Abstract
Using spectral analysis we have studied changes in the heart rate during periodic thermal stimulation of one foot of infants during quiet sleep. Twenty-two appropriately grown preterm infants were studied in the first 15 d after birth to quantify responses in comparison with previously reported term infants. Babies were stimulated at 0.05, 0.10, and 0.15 Hz. Spectral power was calculated at the stimulus frequency ±0.01 Hz and ±0.02 Hz and over the low frequency range 0.03 Hz to 0.17 Hz. The data show that 1) there is an increase in power around the frequency of stimulation for each frequency studied (p < 0.002); and 2) there is an increase in the ratio of local to low frequency power at 0.05 Hz(p = 0.002) and 0.10 Hz (p = 0.001), but not at 0.15 Hz(p = 0.109). These data confirm the concept of entrainment in the appropriately grown preterm infant but demonstrate that it occurs over a wider frequency range than previously reported. The wider range is the same as that of the term infant, although there are differences in the patterns of entrainment between the two groups. Further work is required to map out the maturation of the autonomic nervous system in both the term and the preterm infant with respect to the low frequency components of the heart rate variability power spectrum.
Similar content being viewed by others
Main
The beat to beat change in the heart rate of the newborn infant is modulated by a variety of influences such as respiration, vasomotion, and thermoregulation. The culmination of these interacting body systems is the continually changing interbeat interval of the heart rate-the so-called heart rate variability. Breathing induces changes in the heart rate at the rate of breathing (high frequency). It has also been shown that breathing induces changes at lower frequencies in the range of 0.05 to 0.15 Hz(1–3). These lower frequency changes are thought to be related to vasomotor, thermoregulator, and baroreceptor activity(4). These responses are markedly affected by the sleep state of the infant(3, 5).
Application of a periodic stimulus can produce entrainment of the heart rate variability at the frequency of stimulation(6–8). Lindqvist and his co-workers(6) applied a periodic thermal stimulus to one foot in newborn infants of various gestations to assess the degree of entrainment. In preterm infants weighing >1000 g, they showed that the heart rate can be entrained and suggested it is maximal at 0.083 or 0.10 Hz. Further work from the same laboratory supported these results with a fixed stimulus at 0.083 Hz(9). We have subsequently reported that the heart rate can be entrained in the term infant over the frequency range of 0.05-0.15 Hz, a wider range of frequencies than had been previously shown, and that no single frequency appears to be more powerful than another(10).
We have now studied overall heart rate variability in a group of appropriately grown preterm infants over the same frequency range to compare the responses with those in the term infant. This is part of an ongoing longitudinal study of the concept of entrainment of the heart rate as a measure of autonomic nervous system maturation.
METHODS
Subjects. Twenty-two appropriately grown (>10th centile, Gairdner and Pearson charts) preterm infants of gestational ages 29-36 wk were studied within 15 d after delivery. Studies were performed once the infants were stable and spontaneously breathing room air. None was known to have cerebral pathology. Postconceptional age at the time of study ranged from 31 to 36 wk. All studies were performed in the neonatal intensive care unit of the Homerton Hospital. Research Ethics Committee approval was granted for the study, and written informed consent was given by the parents. Fifteen of the mothers chose to be present during the studies, which were performed mid morning after a feed. The babies lay supine in a cot, wearing a“baby-grow” and covered with a light blanket The room temperature was maintained at 27-29 °C. Only the infant's left foot was exposed, and at all times it was pink and warm to the touch. Details of the infants are shown in Table 1. All studies were performed with the babies in quiet sleep, which was determined by trained observers (P.A.M., D.P.I.) using the criteria of Prechtl and Beintema(11).
Recordings. The methods used for data acquisition and analysis in this study were the same as those detailed in our previous report(10). In summary, the ECG and abdominal breathing movements were recorded. Warm air was supplied by an adapted hair dryer directed via tubing onto the infant's exposed foot. The temperature of the air stream was measured by a rapidly responding thermistor. The heater was controlled by an accurate quartz clock providing periods of warming and cooling of equal duration. The infants were stimulated at 0.10 Hz as the central stimulating frequency and at 0.05 and 0.15 Hz, which were the extremes of entrainment in our previous study.
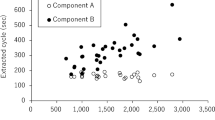
Analysis. Data were recorded onto a frequency modulated cassette recorder (TEAC) and digitized using a Cambridge Electronic Design system (Cambridge, UK). This incorporates a 16-bit analog-to-digital converter with a 1-MHz internal frequency source. The ECG was digitized at 1000 Hz and the breathing and thermistor data at 100 Hz. The algorithm of Okada(12) with a resolution of 1 ms was used to detect successive R waves in the ECG, and these were used to calculate instantaneous heart rates sampled at 10 Hz(3). Programs were written to determine the onset of each breath and then a 5-s moving window(13) was used from these onsets to determine at 10 Hz the instantaneous breathing rates. The temperature data from the thermistor was decimated from 100 to 10 Hz. Figure 1 shows raw data from part of the tracing from baby 589.
Example of part of original data from baby 589. All channels are in volts. channel 1, ECG; channel 2, abdominal breathing movements; Channel 3, thermistor temperature(inverted, i.e. increasing temperature is downward). Vertical lines indicate end of stimulation at 0.05 Hz and start of stimulation at 0.15 Hz.
Two minutes of stable data containing no artifacts due to movements or sighs were used for the analysis of each section of control and stimulus data. The data were detrended using a least-squares method, and a cosine taper was applied to each end of the data. Auto- and cross-spectral analyses(14) were performed on the data sets, and the power spectra for the 120-s sections of stable data were evaluated from 0.01 to 1.0 Hz at a resolution of 0.01 Hz.
Statistical methods. The distribution-free Wilcoxon matched-pairs signed-ranks test was used for comparison of related samples. A probability of 0.05 or less was considered significant, and the null hypothesis was rejected. Multiple regression of a dependent variable against a number of independent variables was performed using the Stata statistical package.
RESULTS
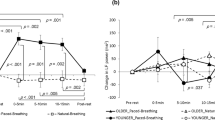
Figure 2 shows the instantaneous heart rates from baby 555 for a 120-s control period and a 120-s period with a repetitive thermal stimulus applied to one foot at 0.10 Hz. The lower graphs are the corresponding power spectra. It can be seen that, in the control spectrum, with the temperature in the air stream constant, there is a spread of low frequency power from 0.03 to 0.20 Hz and a high frequency peak at 0.55 to 0.80 Hz. After the application of a periodic thermal stimulus at 0.10 Hz, with the air stream warming and cooling for equal periods of time, the power spectrum shows a concentration of the low frequency power around the frequency of stimulation resulting in a prominent local peak.
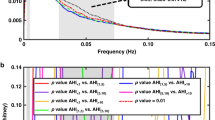
To be able to compare and quantify the response in our babies to periodic thermal stimuli of varying frequencies, the total power over a number of frequency ranges was measured for each baby for each control and stimulus period. Comparison of the values for power over these different frequency ranges for the control and the stimulus periods afforded us a measure of entrainment for each baby at each frequency of periodic stimulation. The frequency ranges over which we calculated power are shown in Figure 3.
The same methods used in our previous study on term infants(10) were used to assess the effect of a periodic thermal stimulus on the heart rate spectrum compared with the control period:1) the actual power immediately around the stimulus frequency f (area A in Fig. 3, i.e. f± 0.01 Hz); 2) the presence of a local peak of power at the stimulus frequency f (the ratio of A to B in Fig. 3, i.e. f ± 0.01/f± 0.02 Hz); 3) the proportion of power at the stimulus frequency in proportion to the total low frequency power (the ratio of A to C in Fig. 3). We have defined the low frequency region as 0.03 to 0.17 Hz as this range is ±0.02 Hz of the extremes of our range of stimulation.
The results in Table 2 show an increase in power at the frequency of stimulation (area A in Fig. 3) and in the ratio of local power to total low frequency power (area A: area C in Fig. 3) at each of the frequencies used. These increases are significant at 0.05 and 0.10 Hz but not at 0.15 Hz. However, the presence of a local peak around the frequency of stimulation (area A:area B in Fig. 3) shows a highly significant increase in power at each of the three frequencies studied. These results strongly support the concept of entrainment to a repetitive thermal stimulus in the appropriately grown preterm infant.
Multiple regression showed that the response in heart rate to thermal stimulation was not affected by gestational age, postnatal age, sex, mode of delivery, or birth weight.
DISCUSSION
We have shown that the low frequency oscillations in heart rate in the appropriately grown preterm infant are entrained by the application of a periodic thermal stimulus over the frequency range of 0.05 to 0.15 Hz. This range is wider than other studies in the preterm infant have suggested(6) and is the same range over which we found entrainment in the appropriately grown term infants(10).
The presence of a local peak (ratio of A to B) was confirmed in the preterm infants at all three frequencies, as was the greater proportion of stimulus power over low frequency power (ratio of A to C). The preterm infants differed from the term infants in that the absolute power at the frequency of stimulation (A) was not significantly increased at 0.15 Hz. This could be because the preterm infants do show a smaller response at this frequency. However, it may be because the amplitude of the stimulus at 0.15 Hz (±2 °C) is less than that at 0.10 and 0.05 Hz, as shown in Figure 1, and does not provide an adequate stimulus to produce a significant change in the power. This could be tested by using a system which provides a constant temperature change at differing frequencies of stimulation as has been described by Välimäki and his colleagues(9).
Heart rate variability. Much has been written about the analysis of heart rate and the best measure of the heart rate variability. de Boer et al.(15) concluded that the instantaneous heart rate signal may be considered as the most appropriate method to approximate the neural influences on the cardiac pacemaker. This instantaneous rate is derived from the actual interval in question and prevents a lag effect due to the use of the previous interbeat interval. We have, therefore, chosen to use the instantaneous heart rate for spectral analysis in these studies.
Stability of data. Spectral analysis requires the presence of stable data. We have found that these babies tend to make a sigh on average every 2-4 min. This is in keeping with the work by Prechtl(16). As a consequence we have limited ourselves to analysis of data sets of 120-s duration. By selecting 2-min epochs we have been able to produce power spectra for periods of stable data.
Sleep states in infants. Prechtl(16) performed multiple sequential studies on babies at various gestations to determine when the various components of the sleep-wake cycle become synchronized, as is seen in the term infant. Theirs and other studies suggest that it is only at around 36 wk gestation that sleeping patterns becomes at all ordered(17). The literature suggests that it is not so much the different levels of sleep state that vary with gestational age, but the duration of time spent within each of these sleep states in any sleep-wake cycle. Patterns of breathing are inextricably linked to sleep states, and studies such as these require steady breathing patterns for stable data acquisition and analysis as outlined earlier. We have presented data from 22 appropriately grown preterm infants who remained in a quiet sleep state,i.e. with no eye or body movements and a regular breathing pattern, long enough to allow us to analyze a stable power spectrum of the heart rate variability over 120 s. There were, however, other appropriately grown preterm babies in whom we were unable to analyze stable power spectra for heart rate variability because they did not remain in quiet sleep for at least 2 min at a time. It may be that this second group of babies are functionally less mature than the group from whom the data are presented and that the development of sleep states is more than just a function of the gestational age of the baby but also a marker of nervous system maturation.
Comparison with previous studies. Lindqvist and his colleagues studied thermal entrainment of heart rate in a group of babies after adaptation to extrauterine life. Within their study group there were six appropriately grown preterm infants. They concluded that the preterm infant did entrain to a periodic thermal stimulus but only at 0.083 or 0.10 Hz(6). Our own work in the term infant(10) had clearly shown the phenomenon of entrainment to a wider range of frequencies. The present study demonstrates entrainment of heart rate over this same frequency range in a group of appropriately grown preterm infants.
Our study differs from earlier studies in the preterm infant in two important ways. Lindqvist et al.(6) studied data sets of 700 R-R intervals, whereas our data sets are of 120 s. Our experiences confirmed that of Prechtl(16) that these babies produces sighs every few minutes. Such sighs induce changes in the heart rate by producing damped oscillations in the breathing pattern for a short time after the sigh(18), and hence the power spectrum will be affected. Our data sets, being shorter, do not include periods containing sighs, and therefore there is no influence upon respiratory sinus arrhythmia. Secondly, Jahnukainen et al.(9) applied a low pass filter to their data that may have reduced the high frequency components in the heart rate spectrum because a reduction in the apparent respiratory sinus arrhythmia.
The presence of respiratory sinus arrhythmia is of importance in the assessment of heart rate variability. It produces a peak in the heart rate spectrum at the frequency of breathing(1, 3). However, the sleep state of the infant is also of importance as in rapid eye movement sleep the breathing patterns are not stable and little activity is found in the spectrum. In the preterm infant sleep states are poorly synchronized and the overall respiratory rates are increased in comparison with the term infant. We have previously demonstrated a reduction in the power of the respiratory sinus arrhythmia in the spectrum of the term infant receiving a repetitive thermal stimulus. In this group of babies, respiratory sinus arrhythmia power was less marked and more variable than in the term infants. We did not show a consistent change during thermal stimulation, although as Figure 2 shows, there was a marked reduction in the respiratory sinus arrhythmia power with stimulation in some babies. There was no significant change in mean heart rate during thermal stimulation.
We were unable to demonstrate an attenuation of the response between the first and second minutes of stimulation in these preterm infants. This contrasted with the significant attenuation found in the term infants(10). This may be a reflection of the inability of the developing infant to habituate as readily as the term infant to perturbations within their immediate environment.
CONCLUSIONS
We have studied the effect of a periodic thermal stimulus on the heart rate variability in a group of 22 appropriately grown preterm infants. The babies were stimulated at 0.05, 0.10, and 0.15 Hz. We have shown that a local peak of power is produced in the power spectra of the heart rate variability for all frequencies of stimulation which is the same as in the appropriately grown term infant.
We suggest that the autonomic control of the heart rate is more mature in these infants than had been previously demonstrated as evidenced by the entrainment pattern which they show to a periodic thermal stimulus. Further work is required to map out the maturation of the autonomic nervous system in both the term and the preterm infant and further dissection is needed of what is contributing to the low frequency components of the power spectrum of heart rate variability.
References
Finley JP, Nugent ST 1983 Periodicities in respiration and heart rate in newborns. Can J Physiol Pharmacol 61: 329–335.
Hathorn MKS 1987 Respiratory sinus arrhythmia in new-born infants. J Physiol 385: 1–12.
Hathorn MKS 1989 Respiratory modulation of heart rate in newborn infants. Early Hum Dev 20: 81–99.
Hyndman BW, Kitney RI, Sayers BMcA 1971 Spontaneous rhythms in physiological control systems. Nature 233: 339–341.
Thompson CR, Brown JS, Gee H, Taylor EW 1993 . Heart rate variability in healthy term newborns: the contribution of respiratory sinus arrhythmia. Early Hum Dev 31: 217–228.
Lindqvist A., Oja R, Hellman O, Välimäki I 1983 Impact of thermal vasomotor control on the heart rate variability of newborn infants. Early Hum Dev 8: 37–47.
Kellerová E 1971 Vasomotor rhythms in acral skin region as influenced by regularly spaced stimuli. J Interdiscipl Cycle Res 2: 233–237.
Pomerlau-Malcuit A Clifton RK 1973 Neonatal heart rate responses to tactile, auditory, and vestibular stimulation in different states. Child Dev 44: 485–496.
Jahnukainen T, van Ravenswaaij-Arts C, Jalonen J, Välimäki I 1993 Dynamics of vasomotor thermoregulation of the skin in term and preterm neonates. Early Hum Dev 33: 133–143.
Hathorn MKS, Mannix PA, Costeloe K 1995 . Effect of periodic thermal stimulus on heart rate in term newborn infant. J Appl Physiol 79: 1093–1099.
Prechtl HFR, Beintema D 1964 The neurological examination of the fullterm newborn infant. Little Club Clinics in Developmental Medicine No. 12. Heinemann, London
Okada M 1979 A digital filter for the QRS complex detection. IEEE Trans Biomed Eng 26: 700–703.
Scholten CA, Vos JE, Prechtl HFR 1985 Combined profile of respiration, heart beat, and motility in newborn infants: a methodological approach. Med Biol Eng Comput 23: 15–22.
Bendat JS, Piersol AG 1966 Measurement and Analysis of Random Data. Wiley, New York, 287–300.
de Boer RW, Karemaker JM, Strackee J 1985 Description of heart rate variability data in accordance with a physiological model for the genesis of heartbeats. Psychophysiology 22: 147–155.
Prechtl HFR 1974 The behavioural states of the newborn infant (review). Brain Res 76: 185–212.
Curzi-Dascalova L, Peirano P, Morel-Kahn F 1988 . Development of sleep states in normal premature and full-term newborns. Dev Psychobiol 21: 431–444.
Cleave JP, Levine MR, Fleming PJ 1984 . The control of ventilation: a theoretical analysis of the responses to transient disturbances. J Theor Biol 108: 261–283.
Acknowledgements
The authors thank T. G. Barnett for expert assistance with electronics.
Author information
Authors and Affiliations
Additional information
Support was provided by the NE Thames Regional Health Authority Locally Organised Research Scheme and The Wellcome Trust Grant 16935.
Rights and permissions
About this article
Cite this article
Mannix, P., Inwald, D., Hathorn, M. et al. Thermal Entrainment of Heart Rate in the Preterm Infant. Pediatr Res 42, 282–286 (1997). https://doi.org/10.1203/00006450-199709000-00006
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199709000-00006
This article is cited by
-
Birth prematurity determines prolonged autonomic nervous system immaturity
Clinical Autonomic Research (2004)