Abstract
Secondary brain damage after transient cerebral hypoxiaischemia (HI) is caused by a cascade of cellular events. In this study, complementary methods of magnetic resonance imaging and histochemistry were used to investigate the formation of cytotoxic and vasogenic edema during secondary brain damage induced by transient HI in 7-d-old rats. To elicit injury, 21 rats underwent right common carotid artery ligation followed by 1.5 h of 8% O2 exposure. Sequential apparent diffusion coefficient (ADC) and transversal relaxation time (T2) weighted magnetic resonance imaging were recorded for up to 3 d in 13 7-d-old rats. Eight animals were killed at various intervals between the end of HI and 21 h of recovery to perform histochemical assays using neuronal and astrocytic markers. Changes of the ADC revealed a biphasic function for the evolution of cytotoxic edema during the recovery period. At the end of HI, the ADC in the ipsilateral cortex was significantly decreased. Upon reoxygenation, it returned transiently to normal followed by a secondary, although less pronounced, decline after 8-48 h. After this, the ADC rose steadily. From 8 h of recovery, the proportion of vasogenic edema steadily increased as indicated by the T2 prolongation. At 21 h, the majority of glial cells showed immunoreactivity for glial fibrillary acidic protein and were of larger size, whereas the neurons were apoptotic. These results indicate that the delayed cerebral injury is accompanied by late glial swelling in conjunction with an enlarged interstitial space due to cell damage.
Similar content being viewed by others
Main
Cerebral HI is accompanied by excessive release of mediator compounds that cause secondary brain damage after a transient recovery from the initial destructive effect in the brain(1). Such mediators are high concentrations of extracellular glutamate and potassium, high concentrations of intracellular calcium, FFA, or oxygen radicals. Considerable scientific effort has been devoted to the role of cytotoxic(2) and vasogenic(2) edema as part of this secondary brain damage. It has been demonstrated that, during the early stages of HI, “ion control ranges over volume control” initiating cytotoxic, mostly glial swelling(3). Furthermore, the secondary metabolic events that follow glutamate excitotoxicity are also known to induce cell swelling in vitro. This is an important observation in the context of neuron-glial interaction, which involves large differences of neuronal and glial responses observed in this disease(4). On the other hand, there is also a component of vasogenic edema due to tissue necrosis and impaired blood brain barrier permeability(5).
MRI provides insight into pathophysiologic mechanisms of brain edema formation noninvasively. There are two basic approaches of decomposing edema. Cytotoxic edema can be made visible by DWI, whereas the vasogenic edema can be made visible by T2WI(6).
The neonatal rat model of combined unilateral ischemia with hypoxia provides a unique opportunity to study nature, time-course, and extent of cerebral edema(7), because it admits to titrate the severity of brain damage by varying either the time delay between the onset of ischemia and hypoxia or the intensity and duration of hypoxia. The CCA of the 7-d-old rat is occluded unilaterally followed by exposure to reduced oxygen content(8). In a previous study, we investigated the threshold duration of hypoxia causing brain edema in conjunction with unilateral CCA ligation(9). The extent of brain damage to the ipsilateral hemisphere was found to be mild for up to 30 min of hypoxia, but progressively increasing edema formation for long-term hypoxia.
In the present study, we have addressed two questions: 1) whether the evolution of cytotoxic edema after acute HI is biphasic analogous to the biphasic energy failure after HI(10,11), and 2) which cell fraction attributes to the cytotoxic edema. To answer these questions, we continuously measured 7-d-old rats with MRI over 3 d during the recovery period from a HI injury, elicited by right CCA ligation and 90-min exposure to 8% oxygen. In addition, histologic examination was performed at discrete time points to investigate the type of cells involved in in vivo studies for a better understanding of the“macroscopic” images obtained from magnetic resonance.
METHODS
Animal preparation. A total of 21 7-d-old rats (Spargue-Dawley) were subjected to unilateral CCA occlusion under anesthesia (0.7% halothane in a 70/30 mixture of N2O and O2). Hypoxia of 90-min duration was induced by reducing the inspired oxygen concentration to 8%, the time delay between surgery and hypoxia being 1 h. Spontaneous breathing was monitored. The rats were kept at a constant environmental temperature of 34 °C, which guaranteed a rectal temperature of 37 °C monitored by a copper constantan thermocouple (Marlin, Cleveland, OH). The study was approved by the Animal Ethical Committee of the University of Zurich.
MR methods. Diffusion sensitization is achieved by using balanced pairs of pulsed gradients (Stejskal-Tanner pulse sequence and its stimulated echo variant) to encode the net displacement of water molecules(12). By this way the signal S is attenuated according toequation 1 where b is the diffusion weighting factor and SO is the signal intensity for b = 0. In contrast to the free diffusion model, ADC is connected to parameters that characterize tissue at the cellular level such as intra- and extracellular diffusion coefficients, cell sizes, cellular volume fractions, and membrane permeabilities(13). Diffusion-sensitive methods can be classified into two main categories. The first category comprises diffusion weighting in the image contrast, which depends on an optimized b value for maximizing the diffusion discrimination sensitivity. Areas of restricted diffusion appear hyperintense on DWI, whereas structures with freely diffusible water are hypointense, i.e. a higher signal attenuation. It must be kept in mind that mere diffusion weighting has also a significant T2 contribution(12). The second category contains a quantitative determination of ADC values from a number of DWIs of acquired differing b values. Image contrast depends only on diffusion and, therefore, the image brightness is proportional to ADC. In summary, a slowed ADC is bright on DWI and dark on ADC maps.
For mere diffusion weighting, DWI, the stimulated echo imaging technique was used(14). The sequence parameters were TE 18 ms to minimize T2 effects, TR 2000 ms, and b 1400 s/mm2. Four averages were recorded resulting in a total experimental time of 9 min for an image matrix of 128 by 64 pixels. In addition, a pulse sequence was designed specifically to accomplish the following requirements:1) to image ischemia induced changes in T2 and ADC,2) to generate quantitative maps of ADC values, i.e. over the entire field of view, and 3) to acquire motion-free data within minutes. The imaging sequence consists of two parts: a one-dimensional diffusion sensitizing spin echo sequence introduced before a fast RARE-type image acquisition(15). Typically, three interleaved image segments were sampled to produce 128 by 96 data points (RARE factor = 32, echo spacing = 11 ms). This sequence allowed acquisition of eight images with increasing b values ranging between 0 and 1400 s/mm2 within a 5-min experimental time frame. The first image with b = 0 is purely T2 weighted, whereas ADC maps were calculated by fitting the signal intensities against b factors using the monoexponential model of Equation 1.
T2WI was taken by means of the multislice RARE technique. The RARE factor was chosen to be 16, the interecho intervall was 22 ms, and TR was 4000 ms. The voxel dimensions were approximately 115 by 230 μm.
In all MR experiments, the slice thickness was 2 mm and the field of view 4 cm. Data were acquired on a TOMIKON S200A 2 Tesla system (Bruker-Spectrospin, Fällanden, Switzerland) using a 33-cm actively shielded gradient insert for gradient field strengths up to 25 mT/m and 150-μs rise time. A home-built 1H solenoid with an inner diameter of 5 cm was used for excitation and reception of the radiofrequency signals.
For the qualitative analysis of DWI and T2WI of the ipsilateral cortex, circular ROI of 1.2-mm diameter were chosen with the highest homogeneous intensity distribution to minimize partial volume effects. Values of percent change of the image intensities were calculated as referenced to the contralateral hemisphere. The use of the nonischemic hemisphere in the same animal as a determinator of the signal intensity takes the developmental changes over 3 d into account. For quantitative diffusion imaging, the mean ADC values of ROIs within the lateral cortex were obtained from the calculated ADC maps. The deviation of the pixel by pixel analysis within the ROI was<100 μm2/s.
During the experimental MRI procedure, the rats were placed into a specially designed animal holder, which allowed anesthesia, correct coil placement, and constant temperature setting. Eight rats were used for the longitudinal study of DWI and T2WI, five rats (plus four control animals) for ADC, and eight animals for combined MRI and histology.
Histologic examination. Four times two similarly prepared rats were examined with the MRI methods either at the end of HI or at the following time points of recovery from HI: 5, 15, and 21 h, and subsequently killed for histologic examination. The rats were perfused under deep Rompun/Ketanest anesthesia with 200 mL of 4% paraformaldehyde in 0.01 M PBS, pH 7.4. Brains were removed and postfixed in the same fixative for 3 h at 4 °C, then dehydrated in ascending alcohols and embedded in paraffin according to standard techniques. Paraffin sections of 4-μm thickness were cut at the levels of the dorsal hippocampus. Paraffin sections were stained with hematoxylineosin, Luxol, and cresyl violet for routine histology. In addition, sections were immunostained for the astrocytic marker using a polyclonal anti-cow GFAP antibody. For in situ detection of apoptosis, the TUNEL method was used. Briefly, paraffin sections were rehydrated, treated with proteinase K (20 mg/mL in Tris-HCl buffer 10 mM, pH 8 at 37 °C) for 10 min, washed, and incubated with a reaction mix including the enzyme terminal transferase and biotin-16-dUTP (5 nM). Visualization was accomplished by streptavidin-alkaline phosphatase and nitro blue tetrazolium as a chromogen.
RESULTS
MRI. Consistent and reproducible results for the time courses of the relative changes in signal intensities of T2WI and DWI during the recovery period were obtained. Figure 1 demonstrates the average time courses of T2WI (upper curve) and DWI(lower curve) for a group of eight animals. Analyzing the temporal behavior, there were 1) the fast normalization in DWI after 3 h of recovery and normal findings in T2WI in the first 3 h of recovery, and 2) the appearance of a coincidence of hyperintensities in DWI and in T2WI (8-48 h of recovery). The time course >48 h of recovery was characterized by a further significant increase in T2 and a decrease of signal intensity in DWI toward normal and beyond normal values. In the latter case there was only variability between the animals. It is important to note that, for high values of T2, the DWI signal intensity is overestimated approximately by 10-15% due to residual T2 contributions (quantitative ADC values are stated below).
Time course of interhemispheric intensity difference after HI, for T2WI (top curve) and for DWI (bottom curve). T2WI was taken by means of the RARE method (TE = 160 ms), DWI by the stimulated echo imaging technique (TE = 18 ms,b = 1400 s/mm2). ROI values of the HI cortex are presented in percent change relative to the values of the homotopic contralateral hemisphere. Error bars represent SEM. The changes of signal intensity in DWI revealed a biphasic curve. Both signal intensities, the T2WI and DWI, result from an interplay of cytotoxic and vasogenic edema generation.
The characteristics of the spatial pattern were a strictly confined DWI hyperintensity in the cerebral cortex ipsilateral to the CCA ligation immediately post HI. For recovery >8 h, the regional distribution of the changes in signal intensity was similar for T2WI and DWI, commencing in cortex and striatum, spreading inward, then reaching the hippocampus and thalamus. Figure 2 shows a typical series of images of this temporal evolution from a single animal. The spreading throughout the ipsilateral hemisphere crossed finally over to the contralateral side.
Series of T2WIs (top row) and DWIs(bottom row) after HI. At 0.5 h, there was a marked DWI hyperintensity of the ipsilateral cortex. At this point, no T2 prolongation was observed. The effect of increased cortical signal intensity in DWI was reversed after 2 h of recovery, and either in DWI or in T2WI no abnormal changes of signal contrast were seen in any of the cerebral regions. For recovery >8 h, persistent changes became visible in T2WI and in DWI. Lesion areas spread inward, reaching the hippocampus and thalamus.
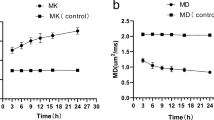
Figure 3 depicts the changes of ADC after HI in the cerebral cortex ipsilateral to the CCA ligation. The ADC mean value in four control animals was 1075 ± 150 μm2/s. This finding is consistent with data found in the literature 16). The very high value for the ADC can be explained by the higher water content and the higher extracellular volume fraction in the neonatal rat brain compared with the adult rat brain(17). In addition, ADC values may vary to some extent, depending on experimental conditions(12). The ADC mean values (n = 5) after HI changed to 625 ± 122 μm2/s at 0.5 h, 690 ± 94 μm2/s at 8 h, 866 ± 182μm2/s at 24 h, and 2860 ± 115 μm2/s at 3 d. Examples of ADC maps in conjunction with T2WI are illustrated in Figure 4. The cortical lesion areas are clearly distinguished, showing drastic ADC decline at 0.5 h, which is less pronounced at 8 and 24 h. By 3 d after HI, the ADC increased above the control value, indicating high water diffusion. Almost one entire cortical hemisphere with the underlying subcortical structures underwent necrosis and was replaced by a cystic infarction.
T2WIs (at top row, b = 0) together with ADC maps (at bottom) of a representative 7-d-old rat. The set of images shows the evolution of brain edema: (left image column) normal T2 and strongest decrease of ADC (dark area) in the cerebral cortex caused by the primary cytotoxic edema at 0.5 h; (middle two image columns) increase of T2 and less pronounced ADC reduction in the cerebral cortex and heterogeneous pattern in the subcortical structures during the secondary cytotoxic edema between 8 h and 24 h; and (right image column) very high T2 and ADC (bright area) in cortical and subcortical structures indicating cystic infarction at 3 d.
Histology. The morphology of the hippocampal formation was assessed at the end of HI and at 5, 15, and 21 h of recovery in sections stained with GFAP and by the TUNEL method. At the 0-h time point (Fig. 5, a and e), an intact neuronal ribbon was detectable. In the surrounding regions of the hippocampus, several GFAP-immunoreactive glial cells without any sign of astrogliosis were identified. The TUNEL stain did not disclose apoptotic cells as depicted in Figure 5e. As early as 5 h after onset of the lesion, however, a significant increase in the number and size of GFAP-immunoreactive glial cells was readily discernible. The neuronal ribbon was affected by intracellular and pericellular (most likely interstitial) edema (Fig. 5b). Single cells stained positive in the TUNEL reaction (Fig. 5f). The changes described above were much more pronounced after 15 h (Fig. 5, c and g). At the latest time point, disintegration of neurons and very marked edema were apparent along with marked gliosis (Fig. 5d), and the majority of neurons were TUNEL-positive (Fig. 5h).
GFAP immunocytochemistry for reactive glial cells(a-d) and TUNEL staining for cell apoptosis (e-h). The brain sections were cut at the level of the hippocampus the following time points: at the end of HI (a and e), at 5 h (b and f), at 15 h (c and g), and at 21 h(d and h) of recovery. Reactive glial cell showed enhanced labeling and larger cell size at 15-21 h, whereas at this time the majority of neurons showed apoptosis and cell shrinkage.
DISCUSSION
The pathogenic processes induced by HI were investigated by analyzing the formation of brain edema during the course of recovery. There are three major findings to be summarized: 1) The acute insult caused a biphasic decline of the ADC, which signified a characteristic temporal profile of the cytotoxic edema; 2) after 8 h of recovery a steadily increasing T2 prolongation reflected increasing proportions of the vasogenic edema, whereas infarction developed at later times; and 3) there existed transitional forms on cellular bases. The time-dependent changes of GFAP-labeled glial cells showed a maximum in number after 21 h, whereafter followed autolysis. On the other hand, the majority of neurons were apoptotic at 21 h after HI.
Although it is widely accepted that in cytotoxic brain edema a narrowing of the extracellular space leads to signal hyperintensity in DWI(18, 19), our knowledge of the mechanisms responsible for an impaired cell volume regulation remains incomplete. Because several factors probably act together to account for the disturbed regulation of cellular volume and cellular swelling, we divided the observed biphasic course into two distinct phases-a phase of primary cytotoxic edema and a phase of secondary cytotoxic edema, after a transient recovery.
The primary cytotoxic edema. The mechanisms of primary cellular swelling, which take place during the time course of HI, have been discussed previously(20). Temporary inhibition of the cell metabolism by means of HI causes transmembranous ion movements to shift from an active to a more passive transport, e.g. down an electrochemical gradient, which is accompanied by an uptake of Na+, Cl-, and water. Apart from this pump-leak model, fast neuronal release of excitatory amino acids(21), predominantly glutamate and aspartate, in conjunction with an impaired reuptake leads to an immediate increase of intracellular Na+ and water, and thus contributes to the primary cytotoxic edema. At the beginning of the recovery period, resupply of oxygen and substrates leads to cellular volume regulation if the swelling remains within recoverable limits. We interpreted the normalized signal intensity in DWI after 3 h of recovery (Fig. 2) as indicative of reversible alterations of physiologic water compartmentation.
The secondary cytotoxic edema. Although the primary cytotoxic edema could be explained by suppression of the energy metabolism of both cell types, neurons and glial cells, the question remains of which mechanisms led to the observation of a secondary occurrence of apparent restriction to diffusion, which was also accompanied by concomitant prolongation of T2. Additionally, the area of hyperintensity in DWI did spread out in a characteristic way from the peripheral cortex to the basal ganglia and hippocampus. To put this question in cellular terms, what proportion of the signal comes from neurons and what fraction from glial cells? Synapses with both presynaptic and postsynaptic structures are located close to glial cells within a very dense matrix, in which neurons and glial cells are found in roughly equal numbers. Glial cells are known to swell under conditions of lactacidosis and elevated extracellular concentrations of K+, glutamate, and other monoamine transmitters, which are released in increased amounts into the extracellular space during HI(22, 23). This cytotoxic glial swelling is interpreted as a direct consequence of an active process in an attempt to restore ion homeostasis within the neuron-glial unit. The present data support the occurrence of late glial edema, also referred to as secondary cytotoxic edema in two respects: first, the secondary decline of ADC after HI again indicated cell swelling; second, increased labeling of GFAP demonstrated not only vivid, but also activated, glial cells(24).
The vasogenic edema. An additional characteristic of the secondary cytotoxic edema was the coincidentally elevated T2, which became evident after 8 h of recovery (Fig. 2). In view of the relationship between ADC and cellular volume fraction, these changes are apparently paradoxical. It is well established that T2 is elevated when vasogenic edema starts to develop associated with an enlarged extracellular(interstitial) space(9, 25). In proposing a hypothesis within this context, the following two findings were significant. First, the time course of T2 weighted signal intensity did not show any significant changes in the early stage of recovery during which a low ADC appeared. Histopathology at this time point indicated isolated neuronal necrosis. Subsequent T2 weighted hyperintensity from vasogenic edema paralleled neuronal damage being evident as eosinophilic neuronal shrinkage and was accompanied by a strong glial response. As T2 values appeared to be higher at 24-48 h after HI, neuronal necrosis as well as apoptosis developed. Both mechanisms result in enlarged interstitial space either by cell lysis or by cell shrinkage. It should be noted that the temporal profile of neuronal damage is related to the duration of hypoxia(26). Second, the early reduction of ADC during HI fell by about 55% of baseline, whereas the secondary decline of ADC had a value of only 70-80% of baseline, which then increased toward normal (or beyond) values. Thus, it is reasonable to assume that the interplay of cytotoxic and vasogenic edema generation leads to compensating effects on the extracellular(interstitial) space. The results suggested that during the time course of secondary cytotoxic edema more and more cell lysis occurred throughout the ipsilateral hemisphere, thus weakening the underlying DWI effect while increasing the signal intensity in T2WI in a more pronounced manner, likely due to structural water changes(27). At 72 h and later, ADC values higher than normal indicated unrestricted diffusion in necrotic tissue(28). However, this development of the fluid-filled spaces proved that there is a high variability between the animals.
Conclusion. It is apparent from this study that, after the acute HI insult accompanied by a primary cytotoxic edema, cells recover transiently. Subsequently, a secondary cytotoxic swelling follows with a mixed picture of swollen intact cells, namely glial cells, and already necrotic lysed neurons, allowing both types of edema to coexist by reason of a low ADC together with an elevated T2. Although this is a simplified explanation for a complex phenomenon, the presented results of secondary glial swelling may support the role of glial cells in ionic and volume homeostasis during conditions of brain injury.

Abbreviations
- ADC:
-
apparent diffusion coefficient
- CCA:
-
common carotid artery
- DWI:
-
diffusion weighted imaging
- GFAP:
-
glial fibrillary acidic protein
- HI:
-
hypoxia-ischemia
- MRI:
-
magnetic resonance imaging
- RARE:
-
rapid acquisition with relaxation enhancement
- ROI:
-
region of interest
- T2:
-
transversal relaxation time
- T2WI:
-
T2 weighted imaging
- TE:
-
time to echo
- TR:
-
time to repeat
- TUNEL:
-
terminal deoxynucleotidyl transferase dUTP nick end labeling
References
Johnston MV 1993 Cellular alterations associated with perinatal asphyxia. Clin Invest Med 16: 122–132.
Klatzo I 1994 Evolution of brain edema concepts. Acta Neurochir Suppl 60: 3–6.
Kempski OS, Volk C 1994 Neuron-glial interaction during injury and edema of the CNS. Acta Neurochir Suppl 60: 7–11.
Tower DB 1992 A century of neuronal and neuroglial interactions, and their pathological implications: an overview. Prog Brain Res 94: 3–17.
Betz AL, Keep RF, Beer ME, Ren X 1994 Blood-brain barrier permeability and brain concentration of sodium, potassium, and chloride during focal ischemia. J Cereb Blood Flow Metab 14: 29–37.
Moseley ME, Cohen Y, Mintorovich J, Chileuitt L, Shimizu H, Kucharczyk J, Wendland MF, Weinstein PR 1990 Early detection of regional cerebral ischemia in cats: Comparison of diffusion-and T2-weighted MRI and spectroscopy. Magn Reson Med 14: 330–346.
Vannucci RC, Christensen MA, Yager JY 1993 Nature, time-course, and extent of cerebral edema in perinatal hypoxic-ischemic brain damage. Pediatr Neurol 9: 29–34.
Rice JE, Vannucci RC, Brierley JB 1981 The influence of immaturity on hypoxic-ischemic brain damage in the rat. Ann Neurol 9: 131–141.
Rumpel H, Buchli R, Gehrmann J, Aguzzi A, llli O, Martin E 1995 Magnetic resonance imaging of brain edema in the neonatal rat: a comparison of short and long term hypoxia-ischemia. Pediatr Res 38: 113–118.
Lorek A, Takei Y, Cady EB, Wyatt JS, Penrice J, Edwards AD, Peebles D, Wylezinska M, Owen-Reece H, Kirkbride V, Cooper CE, Aldridge RF, Roth SC, Brown G, Delpy DT, Reynolds EOR 1994 Delayed(“secondary”) energy failure after acute hypoxia-ischemia in the newborn piglet: continuous 48-hour studies by phosphorus magnetic resonance spectroscopy. Pediatr Res 36: 699–706.
Buchli R, Rumpel H, Maeder U, Nedelcu H, Martin E 1995 Hypoxic ischemic brain damage in neonatal rats monitored by 31P magnetic resonance spectroscopy. Pediatr Res 38: 428
Norris DG, Niendorf T 1995 Interpretation of DW-NMR data: dependence on experimental conditions. NMR Biomed 8: 280–288.
Szafer A, Zhong J, Anderson AW, Gore JC 1995 Diffusion-weighted imaging in tissues: theoretical models. NMR Biomed 8: 289–296.
Merboldt KD, Hänicke W, Frahm J 1985 Self-diffusion NMR imaging using stimulated echoes. J Magn Reson 64: 479–486.
Hennig J, Nauerth A, Friedburg H 1986 RARE-imaging: a fast imaging method for clinical MR. Magn Reson Med 3: 823–833.
Van der Toorn A, Syková E, Dijkhuizen RM, Vorísek I, Vargová L, Skobisova E, van Lookeren Campagne M, Reese T, Nicolay K 1996 Dynamic changes in water ADC, energy metabolism, extracellular space volume, and tortuosity in neonatal rat brain during global ischemia. Magn Reson Med 36: 52–60.
Lehmenkühler A, Syková E, Svoboda J, Zilles K, Nicholson C 1993 Extracellular space parameters in the rat neocortex and subcortical white matter during postnatal development determined by diffusion analysis. Neuroscience 55: 339–351.
Norris DG, Niendorf T, Leibfritz D 1994 Healthy and infarcted brain tissues studied at short diffusion times: the origins of apparent restriction and the reduction in apparent diffusion coefficient. NMR Biomed 7: 304–310.
Anderson AW, Zhong J, Petroff OAC, Szafer A, Ransom BR, Prichard JW, Gore JC 1996 Effects of osmotically driven cell volume changes on diffusion weighted imaging of the rat optic nerve. Magn Reson Med 35: 162–167.
Macknight ADC, Leaf A 1975 Regulation of cellular volume. Physiol Rev 57: 510–573.
Gordon KE, Simpson J, Statman D, Silverstein FS 1991 Effects of perinatal stroke on striatal amino acid efflux in rats studied with in vivo microdialysis. Stroke 22: 928–932.
Kimelberg HK, Sankar P, O'Connor ER, Jalonen T, Goderie SK 1992 Functional consequences of astrocytic swelling. Prog Brain Res 94: 57–68.
Kempski O, Staub F, Schneider G-H, Weigt H, Baethmann A 1992 Swelling of C6 glioma cells and glial cells from glutamate, high K+ concentrations or acidosis. Prog Brain Res 94: 69–76.
Schmidt-Kastner R, Wietasch K, Weigel H, Eysel UT 1993 Immunohistochemical staining for glial fibrillary acidic protein (GFAP) after deafferentation or ischemic infarction in rat visual system: features of reactive and damaged astrocytes. Int J Dev Neurosci 11: 157–174.
van der Toorn A, Dijkhuizen RM, Tulleken CAF, Nicolay K 1995 T1 and T2 Relaxation times of the major1 H-containing metabolites in rat brain after focal ischemia. NMR Biomed 8: 245–252.
Towfighi J, Zec N, Yager J, Housman C, Vannucci RC 1995 Temporal evolution of neuropathologic changes in an immature rat model of cerebral hypoxia: a light microscopic study. Acta Neuropathol 90: 375–386.
Hoehn-Berlage M, Eis M, Back T, Kohno K, Yamashita K 1995 Changes of relaxation times [T1, T2] and apparent diffusion coefficient after permanent middle cerebral artery occlusion in the rat: Temporal evolution, regional extent, and comparison with histology. Magn Reson Med 34: 824–834.
Gill R, Sibson R, Hatfield RH, Burdett NG, Carpenter TA, Hall LD, Pickard JD 1995 A comparison of the early development of ischaemic damage after permanent middle cerebral artery occlusion in rats as assessed using magnetic resonance imaging and histology. J Cereb Blood Flow Metab 15: 1–11.
Acknowledgements
The authors thank Professor Andreas Fanconi of the University Children's Hospital Zurich for his continues support.
Author information
Authors and Affiliations
Additional information
Supported by the Swiss National Science Foundation (SNF-32-37811.93).
Rights and permissions
About this article
Cite this article
Rumpel, H., Nedelcu, J., Aguzzi, A. et al. Late Glial Swelling after Acute Cerebral Hypoxia-Ischemia in the Neonatal Rat: A Combined Magnetic Resonance and Histochemical Study. Pediatr Res 42, 54–59 (1997). https://doi.org/10.1203/00006450-199707000-00009
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199707000-00009