Abstract
Transient hypothyroxinemia in infants born to mothers with Graves' disease is a unique disorder first reported by us in 1988. Most mothers of these infants have had no treatment, are diagnosed as having thyrotoxicosis during the last trimester, or were not well controlled during pregnancy. These infants are believed to have transient central hypothyroidism, the mechanisms of which have not been elucidated. We measured TSH-receptor antibody activities in maternal serum and blood thyroxine (T4) (free thyroxine, FT4) and TSH levels in blood dried on filter paper at 1, 3, and 5 d of age in 114 infants born to mothers with Graves' disease. The 114 infants were retrospectively divided into three groups according to the clinical course and thyroid function data: group G, neonatal thyrotoxicosis; group T, transient hypothyroxinemia; and group E, euthyroid. In group T, the dried blood T4 (FT4) level from cord blood and/or 1 d of age blood was 6.0± 2.3 μg/dL (0.92 ± 0.52 ng/dL), a value significantly higher than that at 5 d of age (3.6 ± 1.0 μg/dL; 0.38 ± 0.18 ng/dL)(p = 0.025 in T4, p = 0.042 in FT4). In contrast, these levels were significantly lower at birth relative to 5 d in group G (p = 0.0001 in T4) and not significantly changed in group E. The TSH level of cord blood and/or 1-d-old blood in group T was significantly lower than that of group E (p = 0.0006). Moreover, the TSH levels in response to thyrotropin-releasing hormone were blunted in most infants in group T. Bone maturation was not delayed in group T, compared with euthyroid infants. The higher blood T4 (FT4) levels at birth, relative to 5 d in group T, suggested that the fetal T4 level was higher than that of the newborn period. The fetal T4 level might have been elevated owing to transfer of T4 from mother to fetus during the last trimester when the mother's thyroid function was elevated and consequently the fetal pituitary-thyroid axis was suppressed. Although the serum T4 (FT4) levels were decreased after birth, TSH levels were not elevated, probably because the pituitary-thyroid axis was suppressed. This may be the reason for the transient hypothyroxinemia with a normal TSH level in infants born to mothers with poorly controlled Graves' disease. Weak maternal thyroid-stimulating antibody activities and differences in sensitivity of the thyroid gland to TSH-receptor antibodies may contribute to this unique disorder.
Similar content being viewed by others
Main
Several types of transient thyroid dysfunction in infants born to mothers with Graves' disease have been described(1–3). We have conducted neonatal screening of congenital hypothyroidism by measuring dried blood TSH and T4(FT4) levels in the city of Sapporo, Japan, since 1981. We encountered infants with transiently low T4 (FT4) but normal levels of TSH whose mothers had active Graves' disease and were not treated at all or were diagnosed as having Graves' disease during the last trimester of pregnancy. We reported on infants with transient neonatal hypothyroxinemia who had normal levels of TSH in 1988(1), and several other cases have subsequently been reported(2, 4, 5). These infants were believed to have transient central hypothyroidism. The mechanism of central hypothyroidism and whether these were cases of secondary(pituitary) or tertiary (hypothalamic) hypothyroidism have not been elucidated. Therefore, we studied thyroid function, bone maturation, and TSH-receptor antibody activities of these infants to elucidate the mechanism of this unique phenomenon.
METHODS
Patients. Blood samples were obtained from 114 selected mothers(including some previously reported)(1) with Graves' disease and their offspring. The 114 infants were divided retrospectively into three groups according to the clinical course and thyroid function data.
Group G consisted of 17 patients with neonatal Graves' disease. Symptomatic features in the infants were restlessness, sweating, exophthalmos, irritability, and raised serum T4 and FT4 levels. Group T consisted of 30 infants with transient hypothyroxinemia with normal TSH values. These infants were identified in a neonatal T4 (FT4) screening program or by routine follow-up tests of thyroid function in newborn infants whose mothers had Graves' disease. The dried blood T4 and/or FT4 concentrations in group T infants were below 5 μg/dL and 1 ng/dL, respectively, and the low concentrations persisted for at least 2 wk. The blood-spot TSH level was not raised in any case. The blood-spot thyroxine-binding globulin level was within the normal range except in one case(1). Group E consisted of 67 control infants with normal thyroid function during the neonatal period.
Procedures. Umbilical cord blood was taken at delivery, and filter paper spots of blood were taken every other day until the infants were discharged from the hospital at 5-7 d, if they were asymptomatic. Written informed consent was obtained from the mothers of the infants.
TRH tests were performed in 12 cases for a total of 15 tests in group T infants on various days by the method previously reported by Hashimoto et al.(6). TRH tests were performed soon after the result showing hypothyroxinemia with normal TSH was available. TRH (10μg/kg) was administered i.v., and dried blood or serum samples were obtained at 30 min after the TRH injection(6).
Analysis of the dried blood and serum TSH, T4, and FT4 values were done by RIA or ELISA using commercially available kits(7). Normal values of dried blood T4, FT4, and TSH in full-term infants at 5 d of age were: 10.6 ± 2.2 μg/dL, 2.0 ± 0.2 ng/dL, and 4.6 ± 2.9 μU/mL (mean ± SD), respectively(6). Maternal blood samples were taken at or just before delivery or when the infants were referred to the hospital because of an abnormal neonatal thyroid on screening.
TBII were assayed using a radioreceptor assay of TSH by means of a commercially available kit (Baxter Co., Tokyo, Japan). TSAb were assayed by measurement of the increase of 3′,5′-monophosphate after incubation of FRTL-5 cells or porcine thyroid cells with the patient's IgG or bovine TSH. Potency of TSAb was expressed as an equivalent of bovine TSH. The normal range was less than 1.2 μU/mL bovine TSH(8).
Bone maturation was evaluated by measuring the ratio of epiphyseal to metaphyseal width of the femur as reported by Roche et al.(9). Sixty-seven infants with congenital hypothyroidism were studied to determine bone maturation. Another 67 normal infants, who were referred because of abnormal thyroid screens but were finally proved to be normal, were examined as normal controls for bone maturation.
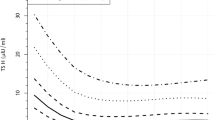
The levels of T4, FT4, and TSH were compared with cord/d-1 blood and d-5 blood by paired two-tailed t tests. The levels of TSH and TSAb activities were expressed on a logarithmic scale before statistical analysis.
RESULTS
Clinical features of transient hypothyroxinemia with normal TSH. Table 1 shows the clinical data for 14 infants in group T and their mothers who were not diagnosed or treated for Graves' disease during the whole pregnancy period. All 14 infants were detected by T4 (FT4) newborn thyroid screening among 277 000 infants examined between 1978 and 1992 in the city of Sapporo. Accordingly, thyroid function studies before 5 d of age were not available in these infants. Thyroid function test results for the mothers indicated hyperthyroidism when they visited the hospital for evaluation of the abnormal neonatal thyroid screening results. Infants weighing less than 2000 g were excluded from this study.
The remaining 16 infants were detected by routine follow-up tests of thyroid function in the newborn period because the mothers had Graves' disease. Among the 16 mothers, 10 had been treated with methimazole, six were treated with propylthiouracil, and two were treated with combinations of an antithyroid drug and Inderal. The antithyroid drug was started before 14 wk of gestation in one case, between 15 and 28 wk of gestation in six cases, and after 29 wk of gestation in nine cases. Thyroid function results for these 16 mothers varied from normal to high.
Filter paper dried blood spot T4(FT4) and TSH levels after birth. Paired blood samples of 0 and/or 1 d of age and 5 d of age were taken from 12 cases in group T, nine cases in group G, and 56 cases in group E(Table 2). In group T, the dried blood T4(FT4) levels in cord blood and/or at 1 d were 6.0 ± 2.3 μg/dL(0.9 ± 0.52 ng/dL) and were significantly higher than at 5 d of age(3.6 ± 1.0 μg/dL 0.38 ± 0.18 ng/dL) (p < 0.05). In contrast, T4 (FT4) values were higher at 5 d of age in group G (p < 0.02), and were not changed or only slightly elevated in group E (Table 2). In case 11 (Table 3), whose dried blood was obtained every day through d 5, the FT4 levels for cord blood and at 1, 2, 3, 4, and 5 d were 1.9, 1.4, 1.0, 0.6, 0.4, and 0.4 ng/dL, respectively.
The dried blood TSH level at 5 d of age in group E infants was 1.5 ± 2.9 μU/mL, a value significantly lower than in cord blood and/or at 1 d(8.1 ± 1.9 μU/mL) (p < 0.001). In contrast, the mean TSH levels in group T infants were similar at birth and 5 d. Moreover, the dried spot TSH level of cord blood and/or at 1 d in group T newborns was significantly lower than in group E infants (p < 0.01)(Table 2).
TRH test. The TRH test was performed in 12 group T infants and repeated in three for a total of 15 tests, at various days of age. The peak TSH levels in response to TRH administration are shown in Table 3. The peak TSH levels varied from no response to a low normal response. In case 11, a complete lack of response to TRH was observed at 10 and 20 d of age. The peak response of TSH to TRH increased modestly to low normal levels with advancing age. No correlation between basal TSH and peak TSH levels, or between basal FT4 and peak TSH levels, was observed.
TSH receptor antibody activities. TBII and TSAb activities of groups T, G, and E are shown in Table 4. Mean TBII and TSAb activities were significantly higher in group G than in the other groups(p < 0.0001). The mean TBII activity of group T was 24.9 ± 3.1%, a value higher than in group E infants (5.5 ± 4.7%) (p< 0.001); however, TSAb activities in the two groups were not significantly different.
Bone maturation. The mean values for the ratio of epiphyseal width/metaphyseal width of the group T infants, infants with congenital hypothroidism, and in normal infants were 0.311 ± 0.057 (n = 19), 0.225 ± 0.126 (n = 58), and 0.311 ± 0.071(n = 78), respectively. The ratio of group T was not significantly different from that of normal infants. The ratio of CH varied from zero to normal, depending on thyroid function and was significantly lower than in the other groups (p < 0.01). This ratio was significantly positively correlated with dried blood T4 and FT4 and negatively correlated with TSH at 5 d of age (p < 0.01) (data not shown).
Long-term follow-up of transient hypothyroxinemia with normal TSH. Twenty-four of the 30 infants of group T were not treated, and their thyroid functions data were followed serially. The serum T4(FT4) level gradually increased to the normal range with advancement in age. Six patients were treated with levothyroxine (L-T4) for a few months. Their thyroid functions remained within the normal range after discontinuation of medication.
DISCUSSION
In the present study, we found that the dried blood T4 (FT4) level in group T infants was higher at birth than 5 d later. This suggested that the fetal pituitary-thyroid axis was suppressed due to transfer of T4 from the mother, when her thyroid function was elevated, and that this suppression persisted after birth. This may be the reason for the transient hypothyroxinemia with normal TSH in infants born to mothers with Graves' disease.
Although hypothyroxinemia was observed in the neonatal period in group T infants, bone maturation was not delayed. This is in striking contrast to infants with congenital central hypothyroidism who are also detected by low T4 (FT4) levels during newborn screening(10).
The cord blood FT4 level in case 11 was 1.9 ng/dL, decreased to 0.4 ng/dL at 4 d, and remained at a low level thereafter. Moreover, the serum TSH response to TRH administration was blunted when performed at 10 and 20 d of age, and was found to be at low normal levels on d 120 and 263. This evidence indicated that the pituitary-thyroid axis was suppressed for a long period of time in this patient (Table 3).
The suppression of the pituitary-thyroid axis is postulated to be due to fetal hyperthyroxinemia during the last trimester. Two mechanisms may be considered for the etiology of fetal hyperthyroxinemia. One is transport of T4 from mother to fetus, the second is transport of TSI from mother to fetus, which causes fetal thyrotoxicosis, as suggested by Mandel et al.(4). Most of the hyperthyroid mothers of the group T infants in the present study either received no treatment or were diagnosed as having thyrotoxicosis during the last trimester and were not well controlled during pregnancy. This suggested the existence of maternal hyperthyroxinemia during pregnancy, particularly during the last trimester. Recent data indicate that maternal thyroid hormones, particularly T4, are transported from mother to fetus during early gestation, before fetal thyroid function is developed(11, 12), and also during the last trimester near term(13). These thyroid hormones may contribute significantly to neurologic development of the fetus and newborn(14, 15). That the cord blood and/or 1-d-old blood T4 (FT4) level was higher than that at 5 d of age suggested a maternal origin of T4 in these group T infants. The absolute values of T4 (FT4), however, were not elevated in this study because those infants whose thyroid function data were collected serially after birth were under medical control, and their mothers had been treated with antithyroid drugs. The cord blood T4 level in infants whose mothers were not treated during pregnancy might have been elevated. However, these infants were referred to the hospital at the age of 10 to 14 d because of an abnormal result on neonatal thyroid screening, and none of their cord blood samples was available for analysis.
The second possible mechanism for fetal hyperthyroxinemia is transport of thyroid-stimulating Ig from mother to fetus causing fetal thyrotoxicosis and suppression of the fetal pituitary-thyroid axis. It is well known that fetal thyrotoxicosis occurs when maternal hyperthyroidism is not properly treated during pregnancy(16, 17). Our present findings, as well as previous reports, show that potent TBII and TSAb activities in mothers are associated with development of neonatal and fetal thyrotoxicosis(1, 2, 18). The TSH-receptor antibody activities in mothers of group T infants were characteristic. The TBII activity varied from potent to weak; however, none of the mothers possessed potent TSAb activity. Thus maternal TSH receptor-stimulating antibodies are not likely to be the cause of postulated fetal thyrotoxicosis in these infants. In the case reported by Slyper and Shaker(5), similar findings were manifested.
The dissociation between TBII and TSAb activities observed in group T mothers differs from the correlation between TBII and TSAb activities usually observed in patients with Graves' disease at diagnosis(19); however, dissociation between TBII and TSAb activities has been observed in some cases with Graves' disease during antithyroid treatment(19). Moreover, potent TSAb activities with weak TBII activities are reported in cases of euthyroid Graves' disease(20). With the recent development of DNA technology, the specific epitopes for binding of TSH, thyroid-stimulating antibody, and thyroid stimulation-blocking antibody have been characterized(21, 22), but the nature of TSH-receptor antibodies found in group T patients remains to be elucidated.
Although all the mothers of group T exhibited clinical symptoms of thyrotoxicosis, none of their infants developed fetal or neonatal Graves' disease. A possible reason may be the difference in sensitivity of the thyroid gland to the TSH-receptor antibodies in the infants and their mothers.
The characteristic feature of thyroid function in group T infants was pituitary-thyroid suppression with an inappropriately low TSH level. The TSH response to TRH was blunted or low normal even at 4 mo of age(Table 3). The reinstitution of normal TSH secretion characteristics during medical treatment of adults with Graves' disease usually requires 0.5-9 mo(23, 24). Once thyroid hormones reach a low normal threshold level, TSH secretion occurs after a lag period of approximately 5 wk(23, 24). Such reequilibration takes 3-19 mo in childhood Graves' disease(25) and 3¼ y in neonatal thyrotoxicosis after antithyroid treatment(4). The inappropriately low TSH secretion might be due to an altered set point for pituitary-thyroid feedback control or a reduced capacity for TSH secretion caused by increased T4 concentrations during a critical stage of fetal life(26). Conversely, an elevated threshold for feedback regulation of TSH release was reported in patients with congenital hypothyroidism for varying periods of time(27).
The mechanism causing prolonged suppression of the pituitary-thyroid axis is not clear. Excess thyroid hormones could cause hypothalamic dysfunction with either diminished TRH secretion or elevated somatostatin secretion. We observed an elevated basal prolactin level as well as an exaggerated response to TRH administration in group T infants. These phenomena, combined with a blunted or low normal TSH response to TRH, indicates that infants in group T suffered from dysfunction of their pituitary thyrotrophs, but not lactotrophs. Consequently, the transient hypothyroxinemia in these infants likely represents secondary, rather than tertiary, hypothyroidism (S. Harada, unpublished data).
The long-term prognosis for transient hypothyroxinemia with normal TSH is not clear. In the present study, case 9 had repeated TRH tests and a low normal TSH response to TRH at the age of 9 mo. L-T4 was discontinued at the age of 9 mo in case 11, and thyroid function as well as physical and mental development seemed to be normal when the child was last examined at the age of 2 y. The transient hypothyroidism in infants born to mothers with TSH-receptor blocking antibodies is also an important disease entity during the perinatal period(28). The prognosis of these infants was thought to be good when first reported in 1980(28); however, the long-term prognosis for intellectual development was subsequently found to be very poor, particularly in those children whose mothers were not properly treated during pregnancy(29). The prognosis for life in infants with intrauterine thyrotoxicosis(16) and the intellectual prognosis with neonatal thyrotoxicosis are reportedly poor(30). The roles of thyroid hormones in perinatal and neonatal neurologic development have been extensively studies(14, 15); however, the effects of hyperthyroxinemia during the perinatal and neonatal periods are not well characterized. Nevertheless, long-term follow-up of thyroid function as well as physical and mental development are necessary to clarify the prognosis of this unique clinical entity.
Abbreviations
- T4:
-
thyroxine
- FT4:
-
free thyroxine
- TRH:
-
thyrotropin-releasing
- TBII:
-
TSH-binding inhibitor Ig
- TSAb:
-
thyroid-stimulating antibody
References
Matsuura N, Konishi J, Fujieda K, Kasagi K, Iida Y, Hagisawa M, Fujimoto S, Fukushi M, Takasugi N 1988 TSH-receptor antibodies in mothers with Graves' disease and outcome in their offspring. Lancet 1: 14–17.
Tamaki H, Amino N, Takeoka K, Iwatani Y, Tachi J, Kimura M, Mitsuda N, Miki K, Nose O, Tanizawa O, Miyai K 1989 Prediction of later development of thyrotoxicosis or centra hypothyroidism from the cord serum thyroid-stimulating hormone level in neonates born to mothers with Graves' disease. J Pediatr 115: 318–321.
Mitsuda N, Tamaki H, Amino N, Hosono T, Miyai K, Tanizawa O 1992 Risk factors for developmental disorders in infants born to women with Graves' disease. Obstet Gynecol 80: 356–364.
Mandel SH, Hanna CE, LaFranchi SH 1989 Neonatal hypopituitary hypothyroidism associated with maternal thyrotoxicosis. J Pediatr Endocrinol 3: 189–192.
Slyper AH, Shaker JL 1993 Neonatal hypothyroxinemia with normal thyrotropin. Clue to maternal Graves' disease. Clin Pediatr 32: 121–123.
Hashimoto H, Sato T, Horita S, Kubo M, Ohki T 1991 Maturation of pituitary-thyroid axis during the perinatal period. Endocrinol Jpn 38: 151–157.
Fukushi M, Takasugi N, Fujieda K, Matsuura N 1987 Measurements of free thyroxine and free triiodothyronine in dried blood on filter paper and its application to neonatal thyroid screening (in Japanese). J Jpn Pediatr Soc 91: 5–11.
Harada S 1991 Studies on TSH receptor antibodies in patients with juvenile Graves' disease-fundamental studies on an assay for thyroid-stimulating antibodies, using functioning rat thyroidal cell lines(FRTL-5 cells) (in Japanese). J Jpn Periatr Soc 95: 1743–1750.
Roche AF, Wainer H, Thissen D 1975 Skeletal Maturity. The Knee Joint as a Biological Indicator. Plenum, New York, 94–95.
Miyai K, Azukizawa M, Kumahara Y 1971 Familial isolated tyrotropin deficiency with cretinism. N Engl J Med 285: 1043–1048.
Morreale de Escober G, Obregon MJ, Escober del Rey F 1987 Fetal and maternal thyroid hormones. Horm Res 26: 12–27.
Contempre B, Jauniaux E, Calvo, Jurkovic D, Campbell S, Morreale de Escobar M 1993 Detection of thyroid hormones in human embryonic cavities during the first trimester of pregnancy. J Clin Endocrinol Metab 77: 1719–1722.
Vulsma T, Gons MH, deVijlder JJM 1989 Maternal-fetal transfer of thyroxine in congenital hypothyroidism due to a total organification defect or thyroid agenesis. N Engl J Med 321: 13–16.
Dussault JH 1992 Transplacental transport of thyroid hormones: possible clinical implications. Thyroid Today 15: 1–7.
Porterfield SP, Hendrich CE 1993 The role of thyroid hormones in prenatal and neonatal neurological development-Current perspectives. Endocr Rev 14: 94–106.
Page DV, Brady K, Mitchell J, Pehrson J, Wade G 1988 The pathology of intrauterine thyrotoxicosis: two case reports. Obstet Gynecol 72: 479–481.
Wallace C, Couch R, Ginsberg J Fetal thyrotoxicosis 1995 A case report and recommendations for prediction, diagnosis, and treatment. Thyroid 5: 125–128.
Mortimer RH, Tyack SA, Galligan JP, Perry-Keene DA, Tan YM 1990 Graves' disease in pregnancy: TSH receptor binding inhibiting immunoglobulins and maternal and neonatal thyroid function. Clin Endocrinol 32: 141–152.
Kasagi K, Iida Y, Konishi J, Misaki T, Arai K, Endo K, Torizuka K, Kuma K 1986 Paired determination of thyroid-stimulating and TSH-binding inhibitory activities in patients with Graves' disease during antithyroid treatment. Acta Endocrinol 111: 474–480.
Kashiwai T, Tada H, Asahi K, Hidaka Y, Tamaki H, Iwatani Y, Amino N 1995 Significance of thyroid stimulating antibody and long term follow up in patients with euthyroid Graves' disease. Endocr J 42: 405–412.
Akamizu T, Kohn LD, Mori T 1995 Molecular studies of Thyrotropin (TSH) receptor and anti-TSH receptor antibodies. Endocr J 42: 617–627.
Seetharamaiah GS, Wagle NM, Morris JC, Prabhakar BS 1995 Generation and characterization of monoclonal antibodies to the human thyrotropin (TSH) receptor: antibodies can bind to discrete conformational or linear epitopes and block TSH binding. Endocrinology 136: 2817–2824.
Fisher HRA, Hackeng WHL, Schopman W, Silberbusch J 1982 Analysis of factors in hyperthyroidism, which determine the duration of suppressive treatment before recovery of thyroid stimulating hormone secretion. Clin Endocrinol 16: 575–585.
Yamada T, Takasu N, Sato A, Aizawa T, Koizumi Y 1982 Pituitary-thyroid feedback regulation in patients with Graves' disease during antithyroid drug therapy. J Clin Endocrinol Metab 54: 83–88.
Sills IN, Horlick MN, Rapaport R 1992 Inappropriate suppression of thyrotropin during medical treatment of Graves' disease in childhood. J Pediatr 121: 206–209.
Mandel SH, Hanna CE, LaFranchi SH 1986 Diminished thyroid-stimulating hormone secretion associated with neonatal thyrotoxicosis. J Pediatr 109: 662–665.
Sato T, Suzuki Y, Taketani T, Ishiguro K, Nakajima H 1977 Age-related change in pituitary threshold for TSH release during thyroxin replacement therapy for cretinism. J Clin Endocrinol Metab 44: 553–559.
Matsuura N, Yamada Y, Nohara Y, Konishi J, Kasagi K, Endo K, Kojima H, Wataya K 1980 Familial neonatal transient hypothyroidism due to maternal TSH-binding inhibitor immunoglobulins. N Engl J Med 303: 738–741.
Matsuura N, Konishi J 1990 Transient hypothyroidism in infants born to mothers with chronic thyroiditis-a nationwide study of twenty-three cases. Endocrinol Jpn 37: 369–379.
Daneman D, Howard NJ 1980 Neonatal thyrotoxicosis; Intellectual impairment and craniosynostosis in later life. J Pediatr 97: 257–259.
Acknowledgements
The authors thank the many obstericians, neonatologists, physicians, and nurses for their kind cooperation. We also thank Dr. Naoko Momotani of Ito Hospital, Tokyo, for kind cooperation and variable comments, and Mami Ohofuji and Michiyo Kanda for their help in the preparation of the manuscript.
Author information
Authors and Affiliations
Additional information
Supported in part grants for Pediatric Research (6C-03) and “Studies on physical and mental disorders of children” from the Ministry of Health and Welfare of Japan.
Rights and permissions
About this article
Cite this article
Matsuura, N., Harada, S., Ohyama, Y. et al. The Mechanisms of Transient Hypothyroxinemia in Infants Born to Mothers with Graves' Disease. Pediatr Res 42, 214–218 (1997). https://doi.org/10.1203/00006450-199708000-00014
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199708000-00014
This article is cited by
-
Hyperthyroidism and pregnancy. An Italian Thyroid Association (AIT) and Italian Association of Clinical Endocrinologists (AME) joint statement for clinical practice
Journal of Endocrinological Investigation (2011)
-
Delayed recognition of central hypothyroidism in a neonate born to thyrotoxic mother
Indian Pediatrics (2010)
-
Mechanisms related to the pathophysiology and management of central hypothyroidism
Nature Clinical Practice Endocrinology & Metabolism (2008)
-
Premature twins of a mother with Graves' disease with discordant thyroid function: a case report
Journal of Perinatology (2007)