Abstract
The study evaluates the long-term effect of neonatal hypoxia on the neurochemical activity of the sympathoadrenal system in the rat. One-day-old male pups were exposed to hypoxia (10% O2) for 6 d and thereafter reared under normoxia. Neonatal hypoxia reduced the body weight of 3- and 8-wk-old rats and did not change the blood pressure at 6 wk of age. In sympathetic ganglia, the content and/or turnover rates of norepinephrine were reduced in neonatal-hypoxic rats of 3 and 8 wk of age, but the content and turnover rates of dopamine were unaltered. The effect was not dependent on the type of ganglion. In the superior cervical ganglion, neonatal hypoxia had a selective effect on the type of catecholamine (dopamine versus norepinephrine), thus suggesting a selective-altered maturation of noradrenergic neurons, but presumably not of the dopaminergic small, intensely fluorescent cells. A long-term deficiency in adrenal activity was the consequence of neonatal hypoxia, as shown by the decrease in the content and turnover rate of dopamine. Neonatal hypoxia elicited a long-term decrease in the content and turnover rates of norepinephrine in heart and lungs but failed to induce a significant effect in kidneys. However, this effect was not tissue-specific. Data provide evidence that a hypoxic episode occurring during a critical period of development in the rat induces a long lasting decrease in the neurochemical activity of the sympathoadrenal system. These results are discussed in terms of their implications for human pathology.
Similar content being viewed by others
Main
The autonomic nervous system is probably of vital importance during early development. This system is activated especially at birth, as reflected by the high levels of circulating catecholamines found in neonates. It seems to be of importance for neonatal adaptation by regulating cardiovascular, respiratory, and metabolic homeostasis(1–5).
The sympathoadrenal system is thus of great importance for neonatal mammals. However, it does not reach full maturity during the neonatal period but undergoes slow maturation that lasts for several weeks in rats(6–10) and for several years in human children(11). Environmental factors present during this development period might alter the maturation of the sympathetic nervous system and have significant consequences for successful postnatal adaptation and cardiorespiratory control throughout the individual's entire life(12). One such environmental disturbance, chronic hypoxia, often occurs during the fetal and neonatal life of human babies. Acute or chronic hypoxia occurs during delivery and under conditions such as recurrent apnea of prematurity, obstructive sleep apnea, and bronchopulmonary dysplasia(13). There are some indication that SIDS is preceded by chronic hypoxemia(14–16).
Studies on alterations resulting from mild neonatal hypoxia are scarce. Available reports deal rather with acute exposure to hypoxia(17, 18) or with hypoxic-ischemic encephalopathy after acute perinatal asphyxia(19). Exposing newborn rats to acute or prolonged hypoxia during the neonatal period elicits delayed disturbances in behavior(20), in ventilation and blood pressure(21, 22), in pulmonary arterial pressure and right ventricle mass(23), and in catecholaminergic activity of certain peripheral and central structures(18, 20, 24–27). More precisely, acute hypoxia experienced at birth delays the maturation of peripheral chemosensitivity(25) and of central nervous processes involved in respiratory events(21) and elicits a long lasting selective increase in the turnover rates of norepinephrine and dopamine in the midbrain and brainstem(18). Early postnatal prolonged hypoxia induced long lasting effects on cardiorespiratory parameters(22), on the dopamine release rate from striatum slices(20), and on the neurochemistry of catecholaminergic areas(27) involved in cardiorespiratory events.
Previous work in our laboratory, conducted in adult rats, has evidenced that long-term exposure to hypoxia (10% O2) alters the neurochemical activity of both central(28, 29) and peripheral(30–33) catecholaminergic areas,i.e. of the afferent (carotid bodies, noradrenergic cell groups of the brainstem) and efferent (sympathetic ganglia and their sympathetic target organs, adrenals) nervous pathways involved in the chemoreflex response and in the subsequent cardiorespiratory adaptation. Therefore, the hypothesis is that hypoxia occurring during neonatal life may alter the development of these immature pathways of prime importance to the cardiorespiratory function(34), thus contributing to the long-term cardiorespiratory disturbances elicited by neonatal hypoxia(22). In fact, it has been recently suggested that the perinatal period may exert a long-term influence on the development of the cardiovascular system and hence on the risk of cardiovascular disease. Oxygen deficiency might be one factor that alters cardiovascular development(35). According to the Barker concept of early programming(12), the primary aim of this study was to define whether the neurochemical activity of the autonomic nervous system controlling cardiorespiratory functions may be altered after long-term exposure to a hypoxic environment when it occurs in the first days of postnatal life, i.e. at an immature stage of its development. The setting of this system, i.e. transmitter synthesis and release and expression of receptors, may occur during a critical maturational period of development. The influence of neonatal hypoxia on the subsequent neurochemical development of the main tissues representative of the sympathoadrenal system,i.e. sympathetic ganglia (superior cervical, stellate, and celiac-mesenteric ganglia), their main target organs (heart, lungs, and kidneys) and adrenals were examined. One-day-old male rats were exposed to mild hypoxia (10% O2) for 6 d and reared thereafter in normoxia. The levels and turnover rates of dopamine, norepinephrine, and epinephrine were evaluated in the sympathetic structures of 3- and 8-wk-old rats.
METHODS
Animals and experimental procedures. Pregnant Sprague-Dawley rats (IFFA-CREDO, France) were housed in a temperature-controlled room (24± 1 °C) with a 12-h light/dark cycle and allowed free access to food and water. At birth, female and male pups were separated and placed with different dams. The experiments were carried out using male pups that were mixed at birth and redistributed at random to nursing dams to maintain a litter size of 10-12 pups to ensure a standard nutritional status. Litters were assigned to a neonatal-hypoxic group or to a normoxic-control group, which were composed of male pups exclusively. Because randomization occurs once, each litter contributes one pup for a single biochemical or blood pressure determination.
Neonatal-hypoxic rats. One-day-old male rats were kept with their dam for 6 d in a Plexiglas chamber supplied with 10% O2 + 90% N2. The concentration of O2 inside the chamber was maintained at 10 ± 0.5%. The O2 and CO2 concentrations were measured twice a day on Servomex analyzers (Servomex Co., Norwood, MA). The CO2 level in the chamber was maintained at the basal level of room air by circulating the gas from the chamber through soda lime. Expired water was trapped in a chilled tank. After 6 d of hypoxia, the litters were taken out from the Plexiglas chamber and returned with their dams to the temperature-controlled room (24 ± 1 °C), where they were reared in normoxic room air (21% O2); the first group of neonatal-hypoxic rats was killed at 3 wk of age before weaning; the second group of neonatal-hypoxic rats was weaned at 21 d of age and killed at 8 wk of age.
Normoxic-control rats. One-day-old male rats were maintained for 6 d in the same Plexiglas chamber as the hypoxic pups, but the chamber was supplied with 21% O2. As the hypoxic pups, they were taken out with their dam from the chamber and were reared in the normoxic room air (21% O2) in a similar normoxic environment as the hypoxic pups; the first group of normoxic-control rats was killed at 3 wk of age before weaning; the second group of normoxic-control rats was weaned at 21 d of age and killed at 8 wk of age.
Measurement of the catecholamine levels and turnover rates. The turnover rates of dopamine and norepinephrine were assessed by measuring the changes in the levels of dopamine and norepinephrine after blocking catecholamine biosynthesis by an intraperitoneal injection of AMPT (Sigma Chemical Co., Saint Quentin Fallavier, France; 250 mg/kg, 2.5 h before sacrifice), as previously described(25, 36). Each experimental group was divided into two half groups: one receiving AMPT, the other receiving the same volume of 0.9% NaCl 2.5 h before sacrifice. The turnover rate was calculated by multiplying the content of dopamine or norepinephrine in saline-treated rats by the slope of the regression line depicting the decrease in amine after AMPT administration and was expressed as picomoles/structure/h or picomoles/pair/h.
Rats were killed by cervical dislocation, after which adrenal glands, superior cervical, stellate, and celiac-mesenteric ganglia, and heart, lungs, and kidneys were rapidly dissected out and frozen at -80 °C. These sympathetic structures were prepared for catecholamine assays using HPLC coupled with electrochemical detection(33, 36, 37). Ganglia were disrupted ultrasonically at 4 °C in 0.1 M perchloric acid containing 2.7 mM disodium EDTA (400 μL for the right and left superior cervical ganglia, 200 μL for the left stellate ganglion, 200 μL for the right celiac-mesenteric ganglion). After centrifugation for 10 min at 8800 × g, 10 μL of the supernatant were injected onto the chromatograph.
Right and left adrenals were sonicated in 400 μL of 0.4 M perchloric acid containing 2.7 mM EDTA and dihydroxybenzylamine (0.01 nmol) as an internal standard. After centrifugation for 10 min at 8800 ×g, the supernatant was diluted 50-fold with 0.2 M acetic acid, and 10 μL were injected onto the chromatograph.
Heart, kidneys, and lungs were homogenized with a Polytron at 4 °C in 5 mL of 0.4 M perchloric acid containing 2.7 mM EDTA and dihydroxybenzylamine(0.09 nmol) as an internal standard. Excess perchloric acid was precipitated with 400 μL of potassium hydroxide/formic acid solution (7.7 M/6 M), and the homogenate was then centrifuged for 10 min at 8800 × g. The resulting supernatant (0.5 mL, diluted to 1 mL with bidistilled water for heart and kidneys; 1 mL for lungs) was purified on alumina in an Eppendorf tube containing 20 mg of purified alumina, 100 μL of 0.04 M sodium metabisulfite, and 0.5 mL of 2.8 M Tris buffer, pH 9.3. After agitation for 15 min and removal of the supernatant, the alumina was washed three times with 1 mL of 14 mM Tris buffer containing 2.7 mM EDTA. Catecholamines were eluted with 300 μL of 0.33 M acetic acid containing 0.68 mM EDTA and 0.12 mM sodium metabisulfite, and aliquots of the eluate (20 μL) were assayed using HPLC-electrochemical detection(37).
Blood pressure measurement. Blood pressure was measured at the age of 6 wk in control-normoxic rats (n = 6) and in neonatal-hypoxic rats (n = 6). Measurements were conducted on these animals while they were awake between 1000 h and noon, using an inflatable tail-cuff and photoelectric sensor(38). The average of at least three measurements was used as baseline control blood pressure and as neonatal hypoxic blood pressure. Results were expressed as mm Hg. Blood pressure recordings were performed at 6 wk, when the rats had recovered from handling and before they were killed for catecholamine analysis at 8 wk. Furthermore, the inflatable tail-cuff technique was not suitable for measurement of the blood pressure in 3-wk-old rats, and 6 wk of age was chosen as a compromise.
Statistical analysis. Data are presented as the mean ± SEM. Statistical analyses were conducted according to previous published developmental studies(39, 40). Before statistical evaluation by ANOVA, values were subjected to log transformation to reduce the heterogeneity of variance. All studies were multivariate (treatment, age, tissues, amine type) so that data were analyzed with global ANOVA. Where significant effect of treatment was detected, subsequent two-way ANOVA was carried out to assess the interaction treatment × tissue, or the interaction treatment × amine type. For the developmental normoxic results in ganglia, data were tested with three-factor ANOVA with factors of age, amine type, and tissue. Where the interaction was significant, the post hoc test (Fisher's PLSD) was applied for individual group comparison. A p value ≤0.05 was considered statistically significant.
Ethics. Surgical and experimental procedures were approved by the French (Ministère de l'Agriculture) and EEC Council Directives for care of laboratory animals.
RESULTS
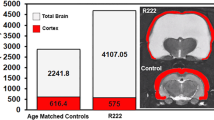
Body and tissue weights. Exposure to neonatal hypoxia had an effect on body weight and on most on the sympathetic tissues(Table 1). At 3 and 8 wk of age, the body weights of the neonatal-hypoxic rats were reduced and set at 76 ± 1% and 89 ± 2%, respectively, of the normoxic age-matched controls.
At 3 wk of age, no significant differences between the neonatal-hypoxic and the normoxic-control groups were observed with respect to the weights of adrenals and heart. At 8 wk of age, the weights of the adrenals, heart, and lungs of neonatal-hypoxic rats were reduced significantly by 10-18%, but the weight of kidneys remained unaltered (Table 1).
Blood pressure. At 6 wk of age, the blood pressure was the same in the normoxic-control rats (121 ± 3 mm Hg) as in the neonatal-hypoxic rats (120 ± 3 mm Hg).
Sympathetic ganglia. Multifactor ANOVA (factor of treatment, tissue, age, amine type) indicates a significant effect of neonatal hypoxia on the contents and turnover rates of catecholamines in sympathetic ganglia (main treatment effect) (p < 0.05). More specifically, considered at separate ages, exposure of newborn rats to hypoxia for 6 d reduced the turnover rate of norepinephrine in the superior cervical, stellate, and celiac-mesenteric ganglia of 3-wk-old rats to 64.6 ± 5.3%, 77.5± 3.4%, and 76 ± 5%, respectively, of the normoxic-control values. In contrast, the turnover rate of dopamine in these ganglia of 3-wk-old rats was unaffected by neonatal hypoxia (Fig. 1). In the 8-wk-old rats, the turnover rate of norepinephrine remained significantly reduced only in the superior cervical and stellate ganglia of neonatal-hypoxic rats (Fig. 2); no interaction of treatment × tissue was observed at this age. The turnover of dopamine remained unaltered in these three ganglia. As to concern the contents of norepinephrine and dopamine (Table 2), the changes were similar to the turnover alteration (Figs. 1 and 2), except for the norepinephrine content in the celiac-mesenteric ganglion, which was unaltered at 3 wk of age.
Effects of neonatal exposure to hypoxia (10% O2) for 6 d from 24 h after birth on the turnover rates of norepinephrine(NE) and dopamine (DA) in the superior cervical, stellate, and celiac-mesenteric ganglia of 3-wk-old rats. The columns and bars represent means ± 1 SEM for 20 normoxic-control rats and 20 neonatal-hypoxic rats. Data are expressed as picomoles of norepinephrine or dopamine per ganglion per h. ANOVA performed on log transformed data indicates a significant effect of neonatal hypoxia and no interaction of treatment × tissue and treatment × amine type. *Statistically significant differences from normoxic control data for each amine, assessed by a PLSD Fisher test (p < 0.05).
Effects of neonatal exposure to hypoxia (10% O2) for 6 d from 24 h after birth on the turnover rates of norepinephrine(NE) and dopamine (DA) in the superior cervical, stellate, and celiac-mesenteric ganglia of 8-wk-old rats. The columns and bars represent means ± 1 SEM for 20 normoxic-control rats and 20 neonatal-hypoxic rats. Data are expressed as picomoles of norepinephrine or dopamine per ganglion per h. ANOVA performed on log transformed data indicates a significant effect of neonatal hypoxia and no interaction of treatment × tissue and treatment × amine type. *Statistically significant differences from normoxic control data for each amine, assessed by a PLSD Fisher test (p < 0.05).
In the superior cervical ganglion, the effect of neonatal hypoxia on norepinephrine versus dopamine was different as shown by the significant interaction of treatment × amine type regardless of the postnatal age (p < 0.05).
Adrenal glands. Neonatal hypoxic exposure had a significant effect on the adrenal content and turnover rate of dopamine, which were significantly decreased (p < 0.05) at 3 and 8 wk(Table 3).
Heart, lungs, and kidneys. Neonatal hypoxic exposure produced an overall reduction in the content and turnover rate of norepinephrine in sympathetic target tissues (main treatment effect, p < 0.05). At 3 wk of age, only the heart was analyzed, and the content and turnover of norepinephrine was highly reduced (Fig. 3). At 8 wk of age, the content and turnover of norepinephrine decreased in heart and lungs, whereas hypoxia failed to induce a significant effect in kidneys (Fig. 3,Table 4). However, no significant interaction of treatment × tissue was observed.
Effects of neonatal exposure to hypoxia (10% O2) for 6 d from 24 h after birth on the content (nanomoles) and turnover rate(nanomoles/h) of norepinephrine (NE) in the heart of 3- and 8-wk-old rats. The columns and bars represent means ± 1 SEM for normoxic-control and neonatal-hypoxic rats. Ten control and 10 neonatal-hypoxic rats were used for the determination of the content of norepinephrine, and 20 control and 20 neonatal-hypoxic rats were used for the determination of the rate of norepinephrine turnover. Data are expressed as nanomoles of norepinephrine per heart for the content and as nanomoles of norepinephrine per heart per h for the turnover rate. ANOVA performed on log transformed data across both ages indicates an effect of neonatal hypoxia. *Statistically significant differences from normoxic control data, assessed by a PLSD Fisher test(p < 0.05).
Age-related catecholamine contents and turnover rates in sympathetic ganglia of normoxic control rats. As shown in Table 5, three-factor ANOVA (factors of age, tissue, and amine type) indicated that the postnatal age had an overall effect on the content and turnover rates of catecholamines in sympathetic ganglia(p < 0.05). This effect of age was dependent on the amine type(norepinephrine or dopamine) (interaction of age × amine type,p < 0.05) and on the tissue (interaction of age × tissue,p < 0.05). The interaction of age × amine type was significant for the superior cervical and stellate ganglia: in these ganglia the contents and/or the turnover rates of dopamine were essentially similar for 3- and 8-wk-old rats, i.e. these parameters did not change during this phase of development, whereas the contents and turnover rates of norepinephrine were significantly higher in the 8-wk-old rats than in the 3-wk-old rats.
DISCUSSION
The purpose of this study was to evaluate the long-term consequences of neonatal hypoxia on the neurochemical activity of the sympathoadrenal system in the rat. The results indicate that neonatal exposure to moderate hypoxia for 6 d, starting 24 h after birth, induced alterations in the development of the sympathoadrenal system. The main effect of this neonatal hypoxia was a long-term decrease in the neurochemical activity in sympathetic ganglia and innervated target organs as well as in the adrenal medulla.
In this study only male pups were included to eliminate the influence of gender. In fact, sex-related differences of neonatal asphyxia have been reported on body growth and norepinephrine synthesis in the brain, with male animals being more sensitive than females(41). In addition, most of the literature data on hypoxia in adult rats deal with male animals. Furthermore, these biochemical findings on male neonates might have some significance for human pathology in light of the fact that early schizophrenic illness, infantile autism, and SIDS occur with a greater frequency in boys than in girls.
One-day-old pups were exposed to moderate hypoxia (10% O2) for 6 d. This period of life is considered to be a critical time in the rat, because of the immaturity of the autonomic nervous system and the subsequent development of neural functions(20, 34). All the pups survived the exposure to hypoxia but 5-10% died during the first days after the return to normoxia. This early hypoxic exposure had long-term somatic consequences, such as persistent disturbance of growth and reduction in the weight of adrenals, heart, and lungs. Our results extend previous findings(42–44) to adrenals.
The neurochemical consequences of neonatal hypoxia for the sympathetic ganglia were a long-term overall effect that was not dependent on the type of ganglion. For the superior cervical, stellate, and celiac-mesenteric ganglia, the effect was pronounced decreases in the content and/or turnover rate of norepinephrine at 3 wk of age (Fig. 1,Table 2). This change persisted until at least 8 wk for the superior and stellate ganglia (Fig. 2,Table 2). In contrast, the content and turnover rate of dopamine were never altered after neonatal hypoxia in any of the ganglia at either of the postnatal ages examined (Figs. 1 and 2,Table 2).
In the superior cervical ganglion, the effect of neonatal hypoxia was dependent on the type of amine (significant interaction of treatment × amine type). The differential effect of neonatal hypoxia on dopaminergic and noradrenergic activity in the superior cervical ganglion may be a reflection of the storage of dopamine and norepinephrine in different cells. In fact, in the adult superior cervical ganglion, catecholamines are synthesized and stored in two distinct cell populations, the major of these being the noradrenergic cell bodies of the principal neurons, whereas the other is the SIF cells, which synthesize dopamine as a final neurotransmitter(45, 46). In adult rats the SIF cells synthesize and store half of the total ganglionic dopamine and appear to be true chemosensitive elements, responding to hypoxia by increasing specifically the content and turnover rate of dopamine and by increasing their number(47). Morphologically, the first week of postnatal life is a critical period for the two ganglionic cell populations, i.e. SIF cells and principal neurons(48–50). In light of these morphologic and biochemical considerations, our results suggest that neonatal hypoxia is able to alter the maturation of the superior cervical ganglion by selectively affecting the noradrenergic principal neurons, but not the dopaminergic SIF cells. The observed decrease in the content and turnover rate of norepinephrine in the superior cervical ganglion at 3 and 8 wk of age might lead to a feed-back increase in the content and turnover rate of dopamine that could offset the main effect of a decrease caused by hypoxia. However, this down-regulation may be disregarded because this mechanism refers only to dopamine as a precursor of norepinephrine. In any case, appropriate immunocytochemical studies of ganglia using tyrosine hydroxylase (EC 1.14.16.2) immunoreactivity have to be done to visualize the differential effect of neonatal hypoxia on noradrenergic cell bodies and dopaminergic SIF cells. Accordingly, a protective or even stimulating effect of neonatal hypoxia on the tyrosine hydroxylase activity(51) and on the number of tyrosine hydroxylase-positive fibers(24) has been demonstrated in central dopaminergic areas.
Moreover, the present study showed a differential development of dopamine versus norepinephrine in ganglia with a significant interaction of age × amine type for the superior cervical and stellate ganglia(Table 5). In the normoxic-control superior cervical and stellate ganglia, the content and/or turnover rate of dopamine attains an adult profile at 3 wk of age, whereas the content and turnover rate of norepinephrine increased significantly during the period of 3-8 wk of age. This may suggest that the dopaminergic pool matures earlier than the noradrenergic one, at least in these two ganglia.
The activity of the adrenals remains reduced until after puberty, after neonatal exposure to hypoxia (main treatment effect). This was reflected in decreases in the content and in the turnover rate of dopamine. The significant interaction of treatment × amine type supports the reliability of dopamine as an index of adrenal activity reported earlier(33, 52). The low turnover rates and the large endogenous stores of adrenal norepinephrine and epinephrine could offset the effect of treatment.
The adrenals are immature at birth(3, 39), and despite the absence of functional neuronal connections until 10 d of age, they are able to release catecholamines directly in response to acute hypoxia(17, 53). However, the recovery of adrenal catecholamine stores after their depletion requires a long time (2 wk), because of the lack of functional innervation of this gland. Our results indicate that the hypoxia-induced release of adrenal catecholamines, useful for surviving the stress of neonatal hypoxia(5, 54), is not associated with an increase in adrenal activity. In addition, this long lasting neurochemical deficiency in the adrenals as a consequence of neonatal hypoxia may alter the capacity of this organ to respond to other stressful situations during infancy or adulthood and may thus be of importance in human pathology. Accordingly, preterm human neonates who have had respiratory disorders present a lack of adrenal response to environmental stress(55).
In the target organs, neonatal hypoxia elicited a long lasting decrease(main treatment effect) in the turnover rate of norepinephrine, which is significant in the heart (Fig. 4) and lungs (Table 4) but not in the kidneys (Table 4). However, we did not detect a tissue-dependent effect of neonatal hypoxia in sympathetic target organs. The autonomic innervation of the rat heart and lungs is immature at birth, and the first 3 wk of life are considered to be the most important developmental period in cardiovascular events(10). In showing that exposure to hypoxia during the 1st wk of life alters postnatal development of the cardiac and pulmonary noradrenergic neurons, our results suggest that such neonatal hypoxia may alter the development and/or the function of the cardiorespiratory system.
The extended and long-term neurochemical alteration of the autonomic nervous system might have several physiopathologic consequences. The known long-term consequences of neonatal exposure to hypoxia are increased ventilation and very small rise in blood pressure in 50-d-old rats(22, 56), increased pulmonary vascular resistance, and pulmonary arterial pressure(23) with normal arterial Po2 values(22). However, using the same experimental protocol as Okubo and Mortola(22) we found no alteration in the blood pressure at 6 wk of age, thus suggesting that the rats were too young (42 d) to soon demonstrate modification of the blood pressure which might be thus age-dependent. This point is of importance, considering the fact that factors which impair growth during critical periods of early development may permanently affect, late in life, the structure and physiology of a range of tissues, including blood vessels(57). Retardation of intrauterine growth in the guinea pig causes long-term elevation of blood pressure(58), and it is now suggested that, in humans, low rates of fetal and infant growth may be associated with an increased risk for the development of coronary heart disease and hypertension as an adult(57).
Furthermore, the deficient sympathoadrenal activity could lead to a deficient adaptive response to metabolic, energetic, and cardiorespiratory demand. In neonates and infants, critical situations induce apnea and bradycardia, which are overcome in most cases by mobilization of the sympathoadrenal system and involvement of catecholamines. Adrenalectomized or phentolamine-treated rats were not able to perform cardiovascular and respiratory adjustments during hypoxia or anoxia, and consequently the vagal tone dominates with bradycardia(54). Our results take on particular significance in relationship to SIDS, if we assume, as proposed by Filiano and Kinney(59), that SIDS occurs at the intersection of three overlapping factors: an exogenous stressor, a critical developmental period, and a vulnerability of the infant. In this context, smoking in pregnancy may represent an exogenous stressor, too, contributing to fetal hypoxia by reducing the fetoplacental blood. Maternal cigarette smoking increased the risk of SIDS(60), adversely affected the autonomic function(61), and delayed the development of central and peripheral catecholaminergic system(40).
With regard to the mechanisms involved in the decreased catecholamine activity in the young adult after hypoxic exposure in the neonatal period, part of the integrated processes and/or cellular events might be evoked. The main mechanism could be an overall adaptative response to hypoxia to reduce metabolism. In fact, it is well established that fetal and/or neonatal starvation reduces metabolism and insulin sensitivity to save calories. As a consequence, a long lasting decrease in the sympathoadrenal activity was observed in human(62) or rat pups(39) fed with a low caloric diet. A similar mechanism could be involved in the saving of O2 to maintain the energetic balance and life of vital organs. This might lead to an altered setting of the autonomic nervous system with regard to cardiorespiratory control,i.e. norepinephrine release and receptor sensitivity(63), thus resulting in a disturbed control of homeostatis in the adult and, at least, in the “metabolic programming”(57). As to cellular events, oxygen-derived free radicals were implicated in hypoxia- and reoxygenation-induced neuron injury during nervous development(64). Programmed cell death induced by reoxygenation after hypoxia(65) should be considered as a possible cellular mechanisms involved in the decrease in the turnover rate and especially in the content of catecholamines in the sympathetic tissues described in this report.
In conclusion, the neurochemical activities of the main structures of the autonomic nervous system are altered after neonatal exposure of rats to hypoxia. If neonatal hypoxia occurs during a critical period of development(the 1st wk of life), it induces a long lasting decrease in the activity of the sympathoadrenal system during childhood and at least until adulthood is reached. These results indicate an alteration in the maturation of the peripheral catecholaminergic system as a consequence of neonatal hypoxia. Our findings may have functional implications with respect to the possibility that the critical period of development is a “programming” period for adult cardiovascular and metabolic diseases(57).
Abbreviations
- AMPT:
-
α-methyl-p-tyrosine
- ANOVA:
-
analysis of variance
- PLSD:
-
protected least square difference
- SIDS:
-
sudden infant death syndrome
- SIF:
-
small, intensely fluorescent
References
Seidler FJ, Slotkin TA 1985 Adrenomedullary function in the neonatal rat: response to acute hypoxia. J Physiol 58: 1–16.
Lagercrantz H, Slotkin TA 1986 The stress of being born. Sci Am 254: 100–107.
Slotkin TA, Seidler FJ 1988 Adrenomedullary catecholamine release in the fetus and newborn: secretory mechanisms and their role in stress and survival. J Dev Physiol 10: 1–16.
Padbury JF 1989 Functional maturation of the adrenal medulla and peripheral sympathetic nervous system. Bailliere's Clin Endocrinol Metab 3: 689–705.
Lagercrantz H 1996 Stress, arousal and gene activation at birth. News Physiol Sci 11: 214–218.
Slotkin TA 1986 Development of the sympathoadrenal axis. In: Gootman PM (ed) Developmental Neurobiology of the Autonomic Nervous System. Humana Press, Clifton, NJ, pp 69–96.
Bartolomé J, Lau C, Slotkin TA 1977 Development of the sympathoadrenal axis. In: Gootman PM (ed) Developmental Neurobiology of the Autonomic Nervous System. J Pharmacol Exp Ther 202: 510–518.
Bartolomé J, Mills E, Lau C, Slotkin TA 1980 Maturation of sympathetic neurotransmission in the rat heart. V. Development of baroreceptor control of sympathetic tone. J Pharmacol Exp Ther 215: 596–600.
Kirby RF, Mc Carty R 1987 Ontogeny of functional sympathetic innervation to the heart and adrenal medulla in the preweanling rat. J Auton Nerv Syst 19: 67–75.
Slavikova J, Goldstein M, Dahlström A 1993 The postnatal development of tyrosine hydroxylase immunoreactive nerves in the rat atrium studied with immunofluorescence and confocal laser microscopy. J Auton Nerv Syst 43: 159–170.
Dalmaz Y, Peyrin L, Sann L, Dutruge J 1979 Age-related changes in catecholamine metabolites of human urine from birth to adulthood. J Neural Transm 46: 153–174.
Barker DJP, Fall CHD 1993 Fetal and infant origins of cardiovascular disease. Arch Dis Child 68: 797–799.
Ballard PL 1986 Hormones and Lung Maturation. Springer Verlag, Berlin
Naeye RL 1989 Sudden Infant Death. Sci Am 242: 52–62.
Haque AK, Mancuso MG 1993 Proliferation of dendritic cells in the bronchioles of sudden infant death syndrome victims. Mod Pathol 6: 360–370.
Rognum TO, Saugstad OD 1993 Biochemical and immunological studies in SIDS victims. Clues to understanding the death mechanism. Acta Paediatr Suppl 389: 82–85.
Seidler FJ, Slotkin TA 1986 Ontogeny of adrenomedullary responses to hypoxia and hypoglycemia: role of splanchnic innervation. Brain Res Bull 16: 11–14.
Seidler FJ, Slotkin TA 1990 Effects of acute hypoxia on neonatal rat brain: regionally selective, long-term alterations in catecholamine levels and turnover. Brain Res Bull 24: 157–161.
Rorke LB 1992 Anatomical features of the developing brain implicated in the pathogenesis of hypoxic-ischemic injury. Brain Res 2: 211–221.
Gross J, Lun A, Berndt C 1993 Early postnatal hypoxia induces long-term changes in the dopaminergic system in rat. J Neural Transm 93: 109–121.
Eden GH, Hanson MA 1987 Effects of chronic hypoxia from birth on the ventilatory response to acute hypoxia in the newborn rat. J Physiol 392: 11–19.
Okubo S, Mortola JP 1990 Control of ventilation in adult rats hypoxic in the neonatal period. Am J Physiol 259:R836–R841.
Hakim TS, Mortola JP 1990 Pulmonary vascular resistance in adult rats exposed to hypoxia in the neonatal period. Can J Pharmacol 68: 419–424.
Bjelke B, Andersson K, Ögren SO, Bolme P 1991 Asphyxic lesion: proliferation of tyrosine hydroxylase-immunoreactive cell bodies in the rat substantia nigra and functional changes in dopamine neurotransmission. Brain Res 543: 1–9.
Hertzberg T, Hellström S, Holgert H, Lagercrantz H, Pequignot JM 1992 Ventilatory response to hyperoxia in newborn rat born in hypoxia-possible relationship to carotid body dopamine. J Physiol 456: 645–654.
Lagercrantz H, Pequignot JM, Pequignot J, Peyrin L 1992 The first breaths of air stimulate the noradrenaline turnover in the brain of newborn rat. Acta Physiol Scand 38: 21–28.
Dalmaz Y, Soulier V, Pequignot JM, Cottet-Emard JM, Lagercrantz H. 1995 Neonatal hypoxia and catecholaminergic systems in rats: altered cardiorespiratory control relevant to SIDS? In: Rognum TO (ed) Sudden Infant Death Syndrome. New Trends in the Nineties. Scandinavian University Press, Oslo, pp 242–245.
Soulier V, Cottet-Emard JM, Pequignot J, Hanchin F, Peyrin L, Pequignot JM 1992 Differential effects of long-term hypoxia on norepinephrine turnover in brain stem cell groups. J Appl Physiol 73: 1810–1814.
Pequignot JM, Soulier V., Cottet-Emard JM, Dalmaz Y, Borghini N, Peyrin L 1993 Stimulatory effect of long-term hypoxia on the posterior part of A2 noradrenergic cell group in nucleus tractus solitarius of rat. In: Data PG, Acker H, Lahiri S (eds) Neurobiology and Cell Physiology of Chemoreception. Plenum Press, New York, pp 429–434.
Dalmaz Y, Pequignot JM, Cottet-Emard JM, Peyrin L 1987 Sustained enhancement of the catecholamine dynamics in rat carotid bodies, adrenals, sympathetic ganglia and target organs during long-term hypoxia. Biomed Biochim Acta 46: 899–902.
Pequignot JM, Cottet-Emard JM, Dalmaz Y, De Haut de Sigy M, Peyrin L 1987 Dopamine and norepinephrine dynamics in rat carotid body during long-term hypoxia. J Auton Nerv System 21: 9–14.
Dalmaz Y, Pequignot JM, Cottet-Emard JM, Tavitian E, Peyrin L 1989 Changes of dopamine, norepinephrine and epinephrine turnover in sympathetic tissues after long-term hypoxic stress. In: Van Loon GR, Kvetnansky R, McCarty R, Axelrod J (eds) Stress: Neurochemical and Humoral Mechanisms. Gordon & Breach, New York, pp 277–285.
Dalmaz Y, Pequignot JM, Cottet-Emard JM, Peyrin L 1994 Adrenal response to long-term hypoxia is still increased after carotid body denervation in rat. J Appl Physiol 76: 1049–1054.
Gootman PM 1986 Development of central autonomic regulation of cardiovascular function. In: Gootman PM (ed) Developmental Neurobiology of the Autonomic Nervous System. Humana Press, Clifton, NJ, pp 279–325.
Barker DJP, Osmond C, Golding J, Kuh D, Wadsworth MEJ 1989 Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. BMJ 298: 564–567.
Dalmaz Y, Pequignot JM, Tavitian E, Cottet-Emard JM, Peyrin L 1988 Long-term hypoxia increases the turnover of dopamine but not norepinephrine in rat sympathetic ganglia. J Auton Nerv Syst 24: 57–64.
Favre-Maurice R, De Haut M, Dalmaz Y, Peyrin L 1992 Differential effect of guanethidine on dopamine and norepinephrine in rat peripheral tissues. J Neural Transm 88: 115–126.
Pfeffer JM, Pfeffer MA, Frohlich ED 1971 Validity of an indirect tail-cuff method for determining systolic arterial pressure in unanesthetized normotensive and spontaneously hypertensive rats. J Lab Clin Med 78: 957–962.
Lau C, Seidler FJ, Cameron AM, Navarro HA, Bell JM, Bartolome J, Slotkin TA 1988 Nutritional influences on adrenal chromaffin cell development: comparison with central neurons. Pediatr Res 24: 583–587.
Navarro HA, Seidler FJ, Whitmore WL, Slotkin TA 1988 Prenatal exposure to nicotine via maternal infusions: effects on development of catecholamine systems. J Pharmacol Exp Ther 244: 940–944.
Simon N, Volicer L 1976 Neonatal asphyxia in the rat: greater vulnerability of males and persistent effect on brain monoamine synthesis. J Neurochem 26: 893–900.
Mortola JP, Morgan CA, Virgona V 1986 Respiratory adaptation to chronic hypoxia in newborn rats. J Appl Physiol 61: 1329–1336.
Penney DG, Tucker A, Bambach A 1992 Heart and lungs alterations in neonatal rats exposed to CO or high altitude. J Appl Physiol 73: 1713–1719.
Frappel PB, Mortola JP 1994 Hamsters versus rats: metabolic and ventilatory response to development in chronic hypoxia. J Appl Physiol 77: 2748–2752.
König R, Heym C 1978 Immunofluorescent localization of dopamine hydroxylase in SIF cells of the rat superior cervical ganglion. Neurosci Lett 10: 187–191.
Borghini N, Dalmaz Y, Peyrin L 1991 Effect of guanethidine on dopamine in small intensely fluorescent cells of the superior cervical ganglion of the rat. J Auton Nerv Syst 32: 13–20.
Dalmaz Y, Borghini N, Pequignot JM, Peyrin L 1990 Involvement of the dopaminergic SIF cells in rat superior cervical ganglion in response to peripheral chemoreceptor stimuli. In: Eyzaguirre C, Fidone SJ, Fitzgerald RS, Lahiri S, McDonald D (eds) Arterial Chemoreception. Springer-Verlag, New York, pp 404–418.
Bohn MC 1987 Division of small intensely fluorescent cells in neonatal rat superior cervical ganglion is inhibited by glucocorticoids. Neuroscience 20: 885–894.
Hall AK, Landis SC 1991 Principal neurons and small intensely fluorescent SIF cells in the rat superior cervical ganglion have distinct developmental histories. J Neurosci 11: 472–484.
Sejvar JJ, Landis SC, Hall AK 1993 SA-1 antigen expression in small intensely fluorescent cells is associated with proliferation. Dev Biol 157: 547–552.
Burke RE, Reches A 1991 Preserved striatal tyrosine hydroxylase activity, assessed in vivo, following neonatal hypoxia-ischemia. Dev Brain Res 61: 277–280.
Renugathan S, Missala K, Sourkes TL 1989 Central regulation of adrenal tyrosine hydroxylase: effect of induction on catecholamine levels in the adrenal medulla and plasma. J Neurochem 53: 1706–1710.
Hedner T, Bergman B, Holmgren M 1980 Adrenal catecholamines during and following hypoxia in neonatal rats. Med Biol 58: 228–231.
Lagercrantz H, Edner A, Milerad J, Runold M, Yuan SZ 1995 Development of autonomic control. In: Rognum TO (ed) Sudden Infant Death Syndrome. New Trends in the Nineties. Scandinavian University Press, Oslo, pp 213–217.
Dalmaz Y, Ariagno RL, Bellon G, Challamel MJ, Peyrin L 1991 Plasma dopamine, norepinephrine, epinephrine and DOPAC levels in preterm infants prior to and immediately after a sleep ventilation hypercarbia test. Acta Paediatr Scand 80: 1008–1013.
Okubo S, Mortola JP 1988 Long-term respiratory effects of neonatal hypoxia in the rat. J Appl Physiol 64: 952–958.
Barker DJP, Gluckman PD, Godfrey KM, Harding JE, Owens JA, Robinson JS 1993 Fetal nutrition and vascular disease in adult life. Lancet 341: 938–941.
Persson E, Jansson T 1992 Low birth weight is associated with elevated adult blood pressure in the chronically catheterised guinea-pig. Acta Physiol Scand 145: 195–196.
Filiano JJ, Kinney HC 1994 A perspective on neuropathological findings in victims of the sudden, infant death syndrome: a triple-risk model. Biol Neonate 65: 194–197.
Schoendorf KC, Kiely JL 1992 Relationship of sudden infant death syndrome to maternal smoking during and after pregnancy. Paediatrics 90: 905–908.
White M, Beckett M, O'Regan M, Matthews T 1995 The effect of maternal smoking in pregnancy on autonomic function in infants. In: Rognum TO (ed) Sudden Infant Death Syndrome. New Trends in the Nineties. Scandinavian University Press, Oslo, pp 174–176.
Sakaguchi T, Arase K, Fisler JS, Bray G 1988 Effect of starvation and food intake on sympathetic activity. Am J Physiol 225:R284–R288.
Roigas J, Roigas G, Heydeck D, Papies B 1996 prenatal hypoxia alters the postnatal development of β-adrenoceptors in the rat myocardium. Biol Neonate 69: 383–388.
Palmer C, Roberts RL, Bero C 1994 Deferoxamine posttreatment reduces ischemic brain injury in neonatal rats. Stroke 25: 1039–1045.
Rosenbaum DL, Michaelson M, Batter DK, Doshi P, Kessler JA 1994 Evidence for hypoxia- induced programmed cell death of cultured neurons. Ann Neurol 36: 864–870.
Acknowledgements
The authors thank the laboratory of Pr. Sassard, Faculté de Médecine Grange Blanche, Lyon, France, for performing the blood pressure measurements. We gratefully acknowledge the skillful technical assistance of R. Favre-Maurice, J. Pequignot, F. Beylot, and L. Boussel.
Author information
Authors and Affiliations
Additional information
Supported by grants from INSERM (CRE 93-0702), the Région Rhône-Alpes, and the Swedish Medical Research Council (grant 05234).
Rights and permissions
About this article
Cite this article
Soulier, V., Peyronnet, J., Pequignot, JM. et al. Long-Term Impairment in the Neurochemical Activity of the Sympathoadrenal System after Neonatal Hypoxia in the Rat. Pediatr Res 42, 30–38 (1997). https://doi.org/10.1203/00006450-199707000-00006
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199707000-00006
This article is cited by
-
Neonatal hypoxic insult-mediated cholinergic disturbances in the brain stem: effect of glucose, oxygen and epinephrine resuscitation
Neurological Sciences (2013)
-
Decreased GABAB receptor function in the cerebellum and brain stem of hypoxic neonatal rats: Role of glucose, oxygen and epinephrine resuscitation
Journal of Biomedical Science (2011)
-
Alterations in cortical GABAB receptors in neonatal rats exposed to hypoxic stress: role of glucose, oxygen, and epinephrine resuscitation
Molecular and Cellular Biochemistry (2010)