Abstract
The role of type IV collagenases during rat bladder development and in response to partial bladder outlet obstruction was evaluated. Gelatinase gel zymography was performed on developing rat bladders (gestation d 16 and 19, at birth, 5, 10, 15, 20, 30, and 75 d postnatally), after partial obstruction of the bladder outlet in young adults and after separation of the epithelium from the mesenchyme in young adults. Bladder function was assessed by cystometry in obstructed animals. During development, the 72-kD type-IV collagenase [matrix metalloproteinase (MMP)-2, both latent and activated] was maximally expressed in the fetal period and decreased with age; whereas the 92-kD gelatinase(MMP-9) was not expressed in developing or adult bladders. MMP-2 was localized to the bladder mesenchyme and was undetectable in isolated epithelium. In 46 obstructed rats, there was an 8-fold increase in bladder volume and weight along with smooth muscle hypertrophy (mean smooth muscle cell diameter 7.09± 0.11 μm versus 4.65 ± 0.05 μm in normal animals, p < 0.001). Obstructed rats had increased quantities of latent and activated MMP-2 and MMP-9 compared with sham-operated and normal controls. These findings suggest that expression and activation of type IV collagenases (MMP-2 and 9) are developmentally regulated and play a role in bladder remodeling during developmental morphogenesis and after partial outlet obstruction.
Similar content being viewed by others
Main
During embryonic development, the bladder undergoes significant tissue remodeling as it increases in size and matures in function. In addition to maturation of smooth muscle and urothelium, much of the change in the bladder wall occurs within the ECM, which serves both structural and regulatory functions(1, 2). In the developing rat bladder, for example, before 14 d of gestation the bladder consists only of undiffer-entiated mesenchyme(3). Immediately thereafter dramatic changes occur in the morphology of both the cellular and ECM culminating in the mature bladder phenotype(3).
Similarly, the bladder wall stretches and thickens in response to pathologic conditions such as obstruction of the outlet. In humans this may occur as a result of congenital obstruction, such as posterior urethral valves, urethral atresia, and ureteroceles, or from acquired disorders, such as urethral strictures or prostatic hyperplasia and carcinoma. To compensate for this, the bladder wall thickens and becomes dilated. The main histologic feature seen in obstruction is an increase in the size of smooth muscle cells(4, 19). In addition, there are changes within the ECM affecting both the fibrillar and nonfibrillar components(5–7).
The changes occurring in the ECM of the bladder during both normal development and in response to obstruction reflect a balance of synthesis and degradation of the fibrous (mainly collagen and elastin) and nonfibrous(proteoglycans and glycosaminoglycans) constituents. Degradation of the ECM appears to be an essential part of many nonpathologic processes in other organ systems, including embryo implantation, ovulation, mammary involution after lactation, nerve regeneration, wound healing, angiogenesis, bone remodeling, and glandular morphogenesis(1, 8). Similarly, cells that undergo malignant transformation are linked to increased expression of ECM-degrading enzymes(9–11). A common characteristic in malignancy is the breaching of histologic barriers, such as the basement membrane. This is accomplished by extracellular proteolytic enzymes which degrade the ECM and facilitate cellular infiltration into surrounding tissues(13, 16). The basement membrane is the component of the ECM which provides the boundary between the bladder mesenchyme and its urothelial lining. It also serves as the boundary for blood vessels and smooth muscle. Degradation of the basement membrane also has been shown to be an essential factor in normal tracheal gland morphogenesis(8). The MMPs which mediate this degradation consist of three major subgroups: the type IV collagenases (72 and 92 kD, also referred to as MMP-2 and MMP-9, or gelatinase A and B, respectively), the interstitial collagenases, and the stromelysins.
The role of basement membrane ECM degradative enzymes, during normal bladder development and in response to the pathologic state of obstruction, is less well understood. We therefore performed zymographic analyses on normally developing rat bladders and created a model of partial bladder outlet obstruction to observe the changes in ECM proteinase activity. The results shown below suggest that 72-kD type IV collagenase facilitates ECM remodeling during bladder embryogenesis and also plays a role in modulating pathologic changes in the bladder wall after outlet obstruction.
METHODS
Partial urethral obstruction. Young adult Fischer 344 virgin rats (60 d old) underwent partial urethral obstruction after sodium pentobarbital anesthesia (50 mg/kg). A midline abdominal incision was made to expose the bladder, and a 20-gauge angiocatheter was inserted into the urethra (Fig. 1). Dissection of the retrourethral space (anterior to the vagina and distal to the bladder neck) was performed, and a 3-0 silk ligature was tied gently, yet snugly, around the urethra with the catheter in place. Sham-operated animals underwent a similar procedure with cannulation of the urethra using the angiocatheter and dissection around the urethra without placement of the silk ligature. The bladders were filled with saline, and the cannula was removed and then compressed to ensure that the obstruction was not complete.
Cystometry. Evaluation of bladder pressure was performed via a cystometric method adapted from Lundbeck et al.(14) and Malmgren et al.(15). Animals were give intraperitoneal urethane(1.5-2.0 mg/g of body weight) and placed supine on a warmed operating table (37°C). The lower abdomen was again opened, and the dome of the bladder was exposed. Polyethylene tubing (PE 50) was inserted through a small puncture in the dome of the bladder and secured in place with a suture, and the abdominal wall was closed (Fig. 2). Tubing was attached to a pressure transducer (Baxter Uniflow pressure transducer, Baxter Healthcare Corp., Irvine, CA) in the with a Harvard infusion pump (Harvard Apparatus, Millis, MA). Room temperature saline was infused at 0.1 mL/min through the pressure transducer, which was zeroed to the atmosphere during infusion. A Macintosh Power PC computer was used for data acquisition using the LabView, software program (National Instruments Corp., Austin, TX). Infusion commenced immediately after aspiration of the bladder contents. Upon infusion, capacity was determined as the volume at which leakage through the urethra occurred. The intravesical pressure at the moment of leakage was termed the leak point pressure. The bladder was emptied, the procedure repeated two additional times, and the mean value recorded.
Histology and morphometry. Animals were killed at 1, 2, and 4 wk after partial obstruction. In addition, fetal bladders were obtained from timed-pregnant Fischer 344 rats on gestational d 16 and 19. Bladders were also obtained from Fischer 344 rats at birth and 5, 10, 15, 20, 30, and 75 d postnatally. Obstructed and control bladders were weighed (dry) and measured, and volumes were calculated. Bladders of newborn rats were separated into epithelial and mesenchymal tissues. This was done by incubating in 20 mM EDTA at 37°C for 20 min. Bladders were then placed in chilled calcium and magnesium-free Hanks' medium (Sigma Chemical Co., St. Louis, MO) to stop chelation, and the epithelium was microdissected from the mesenchyme. Bladders were placed into 10% buffered formalin, processed in graded alcohol solutions and Histoclear, and paraffin-embedded. Sections (5 μm thick) were stained with Masson's trichrome and hematoxylin and eosin. Computer-assisted image analysis was performed to document changes in smooth muscle cell morphology using the Lumina camera system (Leaf Systems, Southboro, MA), a Macintosh Power PC computer, and Prizm view software (Signal Analytics Corp., Vienna, VA). Images were evaluated at 1000×, and only clearly visualized smooth muscle cells seen with a nucleus in the focal zone were used to measure cross-sectional diameters at the level of the nucleus.
Zymography. Substrate-impregnated PAGE was modified from Talhouk et al.(16). The bladders were washed and placed in serum-free medium, then transferred to a mini glass tissue grinder containing 0.5% Triton X-100 (Sigma Chemical Co.) in phosphate buffer(pH 7.8, 4°C) and homogenized. Extracts were centrifuged, and the soluble supernatant frozen on solid CO2. Equal amounts of protein were added to Laemmli SDS sample buffer and electrophoresed on a 10% SDS-polyacrylamide gel slab containing 1 mg/mL gelatin as the substrate for MMP. Prestained low molecular weight markers were run along with the protein samples. After SDS removal, slabs were incubated in a Tris-HCl buffer (pH 7.8, 37°C) for 40 h. The gels were then stained with Coomassie Blue and then destained with acetic acid. Substrate degradation was observed by the loss of staining in the region occupied by the electrophoresed proteinase. Slabs were fixed and dried, and the signals were imaged using the Lumina camera system as described.
RESULTS
Forty-eight of 59 obstructed rats were available for evaluation (survival rate = 81%), 17 at 1 wk, 15 at 2 wk, and 16 at 4 wk postsurgery. Eighteen sham-operated animals were used for comparison; 6 were killed at 1 wk, 7 at 2 wk, and 5 at 4 wk postsurgery.
Cystometry. The physiologic effects of partial urethral obstruction were documented in three randomly selected obstructed (for 2 wk) and two normal animals. Placement of the pressure cannula in the dome of the bladder enabled accurate assessment of the bladder outlet, a factor that transurethral cannula cannot assess. Obstructed animals had markedly increased bladder volume (Fig. 3 and Table 1) and elevated voiding pressures. The mean bladder pressure in obstructed animals was 90 cm H2O (range = 80-100 cm H2O) compared with 35 cm H2O(range = 30-40 cm H2O) in normal animals (Fig. 4). The cystometric results were highly reproducible on repeated assessments, confirming the reliability of this procedure to assess the degree of obstruction in the rat model.
Histomorphometry. After obstruction of the outlet, the bladder wall became thickened, and the bladder volume increased 6-7-fold (Fig. 3 and Table 1), although the cystic shape was maintained. All obstructed animals had bladder calculi, ranging from fine, sandlike material to discrete large stones in some animals obstructed for 4 wk. None of the sham-operated animals had stones, and only one had mild thickening and enlargement of the bladder, suggesting injury to the outlet at operation. In contrast, two animals killed earlier than 1 wk (due to poor thriving) had bladders that were massively dilated but without the characteristic thickening seen in bladders obstructed 1 wk of longer.
Histologically, the bladder wall responded to obstruction by increasing in thickness. This occurred mainly as a result of smooth muscle hypertrophy. Individual smooth muscle cell diameters increased significantly (7.09 ± 0.11 μm) compared with controls (4.65 ± 0.05 μm, p < 0.001) (Fig. 5 and Table 1). The amount of ECM surrounding the smooth muscle appeared to remain constant. Further, there did not appear to be fibrosis within the smooth muscle bundles themselves. There also appeared to be no increased infiltration of the bladder wall by mononuclear cells. Morphometric changes after obstruction were compared at 1, 2, and 4 wk to determine whether time-dependent alterations in smooth muscle architecture were seen. Based upon a single dimensional analysis (individual smooth muscle cell diameter), no differences among the three time points assessed could be detected.
The histologic changes during the course of rat bladder development have been described in an earlier study(3) which focused on changes in smooth muscle size and location. Immunohistochemical studies documenting the localization and quantity of type IV collagen within the urinary bladder have likewise been done(7).
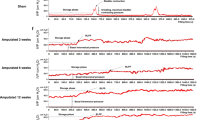
Zymography. During normal development, varying amounts of proteinases were expressed at different time periods (Fig. 6a). The 72-kD type IV collagenases (both latent MMP-2 and its activated 62-kD isoform) had their highest expression in the fetal period, appearing maximally at embryonic d 19, just before birth. The amount steadily decreased with advancing age. In contrast, MMP-9 (92 kD) was not detected until adulthood, and then only in very small amounts. After separation of the epithelium from the mesenchyme in neonatal rat bladders using EDTA and microdissection, MMP-2 localized only to the mesenchyme and not the epithelium (Fig. 6b). No MMP-9 protein expression was detectable.
After obstruction, substantial differences in the quantity of proteinase expression were noted (Fig. 6c). Most impressive was the large quantity of MMP-9 which was maximally expressed at 1 wk after ligation and much less at 2 and 4 wk postobstruction. The changes in MMP-2 after obstruction were uniform for the three time periods (1, 2, and 4 wk) assessed; although the activated form of MMP-2 (62 kD) appeared in maximal quantity early on at 1 wk and diminished gradually thereafter.
DISCUSSION
We have shown that ECM degradative enzymes are regulated during development and after partial outlet obstruction of the rodent bladder. During bladder development, the 72-kD type IV collagenase (MMP-2), and its activated 62-kD form, demonstrated its maximal expression prenatally and decreased steadily thereafter with increasing age; whereas MMP-9 was absent until after tissue injury occurred in adulthood. These findings suggest that during normal rat bladder morphogenesis, expression of type IV collagenases is developmentally regulated and affects remodeling of type IV collagen. We have previously shown that bladder development requires induction of smooth muscle by epithelium(17). This process appears to be the result of direct epithelial-stromal interactions mediated by either direct contact or via a soluble factor(s) traversing the basement membrane(17). The major constituent of the basement membrane in most organ systems is type IV collagen(1). In the bladder, Ewalt et al.(7) have clearly shown that type IV collagen localizes to smooth muscle and epithelial basement membranes. We speculate that the proteolytic action of MMP-2 on basement membrane collagen during the period of early smooth muscle formation may facilitate the epithelial-mesenchymal interactions responsible for smooth muscle morphogenesis. Further studies assessing smooth muscle differentiation with inhibitors of degradative enzymes will help to further elucidate the role of MMP-2 on early bladder development. In contrast, the role of MMP-9 in adulthood is uncertain. Its presence in the disease state suggests possible participation in mediating normal sensecent changes. Alternatively, MMP-9 may be derived from invading leukocytes, suggesting a possible role in mediating the inflammatory response.
In addition to the temporal relationship of the proteinases to the sequence of developmental events, a spatial orientation also exists. In the normal adult bladder, the activity of the MMPs was confined to the stromal component of the bladder wall. Other studies have documented the absence of 72-kD collagenase in the epithelium of most organs except developing postnatal submaxillary(18) and tracheobronchial glands(8). In the latter study, MMP-2 was found to facilitate ECM invasion of tracheal submucosal glandular epithelial cells. In contrast, the bladder epithelium does not form glandular epithelium, thus it is not surprising that the epithelium does not express MMP activity.
Obstruction of the bladder outlet caused severe disruption of the normal bladder morphology and function. The model we have developed caused reproducible outlet obstruction with consistent changes in bladder phenotype. Morphologically, the pattern of bladder wall thickening with smooth muscle hypertrophy was evident. This phenomenon has been observed in the rat by other investigators(6, 19). Our study further investigated the degree of obstruction by performing antegrade cystometry in the rats. Although the animals were able to void in all cases, the leak point pressures generated by obstructed bladders were consistently 2-3-fold higher than those in normal animals.
Zymographic analysis of the obstructed bladder showed an increase in the expressed levels of type IV collagenases, MMP-2 and MMP-9, coincidental with postobstructive bladder wall remodeling. Both the level of MMP-2 and MMP-9 expression and the level of activated MMPs were markedly increased in the obstructed bladder wall. Although not specifically documented in this study, increased deposition in ECM components, such as collagen, might lead one to expect less tissue turnover and thus, less MMP activity. This increase in ECM deposition has been demonstrated in other bladder obstruction studies, both in the human and in animals(4, 12, 18). In unpublished studies of obstructed fetal sheep, Peters showed that type IV collagenase activity was increased along with inhibition of interstitial collagenase (MMP-1), one of the key proteinases involved in the breakdown of collagen types I and III. This suggests that there is decreased collagen breakdown after obstruction of the bladder resulting in an alteration in the balance of synthesis and degradation that ultimately leads to an accumulation of collagen types I and III. The fate of type IV basement membrane collagen is not the same as for types I and III, suggesting a different role for type IV collagen. The reasons for this are unclear. We hypothesize that breakdown of the basement membrane collagen may occur to facilitate mesenchymal-epithelial interactions. The signaling between the epithelium and mesenchyme is known to be vitally important for development of bladder smooth muscle(17). The factors that mediate this signal transduction are not yet known; however, we speculate that proteinases, such as type IV collagenases, may have a role in facilitating this process by breaking down basement membrane collagen. Signaling factors, in turn, may mediate the complex structural remodeling of the bladder wall. Factors that regulate the synthesis of these basement membrane collagenases are not yet defined. Likewise, the modulators of type IV collagen synthesis remain to be elucidated and represent the subject of ongoing investigation.
CONCLUSION
We have conducted a preliminary survey of ECM-degrading proteinases in the bladder, using zymography, to determine their expression and function during development and in response to outlet obstruction. The results demonstrate that high levels of proteolytic activities are not unique to the neoplastic state but are also involved in normal physiologic development of the bladder. Enhanced degradative activities during development and obstruction involve breaching histologic barriers, such as basement membranes, to cause transient or permanent changes in the tissue architecture. Our data strongly suggest basement membrane proteolysis, in particular, is important for tissue remodeling to occur. This feature further suggests that epithelial-stromal interactions are vital for the process of tissue turnover.
Abbreviations
- ECM:
-
extracellular matrix
- MMP:
-
matrix metalloproteinases
References
Alexander CM, Werb Z 1991 Extracellular matrix degradation. In: Day ED (ed) Cell Biology of Extracellular Matrix. Plenum, New York, pp 255–302
Baskin LS, Constantinescu S, Duckett JW, Snyder HM, Macarak E 1994 Type III collagen decreases in normal fetal bovine bladder development. J Urol 152: 688–691
Baskin LS, Hayward SW, Young P, Cunha GR 1996 Ontogeny of the rat bladder: smooth muscle and epithelial differentiation. Acta Anat 155: 104–112
Uvelius B, Persson L, Mattiasson A 1984 Smooth muscle cell hypertrophy and hyperplasia in the rat detrusor after short-time infravesical outflow obstruction. J Urol 131: 173–176
Gabella G, Uvelius B 1990 Urinary bladder of rat: fine structure of normal and hypertrophic musculature. Cell Tissue Res 262: 67–79
Uvelius B, Lindner P, Mattiasson A 1991 Collagen content in the rat urinary bladder following removal of an experimental infravesical outlet obstruction. Urol Int 47: 245–249
Ewalt DH, Howard PS, Blyth B, Snyder HM, Duckett JW, Levin RM, Macarak EJ 1992 Is Iamina propria matrix responsible for normal bladder compliance?. J Urol 148: 544–549
Lim M, Elfman F, Dohrman A, Cunha GR, Basbaum C 1995 Upregulation of the 72-kDa type IV collagenase in epithelial and stromal cells during rat tracheal gland morphogenesis. Dev Biol 171: 521–530
Stetler-Stevenson WG 1990 Type IV collagenases in tumor invasion and metastasis. Cancer Metastasis Rev 9: 289–303
Stetler-Stevenson WG, Liotta LA, Kleiner DE Jr 1993 Extracellular matrix 6: role of matrix metalloproteinases in tumor invasion and metastasis. FASEB J 7: 1434–1441
Mignatti P, Rifkin DB 1993 Biology and biochemistry of proteinases in tumor invasion. Physiol Rev 73: 161–195
Kleiner DE Jr, Stetler-Stevenson WG 1993 Structural biochemistry and activation of matrix metalloproteinases. Curr Opin Cell Biol 5: 891–897
Lin CQ, Bissell MJ 1993 Multi-faceted regulation of cell differentiation by extracellular matrix. FASEB J 7: 737–743
Lundbeck F, Djurhuus JC, Vaeth M 1989 Bladder filling in mice: an experimental in vivo model to evaluate the reservoir function of the urinary bladder in a long term study. J Urol 141: 1245–1249
Malmgren A, Sjogren C, Uvelius B, Mattiasson A, Andersson KE, Andersson PO 1987 Cystometrical evaluation of bladder instability in rats with infravesical outflow obstruction. J Urol 137: 1291–1294
Talhouk RS, Bissell MJ, Werb Z 1992 Coordinated expression of extracellular matrix-degrading proteinases and their inhibitors regulates mammary epithelial function during involution. J Cell Biol 118: 1271–1282
Baskin LS, Hayward SW, Young P, Cunha GR 1996 Role of mesenchymal-epithelial interactions in bladder development. J Urol 156: 1820–1827
Reponen P, Sahlberg C, Huhtala P, Hurskainen T, Thesleff I, Tryggvason K 1992 Molecular cloning of murine 72-kD type IV collagenase and its expression during mouse development. J Biol Chem 267: 7856–7862
Mattiasson A, Uvelius B 1982 Changes in contractile properties in hypertrophic rat urinary bladder. J Urol 128: 1340–1342
Author information
Authors and Affiliations
Additional information
Supported by National Institutes of Health Grant K08 DK02397-01.
Rights and permissions
About this article
Cite this article
Sutherland, R., Baskin, L., Elfman, F. et al. The Role of Type IV Collagenases in Rat Bladder Development and Obstruction. Pediatr Res 41, 430–434 (1997). https://doi.org/10.1203/00006450-199703000-00021
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199703000-00021
This article is cited by
-
The interplay of extracellular matrix and microbiome in urothelial bladder cancer
Nature Reviews Urology (2016)
-
Advances in biomimetic regeneration of elastic matrix structures
Drug Delivery and Translational Research (2012)
-
The bladder extracellular matrix. Part I: architecture, development and disease
Nature Reviews Urology (2009)