.
Schror K 1993 The effect of prostaglandins and thromboxane A2 on coronary vesseltone-mechanisms of action and therapeutic implications. Eur Heart J 14( suppl 1): 34–41.
Brannon TS, North AJ, Wells LB, Shaul PW 1994 Prostacyclin synthesis in ovine pulmonary artery is developmentally regulated by changes in cyclooxygenase-1 gene expression. J Clin Invest 93: 2230–2235.
Hasunuma K, Rodman DM, McMurtry IF 1991 Effects of K+ channel blockers on vascular tone in the perfused rat lung. Am Rev Respir Dis 144: 884–887.
Post JM, Hume JR, Archer SL, Weir EK 1992 Direct role for potassium channel inhibition in hypoxic pulmonary vasoconstriction. Am J Physiol 262:C882–C890.
Yuan XJ, Goldman WF, Tod ML, Rubin LJ, Blaustein MP 1993 Hypoxia reduces potassium currents in cultured rat pulmonary but not mesenteric arterial myocytes. Am J Physiol 264:L116–L123.
Weir EK, Archer SL 1995 The mechanism of acute hypoxic vasoconstriction: the tale of two channels. FASEB J 9: 183–189.
Rodman DM 1992 Chronic hypoxia selectively augments rat pulmonary artery Ca2+ and K+ channel-mediated relaxation. Am J Physiol 263:L88–L94.
Wanstall JC, O'Donnell SR 1992 Responses to vasodilator drugs on pulmonary artery preparations from pulmonary hypertensive rats. Br J Pharmacol 105: 152–158.
Struijker-Boudier HA, Messing MW, Van-Essen H 1992 Preferential small arteriolar vasodilatation by the potassium channel opener, BRL38227 in conscious spontaneously hypertensive rats. Eur J Pharmacol 18: 191–193.
Thomas P, Dixon MS, Winterton SJ, Sheridan DJ 1990 Acute haemodynamic effects of cromakalim in patients with angina pectoris. Br J Clin Pharmacol 29: 325–331.
Acknowledgements
The authors thank Sue Hodgson for expert secretarial assistance and Dr. Alison Hislop for pertinent discussions.
Author information
Authors and Affiliations
Additional information
Supported by the British Heart Foundation.
Rights and permissions
About this article
Cite this article
Boels, P., Gao, B., Deutsch, J. et al. ATP-Dependent K+ Channel Activation in Isolated Normal and Hypertensive Newborn and Adult Porcine Pulmonary Vessels. Pediatr Res 42, 317–326 (1997). https://doi.org/10.1203/00006450-199709000-00012
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199709000-00012