Abstract
To identify the developmental changes in monthly urinary gonadotropin and ovarian hormone excretion, consecutive 30-d first morning void urinary specimens were collected from 36 normal girls, one normal woman, and 15 female patients with idiopathic precocious puberty. Of these children, three normal girls and three patients with precocious puberty volunteered to collect these specimens on 2-3 occasions over a time interval of 0.5-3.2 y. When sampled, six were early prepubertal, nine late prepubertal, eight early pubertal, eight mid-pubertal, and eight late pubertal normal girls, and six were early pubertal and 14 mid-pubertal patients with precocious puberty. The mean level of monthly urinary LH, FSH, and total estrogen excretions increased with pubertal maturation. In prepuberty, the mean LH level was lower than the mean FSH level, and neither showed significant episodic fluctuations. In early puberty, mean FSH levels increased with remarkable fluctuations, and mean LH levels were low with few variations in the course of a month. At the onset of puberty, gonadotropin excretory patterns underwent specific changes, showing at the same time periodically and every other day fluctuating patterns. Urinary total estrogen and pregnanediol excretion fluctuated independently from these periodic variations in urinary gonadotropins. These patterns were observed in six out of 16 patterns in normal pubertal girls and 10 out of 20 patterns in precocious puberty. Once the urine LH level exceeded the urine FSH level, however, these periodic variations disappeared. The cycle of a normal postmenarcheal girl aged 14 y showed a pattern similar to that of a normal adult. In patients with precocious puberty, the hormonal patterns were similar to those of sexual stage-matched normal girls.
Similar content being viewed by others
Main
The onset of puberty and progression of secondary sexual characteristics are controlled by the hypothalamic LHRH pulse generator(1). The LHRH neurosecretory neurons of the hypothalamic LHRH pulse generator have spontaneous autorhythmicity and act as a neuronal oscillator for the pulsatile release of LHRH. In response to pulsatile release of LHRH, pituitary gonadotropes release LH and FSH, also in a pulsatile manner. The secretion of gonadal steroids by the gonads is pulsatile and controlled by the amplitude and frequency of pituitary gonadotropin pulses. This complex system of the hypothalamic LHRH pulse generator and gonadotropin secretion operates actively during fetal life and infancy. Thereafter in childhood, this system is thought to be suppressed due to both gonadal steroid-independent and gonadal steroid-dependent inhibitory mechanisms.
Puberty is thought to be induced by the reactivation of this system. The initial endocrinologic events of puberty have been thought to cause the occurrence of pulsatile LH secretion at night. However, the recent development of immunoradiometric and immunofluorometric assays with high sensitivity has revealed LH pulsatility during sleep in prepubertal children(2, 3). It is now clear that, after the onset of puberty, the amplitude of LH pulses during sleep increases and the daytime level of LH pulses increases. First morning voided urinary gonadotropin and gonadal steroid excretion levels are thought to reflect the integrated serum values of the night before, in which pulsatile secretion of these hormones is most active through prepubertal and pubertal development.
Many studies have been done on diurnal pulsatile secretion of serum LH and FSH in children(4, 5). However, few studies have followed monthly serial changes of serum or urinary gonadotropins in children(6, 7). Using our new and simple method(8) for the determination of urinary gonadotropins, we have identified age- and pubertal stage-related changes in consecutive 30-d urine specimens from normal female and male prepubertal and pubertal children and patients with sexual disorders(9).
We have now extended our earlier studies to define the developmental characteristics of monthly urinary patterns of these hormones in normal female prepubertal and pubertal children based on a larger series. We have also studied urinary ovarian hormone levels in the same specimens to establish the pubertal changes in these hormones and to disclose the biologic consequences of these striking variations in urinary gonadotropin excretions.
METHODS
Subjects. Thirty-six normal healthy girls aged 2-16 y, one healthy adult aged 29 y, and 15 female patients with idiopathic precocious puberty were recruited for this study. The children were members of hospital staff families. The data of urinary gonadotropin levels of seven among these 36 normal girls and five among the 15 patients with precocious puberty in this study were reported previously(9). Pubertal development was assessed according to the criteria of Tanner(10). Of these children, three normal girls and three female patients with precocious puberty volunteered to collect urine specimens on 2-3 occasions at a 0.5-3.2-y interval. Of the normal girls who collected urine specimens, 15 were prepubertal (G1 and G2, 2-10-y-old, Tanner stage 1); eight were early pubertal (G3, 8-11 y, Tanner stage 2); eight were mid-pubertal (G4, 11-13 y, Tanner stage 3, all premenarcheal); and eight were late pubertal (G5, 12-16 y, Tanner stage 4, all postmenarcheal). The prepubertal girls were further divided according to age as age 6 y (G1) and age <6 y (G2).
Because some prepubertal girls aged <6 y (G2) were thought to be affected by the transient activation of the hypothalamo-pituitary-gonadal axis after birth, prepubertal girls aged 6 y were classified as G1 and compared with other groups.
According to clinical criteria, the diagnosis of precocious puberty in girls is established when breast buds appear before the age of 7 y, breast buds and pubic hair appear before the age of 8 y, and menarche occurs before the age of 9 y. Bone age was accelerated by a minimum of at least 1.5 y compared with the chronologic age. When female patients with precocious puberty were sampled, six were early pubertal (G6, 5-7 y, Tanner stage 2) and 14 were mid-pubertal (G7, 6-10 y, Tanner stage 3-4). FMV urine specimens were collected from these subjects for 30 consecutive days and were stored at 4°C for 1 mo(8, 16).
Hormone assays. Routine measurements of LH and FSH in urine after ammonium sulfate extraction were made by a polyclonal double-antibody RIA kit obtained from Eiken Co., Tokyo, Japan. Extraction and RIA procedures were the same as in our previous study(8). Urinary total estrogen (conjugated and unconjugated) and pregnanediol were measured by previously reported methods(11, 12). The results obtained from the method for RIA of urinary total estrogen(11) correlated well with the sum of urinary estrone, estradiol, and estriol values, urinary estrogen metabolites, measured by the reported method with the chromatographic purification method(13) (data not shown). The ratio of estrone to estradiol and estriol is 44.5 ± 16.6:13.4 ± 6.8:42.1 ± 17.2% in the urine of prepubertal girls measured by the assay(13)(n = 14). In the urine of pubertal girls, this ratio is 53.4± 14.7:15.3 ± 6.3:34.5 ± 12.4% (n = 11). The intraassay and interassay coefficient of variations for the total estrogen RIA system were 11.0 and 11.9%, respectively. The intraassay and interassay coefficient of variations for the pregnanediol RIA system was 7.3 and 12.8%, respectively. Creatinine concentration in urine was measured by the Jaffe reaction using an autoanalyzer. Results were divided by the creatinine concentration of the corresponding urine samples. All specimens from a single subject were assayed in the same RIA. The level of urinary pregnanediol was measured only in some normal girls, and some patients with precocious puberty.
Analysis of episodic excretions of urine hormones. The frequency of episodic excretions of urinary gonadotropin and ovarian hormones was analyzed using the method of Santen and Bardin(14). A significant spontaneous excretory increment of these hormones was defined as a rise from nadir to peak at least four times the corresponding intraassay coefficient of variation(15).
Statistics. The means in the five study groups of normal girls were compared using one way analysis of variance with post hoc testing (Bonferroni/Dunn). Statistical significance for the differences between the means of patients with precocious puberty and those of sexual stage-matched normal girls was determined by the unpaired t test. Values are given as mean ± SE. A p value of less than 0.05 was considered significant.
RESULTS
Correlation between FMV and 24-h Urinary Total Estrogen and Pregnanediol
A good correlation was obtained between determinations of FMV total urinary estrogen corrected for creatinine excretion and 24-h determinations of total urinary estrogen (data not shown). There was also a good correlation between determinations of FMV urine pregnanediol corrected for creatinine excretion and 24-h determinations of urinary pregnanediol (data not shown). The respective correlation coefficients are 0.94 (n = 24) and 0.84(n = 19).
Mean Level of Urinary LH, FSH, and Total Estrogen Excretions in Each Subject and in Each Group
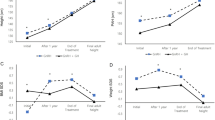
Normal girls. Mean levels of monthly urinary LH, FSH, and total estrogen excretions increased with pubertal stage in normal girls(Table 1 and Fig. 1). In the late prepubertal girls(G1), the mean urinary LH levels were very low (Fig. 1). Each mean LH level was lower than the mean FSH level in all prepubertal girls(Fig. 1). In each prepubertal girl, the highest LH levels did not exceed the lowest FSH values. The mean urinary LH level increased significantly from early to mid-pubertal stage (p < 0.005;Fig. 1 and Table 1). A similar pattern, but less pronounced; was seen for the mean FSH and total estrogen levels (p < 0.005; Fig. 1 andTable 1). With pubertal progression, each mean LH level increased and exceeded the FSH level.
Mean level of monthly urinary gonadotropin and total estrogen excretion in each normal girl and each patient with precocious puberty. The horizontal bars and columns represent mean ± SE obtained from normal girls and patients with precocious puberty. Statistical significance between each group of normal girls is shown with p value < 0.005(*).
There were few or small overlaps in each mean level of urinary LH and total estrogen excretions between early puberty and mid- to late puberty(Fig. 1). However, there were a lot of overlaps in each mean level of urinary FSH between these groups (Fig. 1). A remarkably high mean level of urinary FSH excretion was found in the two youngest (aged 2.5 and 2.8 y) of six early prepubertal girls (G2). The four other girls were aged 4-5 y.
Female patients with idiopathic precocious puberty. The mean level of monthly urinary LH excretion increased from early to mid-puberty in these female patients (Table 1 and Fig. 1). However, the mean FSH and total estrogen levels did not differ between these stages. The mean urinary LH in mid-puberty (p < 0.01), mean urinary FSH in early puberty (p < 0.001), and mean urinary total estrogen in mid-puberty (p < 0.01) differed in these female patients with respect to sexual stage-matched normal girls.
Mean Frequency of Episodic Excretions in Urinary Gonadotropin and Total Estrogen in Normal Girls and Female Patients with Precocious Puberty
The mean episodic excretions in monthly urinary LH and FSH were higher in early and mid-puberty in normal girls (G3 and 4) and female patients (G6 and 7) than those of prepuberty (G1); this was not true, however, of the values of FSH in mid-puberty (G4), as shown in Figure 2. More than 10 episodic fluctuations in urinary LH and FSH excretions per month were observed in early and mid-pubertal girls and patients, but not in other subjects (Fig. 2). After onset of menarche, the frequency of episodic fluctuations in urinary gonadotropins decreased in the normal girls studied.
Mean number of episodic fluctuations in monthly urinary gonadotropin and total estrogen excretion in each girl and patient with precocious puberty. The horizontal bars and columns represent mean ± SE obtained from normal girls and patients with precocious puberty. Statistical significance between each group of normal girls is shown with p value < 0.005(*).
Urinary Gonadotropin and Ovarian Hormone Excretory Patterns
Normal girls. Episodic excretory patterns of monthly urinary LH, FSH, and ovarian hormones were detected in all groups. Typical patterns of monthly urinary LH, FSH, and ovarian hormones in five normal girls at different sexual stages and in a female adult are shown in Figures 3–5. In an early prepubertal girl(2.8 y old, left panel in Fig. 3), roughly 4-fold excursions in FSH from one day to the next were found with low concentrations of urinary LH associated with little or no day-to-day variations. Responding to the increased excretion of FSH, total urinary estrogen excretion increased episodically and showed random fluctuations in the girl. Decreased levels and numbers of variations in urinary LH and FSH were found in a late prepubertal girl (7.0 y old, right panel in Fig. 3). Fewer fluctuations in total urinary estrogen were seen, although peak levels of these variations were higher. Urinary pregnanediol excretions were low in both girls and little day-to-day variations were seen.
In early pubertal girls, the urinary FSH levels increased and fluctuated markedly every other day, accompanied at the same time by similar rhythmic but less remarkable variations in urinary LH. Episodic fluctuations of total urinary estrogen excretion in early pubertal girls seemed to occur independently of the every-other-day variations in urinary gonadotropins(patterns not shown). This characteristic pattern in urinary LH and FSH was seen in three out of eight early pubertal normal girls (G3).
In a mid-pubertal girl (11.0 y old, left panel in Fig. 4), urinary LH levels approached the levels of urinary FSH and varied at the same time with every-other-day fluctuations. A similar monthly urinary pattern was observed in three out of eight mid-pubertal girls (G4). The levels of total urinary estrogen excretion varied, partly opposite to the fluctuations in urinary LH and FSH in this girl. From mid- to late puberty(premenarcheal stage), the levels of urinary LH excretions exceeded those of urinary FSH. Both hormones' periodic fluctuations vanished (patterns not shown). Higher urinary LH excretion varied irregularly with little variations in lower urinary FSH excretion, and menarche was observed in these monthly patterns. The monthly urinary patterns of these hormones collected 6 mo before menarche are shown in Figure 4 (12.3 y old, right panel in Fig. 4). A single large surge of urine LH was observed without subsequent rise in total urinary estrogen and pregnanediol like those in postmenarcheal girls. A postmenarcheal girl (14.6 y old, left panel inFig. 5) showed a pattern similar to that seen in a normal adult woman with regular menstruation (29 y old, right panel inFig. 5). The luteal phase in the girl and in the adult woman was 12 and 15 d long, respectively. The total estrogen and pregnanediol excretion levels were slightly lower in the girl than in the normal female adult.
Female Patients with Idiopathic Precocious Puberty
Monthly urinary patterns of hormones in three female patients with idiopathic precocious puberty at different pubertal stages are shown inFigures 6 and7. The urinary patterns collected three times at 0.6- and 1.2-y intervals from one patient are shown inFigure 6. At an early pubertal stage in this patient, the urinary pattern of these hormones changed from an irregularly and randomly fluctuating pattern of high FSH with low LH to a periodically and every-other-day fluctuating pattern of high FSH with less remarkable but similar variations in urinary LH. One and 0.2 y after the second urine collection with pubertal progression, the levels of urine LH increased and approached the levels of urinary FSH excretion with characteristic fluctuations in both hormones in this patient as shown inFigure 6 (right panel). During the time of collection, total urinary estrogen excretion varied independently from urine LH and FSH with diminished and infrequent fluctuations. A similar pattern was observed in another mid-pubertal patient, as shown in Figure 7 (7.7 y old, left panel). This characteristic pattern with periodic and every-other-day fluctuations in urinary gonadotropin excretions was found in two out of six early pubertal patterns of patients (G6) and eight out of 14 patterns of mid-pubertal patients (G7). In a late pubertal patient (7.1 y old, right panel in Fig. 7), the levels of urinary LH and FSH were almost equal and they fluctuated randomly. The periodicity of these gonadotropin excretions disappeared. In this patient, total urinary estrogen excretion seemed to rise before a high excretion of urinary LH and FSH.
DISCUSSION
We have already reported the monthly patterns of nighttime gonadotropin excretions using consecutive 30-d FMV urine specimens from normal children and from patients with sexual disorders(9).
In the present study based on a larger series, mean concentration, mean number of episodic fluctuations, and patterns of monthly urinary gonadotropin and ovarian hormone excretions at different pubertal stages were determined using 30-d FMV urine specimens from normal girls and female patients with idiopathic precocious puberty.
The mean level of monthly urinary gonadotropin and total estrogen excretion increased with pubertal maturation in normal girls and female patients with precocious puberty. Pubertal changes in mean levels of urinary gonadotropin excretions in normal girls were similar to pubertal changes in serum gonadotropin levels in normal girls reported previously(17). The mean levels of these urinary hormones in female patients differed, however, from those of sexual stage-matched normal girls. The reason is unclear; the discrepancy might be due to the limited number of subjects studied.
The present study confirmed our earlier observations(9) of monthly patterns of urinary LH and FSH during female pubertal development. In two aged less than 3 y, out of six early prepubertal girls, urinary FSH levels were very high with episodic and remarkable fluctuations, and urinary LH levels were low with few variations.
During infancy, the hypothalamo-pituitary-gonadal axis is transiently activated. Serum FSH concentrations are reported to be significantly higher in infancy than in the late prepubertal period(18). These urinary gonadotropin findings agree with serum findings.
With the onset of puberty, however, urinary LH levels rose with striking, rhythmic fluctuations in urinary FSH. With pubertal progression, urinary LH excretion increased further, approaching the urinary FSH level, and varied periodically, accompanied by the same rhythmic changes in urinary FSH.
In the present study, this characteristic monthly urinary pattern was observed in six out of 16 early to mid-pubertal normal girls' patterns and in 10 out of 20 female patients' urinary excretion patterns. Longitudinal follow-up of the monthly pattern was done in two normal girls and two female patients with precocious puberty. This striking pattern was observed in all four subjects from early to mid-puberty. Once the urinary LH level exceeded the urinary FSH level, these fluctuating urinary gonadotropin patterns disappeared. Menarche was observed at this stage. It is not fully understood how pituitary gonadotropin secretion changes from a pattern with no monthly cycle in girls to a cycled pattern associated with a solid surge of gonadotropins in adult women. Whereas the physiologic significance of these urinary patterns is not yet clear, our findings suggest that these characteristic patterns may appear between prepuberty with no periodic and no cyclic patterns in urinary LH and FSH and late puberty with a menstrual cycle, and that the onset of puberty is closely related to the occurrence of these patterns in urinary gonadotropins.
The number of episodic fluctuations in monthly urinary LH and FSH excretions increased from prepuberty to early and mid-puberty and decreased from mid-puberty to late puberty in normal girls. The fluctuations were most frequent and numbered 10 or more in early to mid-puberty. This was due to the occurrence of periodically fluctuating urinary LH and FSH pattern that is unique to early and mid-puberty.
Extensive comparison of our urinary gonadotropin findings with previously reported data is difficult, because publications are scarce in this area. Hansen et al.(6) reported that periodicity in urinary gonadotropin excretion in perimenarcheal girls is suggested by the occurrence of LH elevations associated with FSH elevations. They had investigated urinary gonadotropin excretion patterns only in perimenarcheal girls, not in early to mid-pubertal girls. They did not report the occurrence of these characteristic variations in monthly urinary LH and FSH excretions. The failure to observe these variations might be due to the limited number of subjects and the failure to subclassify pubertal stage. Kulin et al.(19) reported increased urinary LH and FSH excretion during sleep in prepubertal children and nocturnal augmentation of urinary LH excretion in pubertal children. They also reported that the circadian pattern of urinary gonadotropins might vary from one night to the next in pubertal children, because there were some children in whom the nighttime urinary LH excretion level was not higher than the daytime level. Their report suggests that daily fluctuations might occur in consecutive urinary gonadotropin excretions in pubertal girls.
To investigate the biologic basis for these pubertal variations in urinary gonadotropin excretions, we studied the level of urinary ovarian hormone excretions in the same urine specimens. The mean level of monthly total urinary estrogen excretion in normal girls and patients with precocious puberty increased with pubertal development. These findings were similar to those on serum estradiol levels in female subjects at different sexual stages reported previously(20). No variations corresponding to these characteristic monthly patterns with every-other-day fluctuations in urinary LH and FSH excretions were observed in total urinary estrogen excretions. The monthly urinary gonadotropin and ovarian hormone excretory patterns in these patients with precocious puberty were not different from those of sexual stage-matched normal girls.
Taylor et al.(21) reported that ovarian hormones alone were insufficient to induce the complex neuroendocrine interactions underlying the shift from negative to positive feedback. They hypothesized that other factors than ovarian hormones were required to generate the normal mid-cycle surge of gonadotropins. These reports suggest that factors other than ovarian hormones might play a role in the occurrence of these characteristic urinary gonadotropin excretory patterns. Once levels of urinary LH exceeded urinary FSH levels, increased total urinary estrogen excretion was observed before several high elevations of LH in mid-pubertal girls and female patients. These results seem to represent a change from negative to positive feedback by the hypothalamo-pituitary-ovarian axis before the onset of menarche. In normal premenarcheal and perimenarcheal girls, a solid high LH peak like a midcycle surge of LH was observed without subsequent rise in total urinary estrogen and pregnanediol excretions. Wennink et al.(22) reported the same results in normal girls upon measuring gonadotropin and estrogen in serum specimens sampled at 10-min intervals for 6 h twice a day.
Monthly patterns in urinary gonadotropin, total estrogen, and pregnanediol excretions during a menstrual cycle in a normal postmenarcheal girl and a regularly menstruating woman were similar to monthly patterns in serum gonadotropin, estradiol, and progesterone level in normal women with regular menarche.
The developmental changes in these monthly urinary hormone excretions seem to be in accordance with the changes from the transiently activated hypothalamo-pituitary-ovarian axis in infancy and the suppressed system in prepuberty to the reactivated system in puberty.
Further work is needed to evaluate the physiologic importance of these monthly patterns of urinary gonadotropin and ovarian hormone excretions in prepubertal and pubertal girls.
Abbreviations
- FMV:
-
first morning voided
- G:
-
group
- LHRH:
-
LH-releasing hormone
References
Grumbach MM, Styne DM 1992 Puberty: Ontogeny, Neuroendocrinology, Physiology and Disorder. In: Wilson JD, Foster DW (eds) Textbook of Endocrinology. Philadelphia: WB Saunders, pp 1139–1221
Wennink JMB, Delemarre-van de Waal HA, Van Kessel H, Mulder GH, Foster JP, Schoemaker J 1988 Luteinizing hormone secretion patterns in boys at the onset of puberty measured using a highly sensitive immunoradiometric assay. J Clin Endocrinol Metab 67: 924–928
Apter D, Cacciatore B, Alfthan H, Stenman U-H 1989 Serum luteinizing hormone concentrations increase 100-fold in females from 7 years of age to adulthood, as measured by time-resolved immunofluorometric assay. J Clin Endocrinol Metab 68: 53–57
Wu FCW, Butler GE, Kelnar CJH, Stirling HF, Huhtaniemi I 1991 Patterns of pulsatile luteinizing hormone and follicle-stimulating hormone secretion in prepubertal boys and girls and patients with idiopathic hypogonadotropic hypogonadism (Kallmann's syndrome): a study using an ultrasensitive time-resolved immunofluorometric assay. J Clin Endocrinol Metab 72: 1229–1237
Dunkel L, Alfthan H, Stenman U-H, Selstam G, Rosberg S Albertsson-Wikland K 1992 Developmental changes in 24-hour profiles of luteinizing hormone and follicle-stimulating hormone from prepuberty to midstages of puberty in boys. J Clin Endocrinol Metab 74: 890–897
Hansen JW, Hoffman AJ, Ross GT 1975 Monthly gonadotropin cycles in premenarcheal girls. Science 190: 161–163
Penny R, Olatunji Olambiwonnu N, Frasier SD 1977 Episodic fluctuations of serum gonadotropins in pre- and post-pubertal girls and boys. J Clin Endocrinol Metab 45: 307–311
Maesaka H, Suwa S, Tachibana K, Kikuchi N 1990 Quantitation of urinary gonadotropins in normal children. Pediatr Res 28: 401–404
Maesaka H, Suwa S, Tachibana K, Kikuchi N 1990 Monthly urinary LH and FSH secretory patterns in normal children and patients with sexual disorders. Pediatr Res 28: 405–410
Tanner JM 1962 Growth of Adolescence, 2nd Ed. Blackwell Scientific Publications, Oxford
Takami T, Tezuka T, Manita H, Kanbegawa A 1983 A simple method for radioimmunoassay of total estrogen in urine. Folia Endocrinol Jpn 59: 10–19
Manita H, Kanbegawa A 1978 Studies on the measurements of urinary pregnanediol by radioimmunoassay. Folia Endocrinol Jpn 54: 11–22
Makino T, Kanbegawa A, Kokubu T 1975 Radioimmunoassay for estrone, esradiol and estriol in urine and amniotic fluid. Follia Endocrinol Jpn 50: 788–796
Santen RJ, Bardin DW 1973 Episodic luteinizing hormone secretion in man. J Clin Invest 52: 2617–2628
Veldhuis JD, Rogol AD, Johnson ML 1985 Minimizing false-positive errors in hormonal pulse detection. Am J Physiol 248:E475–E481
Kesner JS, Knecht EA, Krieg EF 1975 Stability of urinary female reproductive hormones stored under various conditions. Repord Toxicol 9: 239–244
Oerter KE, Uriarte MM, Rose SR, Barnes KE, Cutler GB 1990 Gonadotropin secretory dynamics during puberty in normal girls and boys. J Clin Endocrinol Metab 71: 1251–1258
Faiman C, Winter JSD 1971 Sex differences in gonadotropin concentrations in infancy. Nature 232: 130–132
Kulin HE, Moore RG, Santner SJ 1976 Circadian rhythmus in gonadotropin excretion in prepubertal and pubertal children. J Clin Endocrinol Metab 42: 770–773
Carr BR 1992 Disorders of the ovary and femal reproductive tract. In: Wilson JD, Foster DW (eds) Textbook of Endocrinology. WB Saunders, Philadelphia, pp 733–798
Taylor AE, Whitney H, Hall JE, Martin K, Crowley WF 1995 Mid-cycle levels of sex steroids are sufficient to recreate the follicle-stimulating hormone but not the luteinizing hormone mid-cycle surge: Evidence for the contribution of other ovarian factors to the surge in normal women. J Clin Endocrinol Metab 80: 1541–1547
Wennink JMB, Waal HAD, Shoemaker R, Shoemaker H, Shoemaker J 1990 Luteinizing hormone and follicle-stimulating hormone secretion pattern in girls throughout puberty measured using highly sensitive immunoradiometric assays. Clin Endocrinol 33: 333–344
Acknowledgements
The authors thank A. Takahashi, Kanagawa Children's Medical Center, for the measurement of urinary creatinine and K. Kagiya for assistance. We thank Dr. A. Ogiwara, Yokohama City University School of Medicine, for the helpful advice on statistical analysis.
Author information
Authors and Affiliations
Additional information
Supported by a “Specific Disease” research grant from the Japanese Ministry of Health and Welfare and a comprehensive research grant for the prevention of mental and physical disorders from the Japanese Ministry of Health and Welfare.
Rights and permissions
About this article
Cite this article
Maesaka, H., Tachibana, K., Adachi, M. et al. Monthly Urinary Gonadotropin and Ovarian Hormone Excretory Patterns in Normal Girls and Female Patients with Idiopathic Precocious Puberty. Pediatr Res 40, 853–860 (1996). https://doi.org/10.1203/00006450-199612000-00013
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199612000-00013
This article is cited by
-
Urinary gonadotrophins: a useful non-invasive marker of activation of the hypothalamic pituitary-gonadal axis
International Journal of Pediatric Endocrinology (2012)