Abstract
The purpose of this study was to determine whether mild hypothermia after a moderate hypoxic-ischemic insult reduces the extent of brain damage. Hypoxia was achieved in newborn piglets (n = 24; age, 14-72 h) by abrupt reduction of the inspired oxygen concentration (Fio2) to the maximum concentration (≅6%) giving low amplitude (<7.0 μV) EEG. Fio2 was temporarily increased if heart rate, blood pressure, or end expiratory partial pressure of alveolar CO2 (PAco2) were markedly reduced. This intermittently resulted in EEG amplitude greater than 7 μV, the EEG traces were therefore later examined to determine the duration of low amplitude EEG. After 45 min of hypoxia, the animals were randomized to normothermia (39 °C) or hypothermia (35 °C) for 3 h. Hypothermia was achieved by applying packs containing ice water. Neurologic assessments and EEG recordings were performed regularly until 3 d when the brains were perfusion fixed. Histologic damage in cortex/white matter, cerebellum, hippocampus, basal ganglia, and thalamus was graded by a pathologist blind to treatment allocation. We found that the severity of brain damage (by histopathologic and neurologic evaluation) was not significantly different when the piglets were normothermic after hypoxia compared with the group made hypothermic. Increased duration of low amplitude EEG and seizure activity were associated with increased damage. When controlling for duration of hypoxia and excluding seizures, piglets undergoing hypothermia had ≅50% less severe histopathologic damage in cortex/white matter, cerebellum, and hippocampus than those kept normothermic. Thalamus and basal ganglia had no or minor damage. It was concluded that there was no general beneficial effect of postinsult hypothermia. However, when controlling for the duration of the insult and occurrence of seizures, hypothermia reduced the severity of brain damage. This indicates a significant neuroprotective effect of 3 h of mild hypothermia on moderate, but not severe, hypoxic-ischemic insults.
Similar content being viewed by others
Main
It is well known that hypothermia during a hypoxic and/or ischemic insult is neuroprotective(1, 2). In birth asphyxia it is impossible to institute hypothermia during the initial insult. A crucial question, which we intended to elucidate, is therefore whether hypothermia influences the extent of cerebral injury when applied after the insult. Results from experimental studies on a potentially beneficial effect of hypothermia applied after asphyxia, stroke, or cardiac arrest are still conflicting(3–13).
In the present study we tested the effect of mild hypothermia applied only after hypoxia. Newborn piglets were used because they resemble human newborns in cerebral maturation(14, 15), metabolism(16), and circulation(17, 18). We have developed a survival newborn piglet model where the insult was produced by reducing the FIO2(19). In contrast to most models of asphyxia, which include regional ischemia by vessel occlusion, the ischemic component is general and secondary to the hypoxemic cardiac depression as it is in human birth asphyxia. As there is evidence that the therapeutic potential is greater for moderate than severe insults(9, 20, 21), the main aim was to investigate moderate insults. Severe insults (defined by the occurrence of seizures after the hypoxia) were therefore to be controlled for in the analyses. Brain damage was evaluated by histopathology, neurologic examination, and EEG.
METHODS
The protocol was approved by the Norwegian Animal Research Committee. Twenty-four piglets of either sex, median age, 26 h (range, 14-72 h); and median weight, 1623 g (range, 1035-2110 g) were obtained from local farmers and kept with the sow until 3 h before the experiment started.
Full details of the methods used in the maintenance and monitoring of the piglets including the evaluation of the EEG recordings, neurologic assessment, and histologic processing of the brains have been given previously(19). Briefly, animals were halothane-anesthetized, intubated, and ventilated with Fio2 at 30% keeping end tidal halothane concentration at 1.0%, transcutaneous Sao2 above 96% and end tidal PAco2 at 4.0-5.0 kPa. Glucose (3.5-5.0%) was given at 7.5 mL kg-1 h-1 to keep blood glucose within 2-10 mM 1-1. Tympanic temperature (chromel-alumel sensor), a good indicator of cerebral temperature(22), was kept normal (38.7-39.2 °C) for newborn piglets. Baseline umbilical MABP was kept ≥5.6 kPa by giving 10-20 mL kg-1 10% human albumin if necessary. Continuous monitoring of HR, ECG, MABP, PAco2, and tympanic and rectal temperature was made, and two-channel EEG were stored on paper and/or computer.
After 30 min of stable baseline conditions, hypoxia was achieved by abrupt reduction of Fio2 to approximately 6%. For the next 45 min, Fio2 was constantly adjusted to the maximum concentration giving a low amplitude EEG signal defined as an amplitude of <7.0 μV. If severe bradycardia, hypotension, or hypocapnia occurred, indicating severe cardiovascular depression, Fio2 was temporarily increased in steps of 0.3 to 1.0%. This occasionally resulted in periods with EEG activity above 7 μV. The EEG traces were later examined, and the exact total duration of low (<7 μV) and very low (<3.5 μV) amplitude EEG was recorded. Measurements of amplitude were performed with a ruler (7.0 μV corresponding to 2 mm on the paper) by an investigator blinded to the mode of treatment.
After the insult the animals were reoxygenated with Fio2 of 100% for 30 min followed by adjustment to baseline conditions. MABP was kept above 5.3 kPa by dopamine infusion, 5-20 μg kg-1 min-1, as long as required. Halothane was discontinued after 5 h, and the piglets were extubated when spontaneous breathing was adequate.
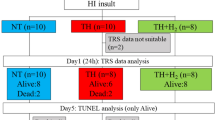
At the end of the hypoxic insult, the animals were randomized to hypothermia or normothermia. Randomization was by opening numbered sealed envelopes containing cards indicating normothermia (n = 12) or hypothermia (n = 12). When it was known that all remaining envelopes had the same treatment category, treatment was decided by a coin toss. Animals in the normothermic group were kept at a tympanic temperature between 38.7 and 39.2 °C. Animals in the hypothermic group were immediately cooled by applying ice water packs and kept between 34.7 and 35.2 °C. This mild hypothermia was sustained for 3 h before gradual rewarming to 39 °C over 90 min.
Arterial pH and blood gases (analyzed at 39 °C), hemoglobin, glucose, and lactate were measured before and after the hypoxic insult, 3 h after reoxygenation (except glucose), and later according to clinical needs. After extubation, the piglets were nursed in a cage with the target rectal temperature being 39 °C. For the first 24 h the animals continued receiving i.v. fluids only. On the 2nd d they were offered oral glucose with phased conversion to artificial pig milk formula (Baby Lactal, Peter Möller a/s, Oslo, Norway). They were bottle-fed every 2-3 h, 7-9 mL kg-1 h-1. The piglets were weighed daily. They were continuously observed, and their behavior and condition were recorded in the protocols. At intervals, EEG activity was recorded, and video recordings were made.
We have developed a neurology score(19) which was used to assess the animals neurologically from the written protocols at 6, 8, 10, 12, 24, 48, and 72 h after the insult. The score was obtained from a list of neurologic items (respiration, walking, fore limb, and hind limb function, consciousness, pathologic movements, activity level, orientation, and tonus) with normal = 2, moderately abnormal = 1, and definitely pathologic = 0. Eighteen animals were also neurologically assessed at least once from the video recordings by a neonatologist blinded to the mode of treatment.
Seizures were defined as high voltage trains of sharp waves lasting more than 30 s. Animals with a cumulative seizure duration of more than 10 min were given anticonvulsive treatment with one or more drugs (lidocaine, phenobarbital, and diazepam) as described previously(19). Absence of the cerebral circulation (or reversed diastolic flow) was confirmed by Doppler ultrasound measurement (Vingmed SD 100, Vingmed Sound A/S, Horten, Norway).
Survival was planned for 72 h when the brains were perfusion-fixed with 4% phosphate-buffered formaldehyde during deep halothane anesthesia. Regional brain damage in the cerebral cortex/white matter, the hippocampus, the basal ganglia, the thalamus, and the cerebellum were graded on a nine-step scale from 0.0 to 4.0(19) by a neuropathologist (E.M.L.) blinded to the mode of treatment. In animals dying with absent cerebral circulation before 72 h had elapsed after the insult, extensive cerebral autolysis occurred. Hence, severity and distribution of damage caused by the primary hypoxic-ischemic insult could not be evaluated in the normal way. In these animals the damage was graded as maximal (4.0) in all brain regions.
STATISTICS
Severity of histopathologic damage in cortex/white matter, cerebellum, hippocampus, basal ganglia, and thalamus in normo- versus hypothermic animals were compared using Mann-Whitney U tests. It was decided, before the series of experiments started, that seizures should be controlled for as an independent variable in the statistical analyses. Five stepwise linear regression analyses were performed with severity of brain damage in the different brain regions as dependent variable and normo- or hypothermia, duration of low amplitude EEG, seizures or no seizures, base excess at the end of the insult, and average MABP during the insult as independent variables. Visual inspection of the residual plots justified the use of the logarithm of the severity of the damage in the cortex/white matter to obtain a normal distribution of the errors.
Simple linear regression analyses were used to determine the association between histopathology and neurology and between histopathology and EEG background amplitude 3 h after the insult. Fisher's exact tests were performed to test the probability for normo- versus hypothermic animals of developing seizures and of needing dopamine. Simple logistic regression analyses were performed with seizures or no seizures as a dependent variable and pH at the end of the insult, average MABP during the insult, glucose, plasma lactate, or duration of very low amplitude (<3.5 μV) EEG as independent variables. Multiple logistic regression analysis was performed with seizures or no seizures as dependent variable and pH at the end of the insult, duration of very low amplitude EEG and normo- or hypothermia as independent variables. Mann-Whitney U tests (without correction for repeated testing) were used for comparison of the groups with respect to other parameters.
RESULTS
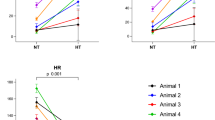
There were no differences between the normo- and the hypothermic animals in average MABP, HR, and PAco2 before or during the insult. Albumin was required in seven normo- and eight hypothermic piglets before the hypoxic insult. Significantly more hypo- than normothermic piglets required dopamine to keep MABP > 5.3 kPa after the insult (11/12 versus 4/12,p = 0.0094). Dopamine infusion was started at a median of 16 (range, 9-175) min after the insult in the hypothermic group and after a median of 76(range, 13-117) min in the normothermic group. With dopamine there was no significant difference in MABP between the hypo- and normothermic piglets posthypoxia. HR and PAco2 were lower during hypothermia (mean ± SD, 183 ± 17 versus 157 ± 17 beats min-1, 3.9± 0.2 versus 3.2 ± 0.3 kPa). All animals developed a severe metabolic acidosis with increased lactate levels during the hypoxic event, received bicarbonate, and had normal acid-base balance 3 h posthypoxia. There were no differences in blood gases, glucose, or lactate levels between normothermic and hypothermic animals at any time, and no difference in weight before the insult or weight gain during the experiment. The piglets randomized to hypothermia reached the target temperature (<35.3 °C) within median 10 (range, 8-21) min.
Histopathology (Table 1). When histopathology scores of normothermic (10 without and 2 with seizures) and hypothermic (7 without and 5 with seizures) animals were compared without controlling for other variables, there were no significant differences between the groups. However, linear stepwise regression (Table 2) demonstrated significant influence of the independent variables duration of low amplitude EEG, seizures or no seizures, and normo- or hypothermia on severity of brain damage in cortex/white matter (Fig. 1), cerebellum (Fig. 2), and hippocampus. These three variables explained 75% of the variability of damage in the cortex/white matter and 67% in the cerebellum. In the hippocampus also the average MABP during the insult had a significant influence, and the four variables explained 77% of the variability. Temperature after the insult did not significantly affect the severity of damage in the basal ganglia. In thalamus it could not be evaluated as the median histopathology scores were 0 in both groups. There were no differences between the normo- and the hypothermic group with respect to distribution of damage.
Effect of increasing duration of low amplitude EEG on severity of damage in cortex and white matter for animals kept normothermic(filled symbols) and hypothermic (open symbols) and for animals without(circles) and with (triangles) seizures. A regression line is drawn for the group of normothermic animals without seizures (filled circles). All the open circles are below this line, showing that hypothermic animals had a lower degree of damage at a given length of the insult than what would be expected in normothermic animals
One normothermic and two hypothermic animals (with seizures) did not survive beyond 48 h. They had negative diastolic cerebral blood flow velocities; at autopsy the cranial sutures were loose or showed diastasis, and the brain protruded when an incision in the dura was made, implying high intracranial pressure. Complete, irreversible ischemia results in autolysis; hence, severity and distribution of damage caused by the primary hypoxic-ischemic insult could not be evaluated. Excluding these animals did not cause significant alterations in the results of the regression analyses(results not shown).
Seizures. Five hypothermic and two normothermic animals had seizures after the insult (p = 0.2, Fisher's exact test) and received anticonvulsant drug treatment. All the animals that demonstrated both electrical and clinical seizures became severely damaged. In simple logistic regression analyses, the probability of developing seizures was positively associated with a lower pH at the end of the insult (p = 0.047) and longer duration of very low amplitude EEG during the insult (p = 0.037). The influence of normo- or hypothermia on development of seizures was not significant (p = 0.2) and was further reduced when controlling for the significant variables in a multiple logistic regression. MABP (during the insult) and plasma glucose or lactate (before or at the end of the insult) did not show significant association with seizures.
Neurology. The median neurology scores in normothermic and hypothermic animals with and without seizures from 6 to 72 h after the insults are shown in Figure 3. When evaluating all animals with and without seizures together, there was no difference between the normo- and the hypothermic group. The animals which developed seizures had significantly lower scores than the animals without seizures. Ten hours after the insult hypothermic animals without seizures had significantly higher scores than the normothermic animals without seizures (p = 0.019). The same result is obtained in a regression analysis including all animals and controlling for seizures. This was also the time when the neurology score best predicted neuropathologic outcome (R2 = 0.713, p < 0.0001). The blinded neurologic assessment from video recordings (results not shown) showed close agreement with the neurologic scores obtained from the written protocol.
Twenty piglets were extubated 50-720 min (median, 158 min) after the discontinuation of halothane, with no difference between those kept normothermic and those exposed to hypothermia. The two hypo- and one normothermic piglets in which the cerebral circulation ceased and one normothermic piglet with seizures were never extubated. All extubated piglets were able to feed from a bottle.
EEG. Three hours after the insult the background amplitude was significantly lower than baseline (median, 29; range, 5-43 μV versus median, 42; range, 27-53 μV) and it was associated with histopathologic outcome (p < 0.0001). When excluding animals with seizures, the background amplitude 3 h after the insult was higher in hypothermic than in normothermic animals (median, 42; range, 32-43 μV versus median, 29; range, 8-40 μV) (p = 0.02)(Fig. 4). Likewise, influence of temperature upon amplitude is demonstrated in a regression analysis including all animals and controlling for seizures.
DISCUSSION
In patients suffering cerebral insults, only posthypoxic treatment strategies have clinical relevance. In adult and newborn animal models, mild to moderate hypothermia applied after the insult has recently shown neuroprotection(3–9). As severe or long lasting hypothermia has well known adverse effects(23–25), establishing the shortest and mildest degree of hypothermia offering protection is important. The two newborn studies reporting protection are both on ligation models with hypothermia either being long lasting(9) or more severe(10). In our newly developed model of total hypoxia, we have examined the effect of a short (3 h) and mild (4 °C reduction) hypothermic intervention applied immediately after the insult.
This study of hypoxic-ischemic brain damage in newborn piglets did not demonstrate an ameliorating effect of 3 h of postinsult mild hypothermia. However, multiple regression analyses were performed because the groups were small, and in spite of randomization variables known or suspected to influence the severity of brain damage were not equally distributed. When epileptiform activity and the duration of low amplitude EEG were controlled for, the histopathologic damage of the brain was ≅50% less in piglets cooled to 35°C for 3 h after the insult than in piglets kept at 39 °C. The EEG background activity 3 h after the insult was also higher in the hypothermic group. Neurologic status tended to improve faster in animals that had been hypothermic.
Confounding and bias. The duration of low amplitude EEG and number of animals developing seizures were not identical in the two groups. These variables may influence the severity of brain damage and were therefore included in the regression analyses. The possibility that seizure activity is a dependent rather than an independent variable is discussed below. Base excess at the end of the insult, a variable which is often available in clinical practice, and MABP during the insult, are variables whose significance in the development of hypoxic-ischemic encephalopathy is often discussed, and they were therefore tentatively included.
After the hypoxic insult it was known to the investigators which temperature group the different piglets were in. To minimize possible bias, strict rules for treatment of hypotension and seizures, feeding, and so forth were decided in advance.
Seizures. Epileptiform activity is commonly seen after severe asphyxia(26). The 29% incidence in the present study, where all the subjects suffered severe hypoxia, strengthens the clinical relevance of the model. Five hypothermic and two normothermic animals developed seizures. This is not a significant difference. However, if the effect of hypothermia per se on development of seizures were to be evaluated, the number of animals would have had to be larger and the period of hypothermia longer.
Neonatal seizures have been shown to increase cerebral metabolic demands above energy supply and may thus cause or exacerbate cerebral injury(27, 28). Animal experiments have shown that epileptiform activity by itself produces neuronal death(29–31) and may worsen neuronal outcome after a hypoxic-ischemic insult(32–34). Also, epileptiform activity after a hypoxic-ischemic insult is likely to worsen the intracellular edema(35). Because piglets have no fontanelle and human neonates have two fontanelles and open sutures, cerebral edema would be expected to increase the intracranial pressure more in the piglet than in the newborn human.
As previous experience has indicated that the potential for treatment effects is better with moderate than severe hypoxic-ischemic insults(9, 20, 21), we primarily wanted to study moderate insults. In the present model, as in mature, human infants, the probability of developing seizures was higher the lower the pH value at the end of hypoxia(36) and the longer the duration of very low amplitude EEG, i.e. the more severe the insult.
As the seizure activity was caused by the hypoxic insult to the brain, and as the effect of postinsult mild hypothermia on the probability of developing seizures is not entirely unambiguous(37–41), it may be argued that seizures should be treated as a dependent variable. However, the evidence of a strong influence of seizures on development of brain damage and the reasonable assumption that hypothermia does not induce seizures justifies inclusion of seizures as an independent variable in the multiple regression analyses when the aim is to evaluate the effect of hypo- versus normothermia.
Neurology. Our neurologic assessment score, like encephalopathy scores for newborns(42), is associated with neuropathologic outcome particularly if performed early. After 10 h, the hypothermic animals without seizures had a significantly better neurology score than those kept normothermic. The trend of faster recovery in hypothermic animals compared with normothermic animals (without seizures) may be due to an anti-edema effect of hypothermia. Posttraumatic(37) or intraischemic(43) hypothermia reduce intracranial pressure.
EEG. In normothermic(19) as well as hypothermic piglets there was a strong association between severity of brain damage and background amplitude early after the insult. This is in accordance with studies on human newborns(44). In animals without seizures, those hypothermic compared with normothermic had higher amplitudes, indicating better cerebral function, 3 h after the insult.
From unpublished experiments we knew that the background amplitude decreases approximately 2.3 μV when newborn piglets anesthetized with 1.0% end expiratory halothane were cooled from 39 to 35 °C. However, adding 2.3μV to the measured amplitude in the hypothermic piglets in the present study did not influence any of the reported results.
Blood pressure. Newborn piglets have impaired autoregulation(45). Hypoxia causes myocardial depression and thereby hypotension. Because hypotension per se may cause brain damage, dopamine was used to keep MABP > 5.3 kPa after the insult. We have also shown that mild hypothermia has a slight hypotensive effect(22), which may explain that significantly more hypo- than normothermic piglets required dopamine.
Average MABP during the insult did not influence the severity of brain damage except in the hippocampus. From his extensive work with hypoxic-ischemic brain damage in newborn monkeys, Myers(46) suggests that slight hypotension tends to merely accentuate the tissue metabolic defects produced by the primary hypoxia. In fetal sheep subjected to one or repeated short episodes of asphyxia, the extent of neuronal loss correlated with the degree of hypotension, and one 10-min occlusion produced damage mainly in the hippocampus, whereas after repeated occlusion the damage was most severe in the striatum(34). Hippocampal damage is a recognized pattern of damage in humans after cardiac arrest, which clinically manifests itself as memory or cognitive defects(47).
Anesthesia. It has been claimed that halothane, possibly by a temperature effect, might protect against delayed neuronal death(48). Because both groups received halothane for 5 h after the insult and the temperature was controlled, this should not influence our results. Halothane reduces metabolic rate, but some cellular energy-requiring functions are being slowed to a greater degree by hypothermia than by anesthetics(49). The animals were kept anesthetized during cooling and rewarming to avoid shivering, which would increase caloric metabolic demands and myocardial work in the hypothermia group. The newborn piglet has only scarce amounts of brown adipose tissue(50) and does, unlike the newborn infant, thermoregulate by shivering.
Hypothermia. Enhörning and Westin(51) reported in 1954 that aborted human fetuses survived“much longer” when body temperature was kept at 25 °C than at 37 °C. Five years later Westin and co-workers(52) had reduced the body temperature of six severely asphyxiated newborn human infants and reported beneficial effects. Several clinical trials on asphyxiated newborn infants followed(53–58), where the protocols were similar to the one originally used by Westin et al. Babies who did not respond to conventional methods of resuscitation and/or had an Apgar score ≤3 at 5 min were subjected to hypothermia. They were placed in cold water until breathing resumed and then allowed to rewarm slowly in normal environmental temperature. None of these trials had control groups. The authors were, however, convinced that transient hypothermia in asphyxiated newborn infants was not deleterious. Furthermore, from comparing the results with mortality in asphyxiated babies not treated with hypothermia published by Drage et al.(59), their own experience, and the fact that the babies treated had already been unsuccessfully resuscitated by conventional means, the authors concluded that hypothermia reduced mortality and morbidity after asphyxia(53–58).
Several randomized controlled trials in animals have confirmed a beneficial effect of hypothermia after hypoxia/ischemia(3–10), but others have not been able to confirm this(11–13). Furthermore, optimal duration and depth of hypothermia and therapeutic time window have not been determined. Hence, further studies are still needed, and it is useful to evaluate hypothermia as a treatment in the present experimental model that, unlike most models, subjects the whole body to hypoxia, avoids vessel ligation, and develops a pattern of histopathologic damage very similar to that seen after human birth asphyxia.
Therapeutic time window, duration, and depth of hypothermia. There is evidence that prolonged and severe hypothermia may have adverse effects, as shown in animals and newborn infants(23–25). It is therefore important to find the shortest duration and mildest degree of hypothermia that is effective when the hypothermia is started without delay. There is a marked reduction in the effect of hypothermia if the onset is delayed(4–8), but a recent study obtained 70% protection, although the 24-h hypothermia period started 1 h after the insult(7). One to 3 h of postinsult hypothermia generally reduces damage. Longer periods of hypothermia give progressively increased protection(5–7). With intraischemic hypothermia, a reduction of 2 °C has been sufficient to reduce damage(60). In most studies of postinsult hypothermia, the temperature has been reduced by 5-10 °C. The present study is the only survival model with posthypoxic seizures where the effect of posthypoxic hypothermia has been examined. It is clear from our results that 3 h is too short and/or 4 °C temperature reduction is too mild for sufficient protection against severe damage.
Hypothermia-mode of action. The mechanisms by which posthypoxic hypothermia protects against hypoxic-ischemic brain damage is largely unknown. Hypothermia decreases cerebral metabolism, but this alone does not explain all of its protective effects(61). A well known result of hypothermia during an insult is the attenuated increase in glutamate(62) and thereby reduced neuronal death. Hypothermia is neuroprotective also when administered after glutamate; hence, protection is not only due to less NMDA stimulation(63). Reduced apoptosis(64), reduced brain acidosis(65), and reduced delayed energy failure(9) are other known effects of postinsult hypothermia.
Conclusion. This study does not demonstrate a general neuroprotective effect of short lasting postinsult mild hypothermia. However, when controlling for the duration of the insult and occurrence of seizures, hypothermia reduced the severity of brain damage. This indicates a significant neuroprotective effect of 3 h of mild hypothermia on moderate, but not severe, hypoxic-ischemic insults.
Abbreviations
- Fio2:
-
fraction of inspiratory oxygen
- Paco2:
-
partial pressure of alveolar CO2
- Sao2:
-
arterial oxygen saturation
- MABP:
-
mean arterial blood pressure
- HR:
-
heart rate
References
Dietrich DW, Busto R, Halley M, Valdes I 1990 The importance of brain temperature in alterations of the blood-brain barrier following cerebral ischemia. J Neuropathol Exp Neurol 49: 486–497
Laptook AR, Corbett RJT, Sterett R, Burns DK, Tollefsbol G, Garcia D 1994 Modest hypothermia provides partial neuroprotection for ischemic neonatal brain. Pediatr Res 35: 436–442
Boris-Möller F, Smith M-L, Siesjö BK 1989 Effects of hypothermia on ischemic brain damage: a comparison between preischemic and postischemic cooling. Neurosci Res Commun 5: 87–94
Busto R, Dietrich WD, Globus MYT, Ginsberg MD 1989 Postischemic moderate hypothermia inhibits CA1 hippocampal ischemic neuronal injury. Neurosci Lett 101: 299–304
Carroll M, Beek O 1992 Protection against hippocampal CA1 cell loss by postischemic hypothermia is dependent on delay of initiation and duration. Metab Brain Dis 7: 45–50
Coimbra C, Wieloch T 1994 Moderate hypothermia mitigates neuronal damage in the rat brain when initiated several hours following transient cerebral ischemia. Acta Neuropathol 87: 325–331
Colbourne F, Corbett D 1995 Delayed postischemic hypothermia: A six month survival study using behavioral and histological assessments of neuroprotection. J Neurosci 15: 7250–7260
Kuboyama K, Safar P, Radovsky A, Tisherman SA, Stezoski SW, Alexander H 1993 Delay in cooling negates the beneficial effect of mild resuscitative cerebral hypothermia after cardiac arrest in dogs: a prospective, randomized study. Crit Care Med 21: 1348–1358
Thoresen M, Penrice J, Lorek A, Wyatt J, Cady EB, Wylezinska M, Kirkbridge V, Cooper CE, Brown GC, Edwards AD, Wyatt JS, Reynolds EOR 1995 Mild hypothermia after severe transient hypoxia-ischemia ameliorates delayed cerebral energy failure in the newborn piglet. Pediatr Res 37: 667–670
Thoresen M, Bågenholm R, Løberg EM, Apricena F, Kjellmer I 1995 Posthypoxic cooling of neonatal rats provides protection against brain injury. Arch Dis Child 74:F3–F9
Dietrich WD, Busto R, Alonso O, Globus MY-T, Ginsberg MD 1993 Intraischemic but not postischemic brain hypothermia protects chronically following global forebrain ischemia in rats. J Cereb Blood Flow Metab 13: 541–549
Iwai T, Niwa M, Yamada H, Nozaki M, Tsurumi K 1993 Hypothermic prevention of the hippocampal damage following ischemia in mongolian gerbils comparison between intraischemic and brief postischemic hypothermia. Life Sci 52: 1031–1038
Yager J, Towfighi J, Vannucci RC 1993 Influence of mild hypothermia on hypoxic-ischemic brain damage in the immature rat. Pediatr Res 34: 525–529
Dickerson JWT, Dobbing J 1967 Prenatal and postnatal development of the central nervous system of the pig. R Soc Lond 384: 395
Dobbing J, Sands J 1973 Quantitative growth and development of human brain. Arch Dis Child 48: 757–767
Flecknell PA, Wootton R, John M 1982 Accurate measurement of cerebral metabolism in the conscious unrestrained neonatal piglet. Biol Neonate 41: 221–226
Haaland K, Orderud W, Thoresen M 1995 The piglet as a model for cerebral circulation-an angiographic study. Biol Neonate 68: 75–80
Buckley NM 1986 Maturation of circulatory system in three mammalian models of human development. Comp Biochem Physiol 83A: 1–7
Thoresen M, Haaland K, Løberg EM, Whitelaw A, Apricena F, Hankø E, Steen PA 1996 A piglet survival model of posthypoxic encephalopathy. Pediatr Res 40: 738–748
Ridenour TR, Warner DS, Todd MM, McAllister AC 1992 Mild hypothermia reduces infarct size resulting from temporary but not permanent focal ischemia in rats. Stroke 23: 733–738
Morikawa E, Ginsberg MD, Dietrich WD, Duncan R, Kraydich S, Globus MY, Busto R 1992 The significance of brain temperature in focal cerebral ischemia: histopathological consequences of middle cerebral artery occlusion in the rat. J Cereb Blood Flow Metab 12: 380–389
Haaland K, Steen PA, Thoresen M 1996 Cerebral, tympanic and colon thermometry in the piglet. Reprod Fertil Dev 8: 125–128
Rupp SM, Severinghaus JW 1986 Hypothermia. In: Miller RD, ed. Anesthesia, 2nd Ed. Churchill, New York, pp 1995–2022
Steen PA, Milde JH, Michenfelder JD 1980 The detrimental effects of prolonged hypothermia and rewarming in the dog. Anesthesiology 52: 224–230
Silverman WA, Fertig JW, Berger AP 1958 The influence of the thermal environment upon the survival of newly born premature infants. Pediatrics 22: 876–886
Thornberg E, Thiringer K, Odeback A, Milsom I 1995 Birth asphyxia: incidence, clinical course and outcome in a Swedish population. Acta Paediatr 84: 927–932
Younkin DP, Delivoria-Papadopoulos M, Maris J, Donlon E, Clancy R, Chance B 1986 Cerebral metabolic effects of neonatal seizures measured with in vivo 31P NMR spectroscopy. Ann Neurol 20: 513–519
Fujikawa DG, Vannucci RC, Dwyer BE, Wasterlain CG 1988 Generalized seizures deplete brain energy reserves in normoxemic newborn monkeys. Brain Res 454: 51–59
Nevander G, Ingvar M, Auer R, Siesjö BK 1985 Status epilepticus in well-oxygenated rats causes neuronal necrosis. Ann Neurol 18: 281–290
Watson GB, Rader RK, Lanthorn TH 1989 Epileptiform activity in vitro can produce long-term synaptic failure and persistent neuronal depolarization. Brain Res 498: 81–88
Meldrum BS, Brierley JB 1973 Prolonged epileptic seizures in primates. Ischemic cell change and its relation to ictal physiological events. Arch Neurol 28: 10–17
Voll CL, Auer RN 1991 Postischemic seizures and necrotizing ischemic brain damage: neuroprotective effect of postischemic diazepam and insulin. Neurology 41: 423–428
Tan WKM, Williams CE, Gunn AJ, Mallard CE, Glückman PD 1992 Suppression of postischemic epileptiform activity with MK-801 improves neural outcome in fetal sheep. Ann Neurol 32: 677–682
Mallard EC, Williams CE, Johnston BM, Gunning MI, Davis S, Glückman PD 1995 Repeated episodes of umbilical cord occlusion in fetal sheep lead to preferential damage to the striatum and sensitize the heart to further insults. Pediatr Res 37: 707–713
Williams CE, Gunn A, Glückman PD 1991 Time course of intracellular edema and epileptiform activity following prenatal cerebral ischemia in sheep. Stroke 22: 516–521
Goodwin TM, Belai I, Hernandez P, Durrand M, Paul RH 1992 Asphyxial complications in the term newborn with severe umbilical acidemia. Am J Obstet Gynecol 162: 1506–1512
Clifton GL, Allen S, Barrrodale P, Plenger P, Berry J, Koch S, Fletcher J, Hayes RL, Choi SC 1993 A phase II study of moderate hypothermia in severe brain injury. J Neurotrauma 10: 263–271
Vastola EF, Homan R, Rosen A 1969 Inhibition of focal seizures by moderate hypothermia A clinical experimental study. Arch Neurol 20: 430–439
Ferrari E, Amantea L 1955 Convulsive electrocortical discharge in hypothermic dog. Electroencephalogr Clin Neurophysiol 7: 441
Noell WK, Briller SA, Brendel WB 1952 Effects of cold exposure on brain activity. Fed Proc 11: 114
Liu Z, Gatt A, Mikati M, Holmes GL 1993 Effect of temperature on kainic acid-induced seizures. Brain Res 63: 51–58
Levene MI, Sands C, Grindulis H, Moore JR 1986 Comparison of two methods of predicting outcome in perinatal asphyxia. Lancet 1: 67–69
Karibe H, Zarow GJ, Graham SH, Weinstein PR 1994 Mild intraischemic hypothermia reduces postischemic hyperperfusion, delayed postischemic hypoperfusion, blood-brain barrier disruption, brain edema, and neuronal damage volume after temporary focal cerebral ischemia in rats. J Cereb Blood Flow Metab 14: 620–627
van Lieshout HBM, Jacobs JWFM, Rotteveel JJ, Geven W, v't Hof M 1995 The prognostic value of the EEG in asphyxiated newborns. Acta Neurol Scand 91: 203–207
Haaland K, Karlsson B, Skovlund E, Lagercrantz H, Thoresen M 1995 Postnatal development of the cerebral blood flow velocity response to changes in CO2 and mean arterial blood pressure in the piglet. Acta Paediatr 84: 1414–1420
Myers RE 1977 Experimental models of perinatal brain damage: relevance to human pathology. In: Gluck L, ed. Intrauterine Asphyxia and the Developing Brain. Year-book, Chicago, pp 37–96
Cummings JL, Tomiyasu U, Read S, Benson F 1984 Amnesia with hippocampal lesions after cardiopulmonary arrest. Neurology 34: 379–681
Warner DS, Mcfarlane C, Todd MM, Ludwig P, Mcallister AM 1993 Sevoflurane and halothane reduce focal ischemic brain damage in the rat-possible influence on thermoregulation. Anesthesiology 79: 985–992
Nakashima K, Todd MM, Warner DS 1995 The relation between cerebral metabolic rate and ischemic depolarization: a comparison of the effects of hypothermia, pentobarbital, and isoflurane. Anesthesiology 82: 1199–1208
Dauncey MJ, Wooding FBP, Ingram DL 1981 Evidence for the presence of brown adipose tissue in the pig. Res Vet Sci 31: 76–81
Enhörning G, Westin B 1954 Experimental studies of the human fetus in prolonged asphyxia. Acta Physiol Scand 31: 359–373
Westin B, Miller JA, Nyberg R, Wedenberg E 1959 Neonatal asphyxia pallida treated with hypothermia alone or with hypothermia and transfusion of oxygenated blood. Surgery 45: 868–879
Westin B, Nyberg R, Miller JA, Wedenberg E 1962 Hypothermia and transfusion with oxygenated blood in the treatment of asphyxia neonatorum. Acta Paediatr Scand 51: 1–80
Krokfors E, Pitkänen H, Hirvensalo M, Rhen K 1961 The use of hypothermia in severe neonatal asphyxia. Suomen Laakarilehti 17: 987–1004
Ehrström J, Hirvensalo M, Donner M, Hietalathi J 1969 Hypothermia in the resuscitation of severely asphyctic newborn infants. Ann Clin Res 1: 40–49
Cordey R 1964 Hypothermia in resuscitating newborns in White asphyxia. Obstet Gynecol 24: 760–767
Cordey R, Chiolero R, Miller JA 1973 Resuscitation of neonates by hypothermia: report on 20 cases with acid-base determination on 10 cases and the long-term development of 33 cases. Resuscitation 2: 169–181
Dunn JM, Miller JA 1969 Hypothermia combined with positive pressure ventilation in resuscitation of the asphyxiated neonate. Am J Obstet Gynecol 104: 58–67
Drage JS, Kennedy C, Schwarz BK 1964 The Apgar score as an index of neonatal mortality A report from the collaborative study of cerebral palsy. Obstet Gynecol 24: 222–230
Busto R, Dietrich WD, Globus MYT, Valdés I, Scheinberg P, Ginsberg MD 1987 Small differences in intraischemic brain temperature critically determine the extent of ischemic neuronal injury. J Cereb Blood Flow Metab 7: 729–738
Todd MM, Warner DS 1992 A comfortable hypothesis reevaluated. Anesthesiology 76: 161–164
Busto R, Globus MY-T, Dietrich D, Martinez E, Valdés I, Ginsberg MD 1989 Effect of mild hypothermia on ischemia-induced release of neurotransmitters and free fatty acids in rat brain. Stroke 20: 904–910
Bruno VMG, Goldberg MP, Dugan LL, Giffard RG, Choi DW 1994 Neuroprotective effect of hypothermia in cortical cultures exposed to oxygen-glucose deprivation or excitatory amino acids. J Neurochem 63: 1398–1406
Edwards AD, Yue X, Squier MV, Thoresen M, Cady E, Penrice J, Cooper C, Wyatt JS, Reynolds EOR, Mehmet H 1995 Specific inhibition of apoptosis after cerebral hypoxia-ischemia by moderate post-insult hypothermia. Biochem Biophys Res Commun 217: 1193–1199
Laptook AR, Corbett RJT, Burns D, Sterett R 1995 Neonatal ischemic neuroprotection by modest hypothermia is associated with attenuated brain acidosis. Stroke 26: 1240–1246
Acknowledgements
The authors thank Fabio Apricena for excellent technical assistance and Knut Liestøl, Andrew Whitelaw, Erik Hankø, Wenche J. Orderud, and Roger Ødegaard for their contributions.
Author information
Authors and Affiliations
Additional information
Supported by the Norwegian Research Council, the Laerdal Foundation for Acute Medicine, and the Norwegian SIDS Society.
Rights and permissions
About this article
Cite this article
Haaland, K., Løberg, E., Steen, P. et al. Posthypoxic Hypothermia in Newborn Piglets. Pediatr Res 41, 505–512 (1997). https://doi.org/10.1203/00006450-199704000-00009
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199704000-00009
This article is cited by
-
Hydrogen gas can ameliorate seizure burden during therapeutic hypothermia in asphyxiated newborn piglets
Pediatric Research (2024)
-
Opioid exposure during therapeutic hypothermia and short-term outcomes in neonatal encephalopathy
Journal of Perinatology (2022)
-
Short-term outcomes of remote ischemic postconditioning 1 h after perinatal hypoxia–ischemia in term piglets
Pediatric Research (2021)
-
Variability and sex-dependence of hypothermic neuroprotection in a rat model of neonatal hypoxic–ischaemic brain injury: a single laboratory meta-analysis
Scientific Reports (2020)
-
Association between sedation–analgesia and neurodevelopment outcomes in neonatal hypoxic-ischemic encephalopathy
Journal of Perinatology (2018)