Abstract
Zinc supplementation could favor recovery from diarrhea in malnourished children. As the recent experimental evidence suggests that oxidative stress and intestinal anaphylaxis may contribute to the intestinal dysfunction associated with malnutrition, we postulated that zinc could act through antioxidant or antianaphylactic properties. Control (C), malnourished (M), and malnourished zinc-treated (MZ) guinea pigs were, respectively, fed a normal 30% protein diet, a low 4% protein diet, and a low 4% protein diet plus 1800 ppm of zinc. Milk proteins were included in the diets to trigger intestinal anaphylaxis. Milk sensitization was assessed by passive cutaneous anaphylaxis(PCA) against β-lactoglobulin and by intestinal anaphylaxis measured in Ussing chambers by the increase in short circuitcurrent after addition ofβ-lactoglobulin (ΔIscβLg). Oxidative stress was assessed by intestinal lipid peroxidation. The intestinal secretion was assessed by ΔIsc induced by inflammatory mediators. Malnutrition increased the level of anti-βLg reaginic antibodies [PCA = 1.19 ± 0.79 and 0.69 ± 0.67 log(1/titer) in M versus C guinea pigs, p = 0.07] and enhanced intestinal anaphylaxis(ΔIscβLg = 16.4 ± 9.9 and 9.1 ± 5.8μA/cm2 in M versus C guinea pigs, p = 0.07), without inducing intestinal lipid peroxidation. Moreover, malnutrition enhanced significantly the intestinal secretory response to histamine and 5-hydroxytryptamine. Administration of pharmacologic doses of zinc during malnutrition inhibited the increase in milk sensitization induced by malnutrition, both at the systemic [PCA = 0.35 ± 0.55 log(1/titer) in MZ guinea pigs, p = 0.03 versus M] and intestinal(ΔIscβLg = 2.8 ± 2.5 μA/cm2 in MZ guinea pigs; p = 0.001 versus M) level, and prevented the hypersecretion in response to histamine and 5-hydroxytryptamine. These data suggest that zinc has antianaphylactic and antisecretory properties that may contribute to its capacity to prevent intestinal dysfunction during malnutrition.
Similar content being viewed by others
Main
Malnourished children often have diarrhea. A series of confounding factors, including the nutritional status, sanitary environment, as well as the multifactorial origin of diarrhea, render the relationship between malnutrition and intestinal dysfunction difficult to define. Among the many mechanisms of diarrhea in malnutrition, food allergy seems a likely possibility, particularly in chronic diarrhea(1). Oxidative stress, which is an agent of gastrointestinal damage in various diseases(2), could also be involved in the diarrhea associated with malnutrition, because antioxidant defenses are reduced in malnourished children(3). Furthermore, mast cell mediators(4) and oxidants(2) trigger chloride secretion. Hence, both intestinal anaphylaxis and oxidative stress may result in intestinal hypersecretion. In addition, experimental data showed that low protein diets induced intestinal lipoperoxidation in the rat(5) and increased intestinal anaphylaxis in response to cow's milk proteins in the guinea pig(6).
The relationship between zinc and diarrhea is well established: diarrhea leads to zinc loss and abnormal zinc metabolism, and conversely, zinc deficiency results in diarrhea(7). In children, oral zinc therapy improves intestinal permeability(8), helps them to recover from acute diarrhea(9), and reduces the incidence of persistent diarrhea(10). It is more efficient in malnourished than well nourished children(8, 9). These important clinical findings may result from many biologic effects of zinc(11). As an essential nutrient, zinc is capable of correcting a proved zinc deficiency and also of covering the high zinc requirements associated with catch-up growth in malnourished children(12). However, the action of zinc at the intestinal level may involve more direct effects, including local anti-inflammatory activity(13). Indeed, we have recently shown that zinc is able to maintain intestinal structure and function of malnourished guinea pigs, because treatment with high doses of dietary zinc throughout the period of malnutrition prevents the increase in paracellular permeability associated with malnutrition(14). Because antioxidant(15, 16) and anti-anaphylactic(17, 18) properties have been attributed to zinc, we postulated that zinc may prevent the intestinal dysfunction associated with malnutrition by protecting the intestinal mucosa against oxidative or anaphylactic injury. To test this hypothesis, we assessed the effect of zinc on the sensitization to milk proteins, the antioxidant/pro-oxidant balance in intestinal mucosa and intestinal function, in malnourished guinea pigs.
METHODS
Animals and diets. Male Dunkin-Hartley guinea pigs (Charles River, Saint-Aubin les Elboeuf, France) were randomly given free access to one of three diets at weaning. The diets, the composition of which is given in Table 1, were based on the known nutritional requirements of the guinea pig(19) and purchased from INRA/APAE(Jouy en Josas, France). A well nourished control group of guinea pigs (C,n = 9 animals) was given a normal protein diet containing 26% soya proteins plus 4% milk proteins. Soya proteins were corrected for their deficiency in sulfur-containing amino acids with 1% methionine. Cow's milk proteins were provided by Protarmor, Saint-Brice-en-Cogiès, France, and consisted of whey proteins naturally rich in βLg. A malnourished group(M, n = 11 animals) was given a diet which contained the same number of calories as the control, but only 4% milk proteins, and in which soya proteins were replaced by carbohydrates (saccharose and cornstarch, 1/3:2/3). A malnourished, zinc-treated group (MZ, n = 6 animals) was given the same low protein diet, enriched with 1800 ppm of zinc (ZnSO4). Because diets with low protein concentrations induce anorexia, animals given such diets suffer from protein energy malnutrition rather than strict protein deficiency. The zinc content of the C and M diets (45 ppm) was adequate. In contrast, we added high doses of zinc (1800 ppm) to the diet of the MZ guinea pigs to have the best possible chance of observing its optimal effect as a pharmacologic agent. Zinc has been shown to be nontoxic in the guinea pig, even in high doses(19). However, this large amount of zinc may not apply to supplementation in human nutrition, because adverse effects have been demonstrated after the ingestion of zinc supplements in excessive amounts and/or prolonged periods(20, 21).
Experimental design. Three days before the experiments, milk proteins were replaced by soya proteins to keep the intestine free of allergic reactions before anaphylactic responses were tested. After 18-20 d on their respective diets, the guinea pigs were anesthetized i.p. with 90 mg/kg sodium pentobarbital. Their blood was collected by cardiac puncture, and plasma samples were stored at -80 °C for later estimation of protein and zinc content, and of the systemic immune response to βLg.
The entire small intestine up to the cecum, starting 10 cm from the pylorus, was removed and carefully rinsed free of intestinal content with cold Ringer solution containing (in mM): 140 Na+, 5.2 K+, 120 Cl-, 25 HCO3-, 1.2 Ca2+, 2.4 HPO42-, 0.4 H2PO4-, 1.2 Mg2+, and 2 glutamine. The first 20 cm of the jejunum was stripped of the outer muscle layer, cut into segments, and immediately used for in vitro studies in Ussing chambers. The remaining small intestine was opened along the mesenteric border, the mucosa was scraped away with the blunt edge of a glass slide, washed three times by resuspension in 10 mM Tris-HCl, 150 mM KCl, 1 mM EDTA, and 1 mM dithioerythritol, pH 7.4, and centrifuged for 5 min at 700 ×g. The pellet was homogenized in 5 volumes of 10 mM Tris-HCl buffer containing 150 mM KCl, 1 mM dithioerythritol and 0.25 mM phenylmethylsufonyl fluoride, pH 7.4, and frozen at -80 °C for later estimation of protein, DNA and zinc content, enzymatic antioxidant defenses, and free radical damage. Protein and DNA contents were, respectively, determined using the Folin phenol reagent(22) and the Burton reagent(23).
Zinc measurement. The zinc concentration was measured in plasma and intestine. Plasma was diluted 1:5 with doubly deionized water. Intestinal homogenates were mineralized in Teflon bombs placed in a microwave enclosure(MDS81D, CEM Corp, Matthews, NC): 50 μL of intestinal homogenates were mineralized with 300 μL of ultrapure nitric acid at 500 W for 5 min and then appropriately diluted with doubly deionized water. The zinc in the samples was measured by air-acetylene flame atomic absorption (Perkin-Elmer spectrophotometer model 2380, Norwalk, CT) using a wavelength of 213.8 nm.
Intestinal electrical parameters in Ussing chambers. Eight adjacent jejunal segments from each animal were mounted in Ussing chambers as flat sheets with an exposed area of 0.5 cm2. They were bathed on both sides with 12 mL of Ringer's solution, which was continuously thermostated, circulated, oxygenated, and maintained at pH 7.4 with 5% CO2 in 95% O2. The mucosal and serosal bathing solutions were connected via agar bridges to calomel electrodes for measurement of the transepithelial potential difference, and to Ag-AgCl electrodes for current application. The tissue was kept under short-circuit conditions by an automatic clamping device (World Precision Instruments, Aston, England) that canceled out fluid resistance. The short-circuit current (Isc) was constantly recorded, and the tissue was pulsed at 0.5 mV every 30 s. The Isc deflection was used to calculate ionic conductance (G) according to Ohm's law.
Isc and G, measured 30 min after tissue mounting, were taken as the basal electrical parameters. Basal Isc was used as an index of total electrogenic secretion and G as an index of paracellular permeability. Ionic secretion was estimated from the degree of I sc stimulation in response to various inflammatory secretagogues, a rise in Isc reflecting chloride secretion. The maximal increases in I sc (ΔIsc) induced by serosal addition of the oxidant H2O2 (1 mM) or of the mast cell mediators PGE2 (1μM), histamine (100 μM), or 5-hydroxytryptamine (100 μM) were measured, each secretagogue being added in two of the eight chambers.
Immune sensitization to βLg. Systemic antibody responses. Immune sensitization to cow's milk proteins was estimated as previously described(24) by considering the milk antigen βLg as a sensitizing antigen. In the guinea pig allergic to cow's milk, anaphylactic antibodies belong to both the IgE and IgG subclasses and can be measured simultaneously by PCA against βLg. For this purpose, aliquots of 100 μL of serially diluted sera (1:2/1:256) from the experimental guinea pigs were injected intradermally into sites on the back of closely shaven naive guinea pigs fed a commercial chow. Seventy-two hours after serum injection, 2.5 mg of βLg in Evans blue dye (1% in NaCl solution) was injected i.v. in a final volume of 0.5 mL. One hour later, PCA reactivity was measured as the diameter of local blue skin patches. Titers were expressed as the log of the last dilution giving blue patches at least 4 mm in diameter.
Intestinal anaphylaxis. The local intestinal immune response was assayed in Ussing chambers by recording the rise in Isc induced by serosal addition of 100 μg/mL βLg. The Isc response to the sensitizing antigen βLg is known to be due to the electrogenic chloride secretion induced by mast cell degranulation and the subsequent release of inflammatory mediators(4). Therefore, the maximal increase in Isc induced by βLg(ΔIscβLg) was taken as an index of intestinal anaphylaxis.
Enzymatic antioxidant defenses and free radical damage in the intestine. Enzymatic defenses against oxidative damage were evaluated by measuring the activities of SOD (EC 1.15.1.1), Se-GPx (EC 1.11.1.9), and catalase (EC 1.11.1.6) as well as the concentration of the non-protein sulfhydryl groups, mostly reduced glutahione. Free radical damage was estimated by measuring the TBARS, which constitute malonadehyde and similar by-products of lipid peroxidation. TBARS, enzymatic activities, and glutathione content were determined in plasma or intestinal homogenates by colorimetry, as previously described(5).
Statistical analysis. Data were analyzed by a nonparametric test. Multiple comparisons followed by group to group comparisons were performed by the Kruskal-Wallis one-way analysis of variance, included in the NPARIWAY procedure of the SAS package (SAS Institute, Cary, NC). Results are means ± SD, with n as the number of animals.
RESULTS
Nutritional status of guinea pigs. Figure 1 and Table 2a show the nutritional status of the three groups of guinea pigs. Well nourished control guinea pigs (C) gained weight regularly throughout the study (Fig. 1). In contrast, the animals given the low protein diets (M and MZ) experienced weight loss, and there were no significant differences in body weight between the two groups of malnourished animals respectively, treated with zinc (MZ) and not (M). Thus, at the end of the study the malnourished animals had a body weight that was below their initial weight at weaning and was about half the weight of the well nourished animals at the end of the feeding schedule. The plasma protein levels were significantly lower in the M and MZ groups of malnourished animals than in the control group C (Table 2a). The situation was quite different in the intestine, where the protein content was not modified by malnutrition alone (M) but increased during malnutrition with zinc treatment (MZ). None of the three diets altered mucosal DNA content. Zinc treatment (MZ) dramatically raised the serum and mucosal zinc concentrations.
Evolution of body weight in guinea pigs in the three dietary groups. Each point represents the mean value ± SD for n = 6 to 11 animals. Animals were weaned on d 0 of the study. From the 5th d of the dietary protocol, the mean body weight of the malnourished guinea pigs (M and MZ groups) was significantly lower (p < 0.01) than that of control animals (C group).
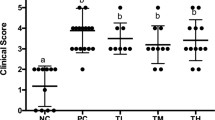
Immune responses to βLg. Systemic sensitization. As shown in Figure 2, giving cow's milk proteins to guinea pigs induced a systemic humoral anti-βLg response in all groups, although in varying degrees. Thus PCA titers were higher in malnourished M than well nourished C guinea pigs. In contrast, in guinea pigs treated with zinc during malnutrition (MZ), PCA titers did not differ from the control titers, and were significantly lower than the corresponding titers in the malnourished M group. Thus, zinc treatment during malnutrition (MZ) prevented the increase in the systemic immune sensitization induced by malnutrition alone (M).
Systemic and local intestinal immune responses toβLg in guinea pigs fed the three experimental diets. PCA, titers of passive cutaneous anaphylaxis; ΔIscβLg, maximal increase in short-circuit current in response to βLg. Results are means ± SD, n = 6 to 11 animals. *Significantly different from the malnourished group C (p < 0.05).†Signficantly different from the malnourished group M (p < 0.05).
Intestinal anaphylaxis. Milk sensitization was demonstrated in the intestine by in vitro anaphylaxis in response to βLg: a rapid increase in Isc was observed after the addition of βLg to the serosal side of jejunal segments from all the guinea pigs. As shown in Figure 2, the mean maximal magnitude of this increase,ΔIscβLg, was greater in the malnourished M group than in the well nourished C group, suggesting that malnutrition increases intestinal anaphylaxis. In contrast, when malnourished guinea pigs were treated with zinc (MZ), ΔIscβLg dropped significantly, not only compared with the malnourished M group, but also to the control C group. Therefore, zinc treatment (MZ) inhibited the increase in sensitization to βLg induced by malnutrition alone (M), both at the systemic and intestinal levels.
Enzymatic antioxidant defenses and free radical damage.Table 2 (b and c) shows the level of lipid peroxidation(TBARS) and the enzymatic antioxidant activities in the intestinal mucosa. Data were expressed per mg of mucosal DNA, because no significant differences were observed between the DNA content of the three dietary groups. The free radical metabolizing potential of the small intestine was not altered by malnutrition, as attested by the absence of significant differences in the activities of catalase, SOD, and the glutathione system (Se-GPx) in M and C guinea pigs. Malnourished animals treated with zinc (MZ) exhibited significantly higher intestinal SOD activity, but their catalase and glutathione system activities remained unchanged compared with those of both the C and M groups. In addition, neither malnutrition alone (M), nor zinc treatment during malnutrition (MZ) modified intestinal free radical damage, as indicated by the similar TBARS content in mucosa in the three dietary groups. Moreover, the TBARS level in plasma (Table 2b) were similar in the three groups, suggesting that the absence of oxidative stress during malnutrition was not limited to the intestine.
Intestinal electrical parameters. Basal electrical parameters. Basal jejunal electrical parameters are reported in Table 3. Both Isc and G increased significantly in the malnourished M group compared with the well-nourished control C group. Zinc tented to reverse, although not significantly, the rise in G observed during malnutrition.
Electrogenic response to inflammatory mediators.Figure 3 shows the mean values for the maximal increase in Isc (ΔIsc) induced by the in vitro addition of H2O2 and the mast cell mediators PGE2, histamine, and 5-hydroxytryptamine. In response to all four secretagogues,I sc increased significantly more in jejunal segments from the malnourished M guinea pigs than from the well nourished C guinea pigs. Zinc treatment during malnutrition prevented, either partially or totally, this increased secretory activity in response to inflammatory mediators, although I sc response to H2O2 remained significantly increased in the MZ group.
Maximal increase in Isc(ΔIsc) induced by inflammatory mediators in jejunal segments from guinea pigs fed the three experimental diets. Effect of 1 mM H2O2 (serosal), 1 μM PGE2 (serosal), 100 μM histamine (serosal), and 100 μM 5-hydroxytryptamine (5HT, serosal). Results are means ± SD; n the number of animals, was 9, 11, and 6, for C, M, and MZ, respectively. *Significantly different from the control group C (p < 0.01).†Significantly different from the malnourished group M (p< 0.01).
DISCUSSION
The present results confirm that zinc is able to prevent intestinal dysfunction during malnutrition and suggest that antianaphylactic and antisecretory, rather than antioxidant, properties may contribute to the protective effect of zinc on the intestine.
In the present model of malnourished milk-sensitized guinea pigs, as in other models of experimental malnutrition, the intestinal transport of ions is altered. Here, we confirmed that experimental malnutrition exacerbates the chloride secretion in response to inflammatory mediators(25) and increases the intestinal ionic conductance(26). The antibody and Isc responses toβLg were stronger in malnourished than control animals, confirming that malnutrition, like intestinal inflammation(27), enhances milk sensitization in guinea pigs(6). Neither the lipoperoxidation nor the antioxidant enzyme activities in the intestinal mucosa were altered by malnutrition, suggesting that, unlike what we observed in rats(5), malnutrition did not induce oxidative stress in guinea pigs. This might be due to species differences, because antioxidant enzyme activities were 6 (Se-GPx), 14 (catalase), and 16 (SOD) times greater in guinea pig than rat intestine(5), suggesting that the guinea pig is much better protected against free radical damage.
The major finding of this study is that zinc significantly prevented, both at the systemic and intestinal level, the exacerbation of milk sensitization induced by malnutrition. The inhibition of intestinal anaphylaxis might result from a local, membrane stabilizing effect of zinc(28), operating either on the submucosal immune cells involved in the anaphylactic reaction or on the enterocyte. Thus, the reduction of βLg-induced secretion by zinc might be due to decreased release of inflammatory mediators by mucosal mast cells. Indeed, zinc was previously shown to block both nonspecific histamine release(18) and IgE-mediated histamine release(17) from mast cells in vitro. The low PCA reactivity observed here in zinc-treated guinea pigs reflects a decrease in the level of systemic anaphylactic antibodies and suggests that inhibition of milk sensitization by zinc may involve direct modulation of the immune system. Such decrease in reaginic antibodies could also be secondary to the stabilization of mast cells, because mast cells have been involved in the induction of IgE production by B cells(29).
The involvement of zinc in protein metabolism(11) might explain the high protein content that we found in the small intestine of zinc-treated animals, although their body weight and plasma protein were still depressed, indicating that zinc alone was unable to correct malnutrition. Although the low protein diet had an adequate zinc content and did not induce hypozincemia or mucosal zinc depletion in our malnourished guinea pigs, their intestine displayed great functional responsiveness to the pharmacologic dose of dietary zinc we used. Zinc inhibited the malnutrition-induced increase in transepithelial conductance, showing its protective effect on the paracellular intestinal permeability, as previously described in malnourished nonsensitized guinea pigs(14). In addition, zinc reduced chloride secretion, because it prevented the rise in short-circuit current responses to mast cell mediators, observed during malnutrition. This decreased secretion might be due to a stabilizing effect of zinc on the eneterocyte, and could explain, at least in part, the inhibition of intestinal anaphylaxis we observed in the zinc-treated group. Such an antisecretory effect of zinc could be considered as a part of a more general anti-inflammatory effect, because zinc is also able to inhibit the contractile response of guinea pig intestine to 5-hydroxytryptamine and histamine(30).
The absence of lipoperoxidation and the fact that zinc was unable to prevent the hypersecretory response induced by the oxidant H2O2 seem to exclude the possibility that zinc acts as an antioxidant in this guinea pig model. Indeed, the capacity of zinc to exert a direct antioxidant protection has been recently questioned by both in vitro(31) and in vivo(32) studies. In our study, one of the antioxidant enzyme, SOD, was increased by zinc treatment. This result was unexpected because high dietary zinc was previously shown to decrease SOD activity(33), owing to an impairment of copper status(34). However, alteration of copper status by high zinc diets is not a constant finding(16, 35), and because SOD activity is directly related to the tissue concentration of copper(15, 33), the present increase in SOD activity suggests that the copper status of the intestine was not harmed by zinc treatment. Although an induction of SOD may reflect an exposure to oxidative stress, such a possibility is unlikely, because intestinal lipoperoxidation did not increase in the MZ group.
The use of zinc in the medical management of malnutrition will become widespread in the next few years, because it is now recommended by the World Health Organization in its recent manual on treatment of severe malnutrition(36). However, the mechanisms underlying the protective effect of zinc on diarrhea during malnutrition are still unknown. The present data suggest that the protection exhibited by zinc in the intestine involves an inhibition of the secretion induced by mucosal mast cells mediators during intestinal anaphylaxis. Such an antisecretory effect of zinc may help to explain the mechanism by which zinc inhibits fluid hypersecretion in the gut of malnourished children.
Abbreviations
- βLg:
-
β-lactoglobulin
- C:
-
control
- G :
-
ionic conductance
- Isc:
-
short-circuit current
- M:
-
malnourished
- MZ:
-
malnourished, treated with zinc
- PCA:
-
passive cutaneous anaphylaxis
- PGE2:
-
prostaglandin E2
- Se-GPx:
-
selenium-dependent glutathione peroxidases
- SOD:
-
superoxide dismutases
- TBARS:
-
thiobarbituric acid-reacting substances
References
Walker-Smith JA 1982 Cow's milk intolerance as a cause of postenteritis diarrhoea. J Pediatr Gastroenterol Nutr 1: 163–173.
van der Vliet A, Bast A 1992 Role of reactive oxygen species in intestinal diseases. Free Radic Biol Med 12: 499–513.
Golden MH, Ramdath D 1987 Free radicals in the pathogenesis of kwashiorkor. Proc Nutr Soc 46: 53–68.
Castro GA, Powell DW 1994 The physiology of the mucosal immune system and immune-mediated responses in the gastrointestinal tract. In: Johnson LR(ed) Physiology of the Gastrointestinal Tract. Raven Press, New York, pp 709–750.
Darmon N, Pelissier MA, Heyman M, Albrecht R, Desjeux JF 1993 Oxidative stress may contribute to the intestinal dysfunction of weanling rats fed a low protein diet. J Nutr 123: 1068–1075.
Darmon N, Heyman M, Candalh C, Blaton MA, Desjeux JF 1996 Anaphylactic intestinal response to milk proteins during malnutrition in guinea-pigs. Am J Physiol 270:G442–G448.
Hambidge KM 1992 Zinc and diarrhea. Acta Paediatr Suppl 381: 82–86.
Roy SK, Behrens RH, Haider R, Akramuzzaman SM, Mahalanabis D, Wahed MA, Tomkins AM 1992 Impact of zinc supplementation on intestinal permeability in Bangladeshi children with acute diarrhoea and persistent diarrhoea syndrome. J Pediatr Gastroenterol Nutr 15: 289–296.
Sazawal S, Black RE, Bhan MK, Bhandari N, Sinha A, Jalla S 1995 Zinc supplementation in young children with acute diarrhea in India. N Engl J Med 333: 839–844.
Sazawal S, Black RE, Jalla S, Bhandari N, Sinha A, Majumdar S 1996 Zinc supplementation reduces the incidence of persistent diarrhea and dysentery among low socioeconomic children in India. J Nutr 126: 443–450.
Walsh CT, Sandstead HH, Prasad AS, Newberne PM, Fraker PJ 1994 Zinc: health effects and research priorities for the 1990s. Environ Health Perspect 102: 5–46.
Golden MHN, Golden BE 1981 Effect of zinc supplementation on the dietary intake, rate of weight gain, and energy cost of tissue deposition in children recovering from severe malnutrition. Am J Clin Nutr 34: 900–908.
Milanino R, Marrella M, Gasperini R, Pasqualicchio M, Velo G 1993 Copper and zinc body levels in inflammation: an overview of the data obtained from animal and human studies. Agents Actions 39: 195–209.
Rodriguez P, Darmon N, Candalh C, Chappuis P, Blaton MA, Bouchaud C, Heyman M 1996 Intestinal paracellular permeability during malnutrition in guinea-pigs: effect of high dietary zinc. Gut 39: 416–422.
Bray TM, Bettger WJ 1990 The physiological role of zinc as an antioxidant. Free Radic Biol Med 8: 281–291.
Chvapil M, Peng YM, Aronson AL, Zukoski C 1974 Effect of zinc on lipid peroxidation and metal content in some tissues of rats. J Nutr 104: 434–443.
Marone G, Columbo M, de Paulis A, Cirillo R, Giugliano R, Condorelli M 1986 Physiological concentrations of zinc inhibit the release of histamine from human basophils and lung mast cells. Agents Actions 18: 103–106.
Kazimierczak W, Malinski C 1974 The effect of zinc ions on selective and non selective histamine release in vitro. Agents Actions 4: 1–6.
Navia JM, Hunt CE 1976 Nutrition, nutritional diseases, and nutrition research applications. In: Wagner JE, Manning PJ (eds) The Biology of the Guinea Pig. Academic Press, New-York, pp 235–267.
Fosmire G 1990 Zinc toxicity. Am J Clin Nutr 51: 225–227.
Chandra RK 1984 Excessive intake of zinc impairs immune responses. JAMA 252: 1443–1446.
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ 1951 Protein measurements with the Folin phenol reagent. J Biol Chem 193: 265–275.
Giles KW, Myers A 1965 An improved diphenylamine method for estimation of DNA. Nature 206: 93
Heyman M, Andriantsoa M, Crain-Denoyelle AM, Desjeux JF 1990 Effect of oral or parenteral sensitization to cow's milk on mucosal permeability in guinea pigs. Int Arch Allergy Appl Immunol 92: 242–246.
Young A, Levin RJ 1990 Diarrhoea of famine and malnutrition: investigations using a rat model. 1. Jejunal hypersecretion induced by starvation. Gut 31: 43–53.
Butzner JD, Gall DG 1988 Impact of protein-calorie malnutrition on the developing intestine. Biol Neonate 54: 151–159.
Fargeas MJ, Theodorou V, More J, Wal JM, Fioramonti J, Bueno L 1995 Boosted systemic immune and local responsiveness after intestinal inflammation in orally sensitized guinea-pigs. Gastroenterology 109: 53–62.
Bettger WJ, O'Dell BL 1993 Physiological roles of zinc in the plasma membrane of mammalian cells. J Nutr Biochem 4: 193–207.
Gauchat JF, Henchoz S, Mazzei G, Aubry JP, Brunner T, Blasey H, Life P, Talabot D, Flores-Romo L, Thompson J, Butterfield J, Dahinden C, Bonnefoy JP 1993 Induction of human IgE synthesis in B cells ny mast cells ans basophils. Nature 365: 1038–1041.
Cho CH, Teh GW 1991 The inhibitory action of zinc sulphate on the contractile activity of guinea-pig ileum. J Pharm Pharmacol 43: 294–296.
Markant A, Pallauf J 1996 Metallothionein and zinc as potential antioxidants in radical-induced lipid peroxidation in cultured hepatocytes. J Trace Elements Med Biol 10: 88–95.
Gatto LM, Samman S 1995 The effect of zinc supplementation on plasma lipids and low-density lipoprotein oxidation in males. Free Radic Biol Med 19: 517–521.
L'Abbe MR, Fischer PW 1984 The effects of high dietary zinc and copper deficiency on the activity of copper-requiring metalloenzymes in the growing rat. J Nutr 114: 813–822.
Fischer PWF, Giroux A, L'Abbe MR 1981 The effect of dietary zinc on intestinal copper absorption. Am J Clin Nutr 34: 1670–1675.
Reeves PG 1995 Adaptation responses in rats to long-term feeding of high-zinc diets: emphasis on intestinal metallothionein. J Nutr Biochem 6: 48–54.
Anonymous 1997 Management of severe malnutrition. A manual for physicians and other senior health workers World Health Organization, Geneve (in press)
Acknowledgements
The authors thank M. Dreyfus and M. Matysiak-Budnik for editorial assistance.
Author information
Authors and Affiliations
Additional information
Supported in part by grants from the VOLVIC Research Center on Trace Elements.
Rights and permissions
About this article
Cite this article
Darmon, N., Pélissier, MA., Candalh, C. et al. Zinc and Intestinal Anaphylaxis to Cow's Milk Proteins in Malnourished Guinea Pigs. Pediatr Res 42, 208–213 (1997). https://doi.org/10.1203/00006450-199708000-00013
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199708000-00013
This article is cited by
-
Zinc in child health and disease
The Indian Journal of Pediatrics (2004)