Abstract
To assess toxicokinetics of polychlorinated dibenzo-p-dioxins(PCDDs) and dibenzofurans (PCDFs), oral intake and fecal excretion were measured in two breast-fed infants and one formula-fed infant during the 1st y of life. The intake of these compounds was up to 50 times higher in the breast-fed infants. In these children, fecal excretion of the main tetra- to hexachlorinated congeners was less than 9% of the intake at age of 1 and 5 mo, indicating almost complete intestinal absorption during breast-feeding. In contrast, distinctly higher fecal excretion rates were observed for the hepta- and octachlorinated compounds. Despite much lower PCDD/PCDF intake after weaning, concentrations in stool fat did not decrease substantially. We conclude that concentrations in fecal fat more or less reflect those in body fat. Additionally, PCDD/PCDF concentrations were measured in blood fat of all infants (and in a second formula-fed baby) at the age of 11 mo. International toxicity equivalent (1-TEq) concentrations in the formula-fed infants were less than 25% of maternal values and about 10 times lower than in the infants breast-fed for 6-7 mo. In the latter, a distinct accumulation was found for the tetra- to hexachlorinated congeners compared with maternal concentrations. We conclude that accumulation of PCDDs and PCDFs in infants is as high as expected on the basis of intake data and assuming complete absorption and negligible elimination during the 1st y of life.
Similar content being viewed by others
Main
PCDDs and PCDFs are inadvertently formed in minute amounts, e.g. in combustion processes, and are ubiquitously distributed in the environment leading to background exposure of humans via food. For the last 10 y, it has been possible to analyze these compounds in the picogram/g range with sophisticated technical equipment. The concentrations measured in thousands of human milk samples showed a typical distribution pattern for the 2,3,7,8-substituted congeners, but were relatively high compared with other biologic samples due to accumulation of these compounds in the food chain, as already found for other lipophilic and biologically persistent compounds such as PCBs or organochlorine pesticides (e.g. hexachlorobenzene or DDT).
In particular, the additional accumulation in breast-fed infants due to the relatively high daily exposure to PCDDs and PCDFs via mother's milk, which is about 50 times higher (per kg of body weight) than in adults(1), has caused concern about possible adverse health effects. Theoretically, the contamination of mother's milk ought to lead to substantially higher levels in breast-fed infants than in their mothers (2.9 times after 6 mo assuming a daily consumption of 850 mL of milk with 3.5% fat and complete absorption)(2). Experimentally, comparable accumulation rates for 2378-T4CDD (i.e. 2,3,7,8-tetrachlorodibenzo-p-dioxin) have been found in monkeys at the end of the nursing period (3.7 times higher in marmosets, 4.3 times higher in rhesus monkeys)(3, 4). To confirm this in humans, tissue of sudden infant death syndrome infants was analyzed for PCDDs and PCDFs. At first sight, concentrations in most samples were unexpectedly low compared with the range measured in adults(5–7).
To test the hypothesis that absorption of PCDDs and PCDFs might not be complete in infants, we measured oral intake and fecal excretion of these compounds. Preliminary data of a 3-mo-old breast-fed infant suggested an almost complete absorption for the tetra- to hexachlorinated congeners, but not for the higher chlorinated ones(8). We then measured intake and fecal excretion of PCDDs and PCDFs in a balanced study involving two infants at age 1 and 5 mo during breast-feeding and again 2 mo after weaning. For comparison, a formula-fed (bottle-fed) infant was examined at the same age. To determine the extent of accumulation, it was additionally possible to measure PCDD/PCDF concentrations in blood fat of the infants at the age of 11 mo and to compare these values with those of their mothers.
METHODS
Subjects. Intake and fecal excretion of PCDDs and PCDFs were investigated in two breast-fed infants (B-1, B-2) and one formula-fed infant(F-1). Basic information about the mothers (all born and raised in Germany) and infants (all first-born) is compiled in Table 1, including weight gain and an investigation schedule of each child. All infants were healthy during the 1st y of life and had weight gains above the 50th percentile. Balanced investigations were performed for 5 d at the age of 1 mo, and for 6 d at the age of 5 mo and at the end of the 1st y. Blood was taken at the age of about 11 mo in the breast-fed infants (15 and 3 wk after weaning in infant B-1 and B-2, respectively), in formula-fed infant F-1, and a second formula-fed infant (F-2) for whom no intake/excretion investigations had been performed (because of analytical problems due to low concentrations, see below). Simultaneously, blood was also taken from the mothers who had then all reached their approximate prepregnancy body weight.
Intake measurements. During the investigation periods of 5-6 d, the volume of milk ingested by the babies was measured (breast-fed infants were weighed before and after being nursed). Mother's milk (mostly two samples in each period, at least 100 mL each) was obtained by emptying the entire milk content in the breast by pump. At the age of 5 mo, all babies also received commercially available pap. The amount of pap ingested was measured, and an aliquot of the same lot was analyzed for PCDDs and PCDFs. At the end of the 1st y, infants consumed a variety of foods (pap, cow's milk, homecooked food). The amount ingested was recorded, and a 10% aliquot of every meal was frozen at -18 °C. The pooled food samples from d 1 to 3 and from d 4 to 6 were then lyophilized and ground before analysis. (More detailed information about the diets is given in Table 3.)
Fecal excretion measurements. Duration of feces collection corresponded to that of the intake measurements, but displaced in time by 12-24 h, depending on the intestinal passage time, assumed to be 12 h at age 1 mo. At all other ages, the decision of which stools to include in the collection was made and controlled retrospectively by studying parents' records taken on food intake and diaper changes, and by inspecting the feces for visible markers such as carrots or blueberries. To validate this procedure and recognize eventual sample losses or contamination, samples were collected and analyzed separately for the first and second halves of the investigation periods. New cotton diapers were used preextracted as described elsewhere(9) to avoid contamination from diaper tissues containing relatively high amounts of PCDDs and PCDFs(8–10). I-TEq content per preextracted diaper was 0.42 pg (i.e. 2378-T4CDD < 0.07 pg, 23478-P5CDF = 0.13 pg, 12378-P5CDD < 0.10 pg, 123678-H6CDD = 0.30 pg, 1234678-H7CDD = 7.9 pg, OCDD= 60.5 pg).
Diapers with feces were stored at -18 °C and lyophilized later. Because all infants at the age of 1 mo had soft stools, a separation from the diaper material was impossible, and stool/diaper material had to be processed together. Parts of diapers without feces were cut out and weighed to determine the amount of tissue remaining in stool/diaper material used for analysis. Stool was formed at the age of 5 mo and thereafter, and it could be removed from diapers without significant loss. For the formula-fed infant (F-1) at the age of 1 mo, additionally laundered diapers were used which contained clearly increased levels of PCDDs and PCDFs after washing, and due to the low concentrations in stool fat it was impossible in this case to obtain reliable results from the diaper/stool analysis(9).
During the collection period, lasting several days, infants' bottoms were greased for skin protection with baby cream (up to 0.9 g/d). For this treatment (except in infants B-1 and F-1 at 1 mo) the same lot of Calendula Babycreme (Weleda AG Heilbetriebe, Germany) was used in which PCDD/PCDF concentrations were relatively low (in picograms/g of fat extracted, fat content 42%): 2378-T4CDD < 0.2, 23478-P5CDF < 0.2, 12378-P5CDD < 0.2, 123678-H6CDD = 0.83, 1234678-H7CDD = 11.7, OCDD = 103.0, I-TEq = 0.71 (0.49 if congeners under the limit of detection were disregarded, see below).
Analysis of mother's milk, baby food, feces, diapers, and baby cream. All of the samples were analyzed by the LUA (Oldenburg). The fat was separated from breast milk by centrifuge, blended with sodium sulfate, and eluted with hexane/acetone. Baby food was either refluxed for 4 h with CH2Cl2/methanol (milk formula and lyophilized mixed diet samples) or blended with sodium sulfate and eluted with cyclohexane/CH2Cl2 (ready-to-serve vegetable base meals). Baby cream was blended with sodium sulfate and eluted with n-hexane. Diaper, diaper/stool, and stool samples were extracted for 8 h withn- hexane/acetone. All extracts were evaporated, and the extracted lipids were determined gravimetrically. Cleanup was performed by multichromatographic columns. After concentrating the sample, quantification was performed using high resolution gas chromatography/mass spectrometry involving an Ultra 2 column coupled with a Finnigan MAT 95 mass spectrometer. For quantification and determination of the recovery rate, a mixture of13 C-labeled PCDDs and PCDFs was used.
Analysis of blood. It was possible to measure blood fat concentrations of PCDDs and PCDFs in the infants investigated for intake and fecal excretion by taking a blood sample of approximately 20 mL (40 mL in mothers). This found the agreement of our ethical committee and the consent of the parents. Whole blood was obtained by venipuncture before breakfast and collected in heparinized vials, frozen at -18 °C until analysis for PCDDs, PCDFs, and additionally for nonortho coplanar “dioxin-like” PCBs carried out by ERGO (Hamburg). Samples were spiked with 13C-labeled internal standards and then applied on a Chem Elute (modified silica gel) column. The blood lipids were eluted with hexane/isopropanol and determined gravimetrically. A multicolumn system was used for cleanup of the lipid extracts. The measurements were carried out by means of high resolution gas chromatography/mass spectrometry involving a SP 2330 and/or DB 5 silica column coupled with a VG AutoSpec mass spectrometer. The quantification was performed by the isotope dilution method and by comparison with an external standard mixture of all 2,3,7,8-substituted isomers in question(11–13).
Additionally, two fecal samples (aliquots consisting of three stool portions collected at the time of blood sampling) from infants B-2 and F-2 were analyzed by ERGO. Freeze-dried stool was mixed with sodium sulfate and spiked with 13C-labeled internal standards. The extraction was performed for 20 h using a hexane/acetone mixture on a Soxhlet apparatus. The lipid extracts were determined gravimetrically. Cleanup and measurements were performed as described for blood.
Evaluation. A complete list of the 15 2,3,7,8-substituted PCDD/PCDF congeners usually detected in human samples is shown inTable 4, together with the so-called I-TEFs proposed in 1988 by NATO/CCMS. These define the toxicity of each congener relative to the most toxic 2378-T4CDD (I-TEF = 1.0) and make it possible to calculate a single equivalent sum value (I-TEq) for a complex mixture of PCDDs and PCDFs. For these calculations, the concentrations of congeners below the limit of detection (defined as a signal-to-noise ratio in the relevant time window smaller than 3 to 1) were usually taken as one half of the limit value. If many congeners (especially the most toxic ones) were below the limit of detection, a second value calculated by disregarding any concentrations under the limit is given in Tables 3 and 4 as annotation.
Both LUA and ERGO participate in national and international quality control studies(13). Nevertheless, the possibility of interlaboratory differences should be kept in mind when blood values are compared with values of other origin.
RESULTS
Intake of PCDDs/PCDFs. For clarity, concentrations in dietary(and fecal) fat for each investigation period in the breast-fed (B-1, B-2) and the formula-fed (F-1) infants are compiled in Table 3 as average concentration on fat basis for the whole period of 5-6 d (calculation from at least two samples each) and for the main congeners only: 2378-T4CDD, 23478-P5CDF, 12378-P5CDD, and 123678-H6CDD, which contribute about 85% to the I-TEq value. Additionally, the less toxic 1234678-H7CDD and OCDD are listed which usually amount to more than 50% of the sum of all PCDDs/PCDFs in human samples. Concentrations in mother's milk fat of 19.7 and 22.2 pg of I-TEq/g(B-1 and B-2) resulted in a daily exposure of 82.2 and 106.2 pg of I-TEq/kg of body weight for the breast-fed infants (B-1 and B-2) at the age of 1 mo. This was considerably higher than the daily exposure of the formula-fed infant of 2.1 pg of I-TEq/kg of body weight from a diet containing 0.38 pg of I-TEq/g of fat. At the age of 5 mo, exposure per kg of body weight decreased in the breast-fed infants as they grew and were fed additional pap(Table 2). After weaning, PCDD/PCDF exposure was in a comparable range for all infants under investigation (1.3-3.6 pg of I-TEq/kg of body weight and d).
Fecal excretion of PCDDs/PCDFs. (Net) absorption rate of dietary fat was found to be above 94% (Table 2) in all infants. For the breast-fed infants, I-TEq concentrations in fecal fat at the age of 1 mo (18.2 and 16.0 pg/g in B-1 and B-2, Table 3) were comparable to those in milk fat (Table 3), clearly increased at 5 mo (45.0 and 32.5 pg/g in B-1 and B-2), and decreased only slightly after weaning (22.8 and 12.9 pg/g in B-1 and B-2) despite a considerably lower dietary intake of PCDDs/PCDFs. Therefore, concentration ratios fecal/dietary fat (Table 3) showed an increase from 1 to 5 mo and especially after weaning, when I-TEq concentrations in fecal fat were 24 and 40 times (B-1 and B-2) higher than in dietary fat. Despite unchanged fat absorption rates, fecal excretion rates as percentage of ingested PCDDs/PCDFs (Table 3) increased: for I-TEq from less than 7% during breast-feeding to more than 50% after weaning. These values reflect mainly the most toxic tetra- to hexachlorinated congeners. Distinctly higher fecal excretion rates were observed for the hepta- and octachlorinated compounds: in the breast-fed infants, between 25 and 85% of the OCDD “intake” was excreted at 1 and 5 mo, and even more than 100% after weaning.
In the 5-mo-old formula-fed infant F-1, PCDD/PCDF concentrations in fecal fat (Table 3) were under the limit of detection for all tetra- to hexachlorinated congeners with the exception of 2378-T4CDF which was found in relatively high concentrations in the pap(9). Hepta- and octachlorinated congeners were detectable, with relatively high fecal excretion rates (OCDD: 48% of the intake) comparable to those of the breast-fed infants at the same age. At the age of 10 mo most congeners were measurable in fecal fat despite unchanged concentrations in dietary fat. For I-TEq, the concentration ratio (fecal/dietary fat) was 6.7 and the fecal excretion rate 12.0% of the intake. Both values were lower than those in the breast-fed infants after weaning.
Concentrations in blood fat. The concentrations of PCDDs, PCDFs, and coplanar PCBs in blood fat of the infants (age 11 mo) and their mothers are listed in Table 4 (values of PCB 77 were not reliable due to a possible contribution of a contaminant). In the breast-fed infants, PCDDs and PCDFs had accumulated and reached distinctly higher concentrations (29.2 and 37.5 pg of I-TEq/g in B-1 and B-2) compared with their mothers (12.3 and 10.5 pg of I-TEq/g, respectively). In the formula-fed infants, only a few congeners were detectable in blood fat close to the limit of detection (e.g. 23478-P5CDF: 1.5 and 3.5 pg/g in F-1 and F-2) and distinctly lower than in their mothers (23478-P5CDF: 11.7 and 9.7 pg/g, respectively). PCDD/PCDF concentrations measured in stool aliquots of infants B-2 and F-2 (collected at the time of blood sampling, Table 4) were on the same order of magnitude as those in blood fat.
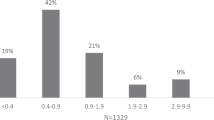
To illustrate the pattern of PCDD/PCDF/PCB accumulation,“accumulation factors” are shown in Figure 1 as a ratio of concentrations in infants' blood fat to those detected in maternal blood at the same time. In the breast-fed infants these factors were between 2 and 4 for tetra- to hexachlorinated congeners, but were distinctly lower for the higher chlorinated ones (lowest factor 0.79 for OCDD in infant B-1). In formula-fed infants the ratios were lower than 0.5 for all congeners detected.
DISCUSSION
Methods. Considering the high costs of PCDD/PCDF measurement, investigations were performed in only four infants who were healthy and developed normally during the 1st y of life. Amounts of fluids ingested and corresponding dietary fat intake (Table 2) were within the age-dependent range as were fat absorption rates(14), absolute fat excretion (e.g. 0.29-1.61 g/d in children 2-12 mo old)(15), and fecal dry mass excretion(16).
The use of baby cream may have contributed to the PCDDs/PCDFs measured in fecal fat, especially in cases of low fecal concentrations and in the higher chlorinated congeners, which were found in comparatively high concentrations in cream fat. Assuming a complete inclusion in feces, a maximum of 24% of OCDD in fecal fat (infant F-1 at 11 mo) could have originated from the baby cream. However, we estimate that not more than 20% of the PCDDs/PCDFs in cream will have reached the feces (distribution over a larger skin area, partial absorption by skin and diapers). Therefore, the baby cream would have contributed not more than 4.8% to the OCDD extracted from fecal fat, and was not taken further into account. In the breast-fed infants at 1 mo of age, when the soft feces could not be removed from the diapers, a source of inaccuracy could have come from the amount of preextracted diaper tissue that remained in the stool/diaper material. But in the case of OCDD found in relatively high concentrations in preextracted diapers, this contribution to the entire stool/diaper analysis accounted for only 16 and 14% (B-1 and B-2). The reliability of our balance method was checked by separate collection and analysis for the first and second halves of the investigation periods. Generally, these results were in good accord, and the average deviation between the two periods was 10% for ratios of I-TEq concentrations(fecal/dietary fat) and 13% for fecal excretion rates of I-TEq.
Intake of PCDDs/PCDFs. Concentrations in mother's milk were within the range measured in samples reported from Germany, 1992-1993(17–19). The congener pattern was typical for middle European countries, with the highest contribution to the I-TEq value by 23478-P5CDF (35-45%)(1, 18). The daily intake of infants B-1 and B-2 at the age of 1 mo (Table 2) was within the range of 48 to 346 pg of I-TEq/kg of body weight estimated for German babies weighing 5 kg(1). It was up to 50 times higher than in the formula-fed infant F-1 whose daily intake was close to the value of 2.5 pg of I-TEq/kg of body weight calculated from analyses of baby food for a 6-mo-old formula-fed child(20) and that of 2.3 pg of I-TEq/kg of body weight estimated for adults(1).
Fecal excretion of PCDDs/PCDFs. During breast-feeding, fecal excretion of the main congeners was low (<9% of the intake for 2378-T4CDD, 23478-P5CDF, 12378-P5CDD, and 123678-H6CDD) in contrast to the hepta- and octachlorinated congeners, confirming the findings of our previous study(8) and those of other investigators(21–24). Obviously, this phenomenon is due mainly to different rates of intestinal absorption, which is almost complete for the lower chlorinated compounds but distinctly poorer for the higher chlorinated ones, as has been observed in animal studies(25).
Although PCDD/PCDF intake for the breast-fed infants was much lower after weaning, fecal excretion did not decrease to the same extent. Obviously, other factors besides the rate of intestinal absorption also influence the overall fecal excretion of these compounds. In fact, with the exception of the poorly absorbed higher chlorinated congeners, concentrations in fecal fat after weaning (Table 3) and blood fat at 11 mo(Table 4) were in the same range. The phenomenon that fecal PCDD/PCDF concentrations more or less reflect those in the body can readily be observed during breast-feeding. In both infants, concentrations in fecal fat had increased between 1 and 5 mo of age together with the total PCDD/PCDF body burden, despite decreased concentrations in dietary fat. Consequently, the ratio of I-TEq concentrations (fecal/dietary fat) also increased from 0.9 to 2.9 and from 0.7 to 2.1 (in B-1 and B-2) and can be taken as a rough estimate for PCDD/PCDF accumulation occurring during breast-feeding. Also in the formula-fed infant F-1, concentrations of these compounds in fecal fat reflect those in body fat, and PCDD/PCDF fecal excretion rates calculated as percentage of the intake were found to be increased at 11 mo of age compared with 5 mo, but were distinctly lower compared with the breast-fed infants after weaning. Generally, these rates appear to depend much more on the proportion of PCDD/PCDF concentrations in dietary and body fat than on the rates of absorption of the ingested compounds. Absorption rates, calculated as 100% minus fecal excretion rate, can give only the net effect of intestinal absorption and elimination.
Our finding that PCDD/PCDF concentrations in fecal fat of infants mainly reflect those in body fat is in accordance with a similar observation reported in a 58-y-old man(26). Another investigation reports the amounts of PCDFs (and PCBs) excreted daily in feces to be comparable to those in 1 g of adipose tissue, both in normal subjects and in “Yusho” patients, who ingested rice oil contaminated with PCDFs, PCBs, and other compounds in Japan in 1968(27). PCDD/PCDF concentrations in fecal fat may be similar to those in body fat due to the partial endogenous origin of fecal fat as a result of turnover and shedding of epithelial cells(28) or the diffusion of ingested PCDDs and PCDFs between(body) fat in the intestinal wall and the intraluminal fat along the concentration gradient during intestinal passage (Fig. 2). There are probably many influencing factors, such as age, intestinal passage time, total intake of dietary fat and PCDDs/PCDFs, composition of the diet, absorption rate of intestinal fat and water, extent of enterohepatic circulation, consistency of feces, intestinal bacterial flora, or ongoing intestinal infections. For OCDD low reabsorption of endogenous losses into the intestine and slow diffusion exchange across the intestinal wall may explain why, in the breast-fed infants after weaning, fecal excretion exceeded 100% of the intake and why concentrations in fecal fat were higher than those in blood fat. For all congeners, fecal excretion can be expected to be higher than dietary intake as long as this is very low or zero. However, on the basis of absolute figures, fecal excretion of the unmetabolized PCDDs and PCDFs is not a relevant route of elimination: the total body burden scarcely decreased, because less than 1.5 g of fat/d were excreted, which for an infant at the age of 11 mo weighing 10 kg with 23% body fat(29) is only 0.065% of body fat mass.
Diagram of possible mechanisms affecting PCDD/PCDF concentrations in intraluminal fat during intestinal passage: secretion of endogenous fat which is partially reabsorbed, and diffusion of PCDDs and PCDFs between (body) fat in the intestinal wall and the intraluminal content. The situation after weaning is represented: low concentrations in the ingested fat and relatively high concentrations in body fat.
Similar assumptions were considered for the fecal excretion of other lipophilic compounds such as certain PCBs or hexachlorobenzene studied in experimental animals(30, 31). They also explain high and congener-specific fecal excretion rates of PCDDs and PCDFs in rats within the first 3 d after a single s.c. injection(32) or enhanced fecal excretion of hexachlorobenzene after intestinal application of poorly or nonabsorbable aliphatic hydrocarbons(30).
PCDD/PCDF concentrations in body fat. Concentrations of PCDDs and PCDFs measured in infants' blood fat were assumed to represent the body burden, as shown in adults(33–35). Compared with their mothers, the breast-fed infants had accumulated these xenobiotics at the end of the 1st y of life as expected from theoretical calculations(2), from animal experiments(3, 4), and from human data of pre- and postnatal exposure to PCBs(36) which are assumed to have a similar toxicokinetic behavior.
Comparing I-TEq concentrations in milk fat (age 1 mo) and infant's blood fat (age 11 mo), an accumulation by a factor 1.5 (B-1, nursed 6 mo) and 1.7(B-2, nursed 7 mo) was observed. These are not very different from the factors 1.8 (B-1) and 2.2 (B-2) which were estimated from fat consumption only, using1) the intake of milk fat during the first months of life (about 4.3 and 5.9 kg of milk fat in infant B-1 and B-2, respectively) and 2) the babies' body weight and assumed body fat content of 23% in boys at the age of 11 mo(29), but disregarding other factors, such as any elimination in the infant and a contribution from prenatal transfer or from baby food other than mother's milk. This estimation also disregarded the decrease of mothers' PCDD/PCDF body burden during the lactation period, reported to be 20-30% on average(1, 37). After nursing for 6-7 mo, the decrease was higher in both mothers of this study if their I-TEq concentrations in milk fat at 1 mo (19.7/22.2 pg/g in B-1/B-2) were compared with those in blood fat after weaning (12.3/10.5 pg/g in B-1/B-2). “Accumulation factors” (Fig. 1) calculated from PCDD/PCDF concentrations in blood fat of mother and infant at the end of the 1 y of life (2.4 and 3.6 for I-TEq) are influenced by increased infant's body burden as well as decreased maternal body burden. Therefore, the values are higher than those mentioned above rating concentrations in milk fat and infant's blood fat. The lower accumulation rates of the hepta- to octachlorinated congeners (Fig. 1) are explained by poor intestinal absorption and the lower concentrations in mother's milk than in mother's blood.
I-TEq concentrations in the formula-fed infants were an order of magnitude lower than those in breast-fed infants. Because the concentrations in blood fat of all mothers were in the same range, prenatal exposure of the infants had probably been comparable (and seems to play a minor role for the PCDD/PCDF body burden of a breast-fed infant at the end of the 1st y of life). Compared with their mothers, the levels in blood fat of the formula-fed infants were distinctly lower at 11 mo. Two factors determine the body burden at this age: prenatal exposure and contamination of the diet. In infant F-1 the contribution of postnatal nutrition can be estimated to be 1.2 pg of I-TEq/g of body fat (using the data of dietary fat intake, I-TEq concentrations in dietary fat, body weight, and body composition). Additionally, 1.8 pg of I-TEq/g of body fat will have remained from prenatal transfer, when an I-TEq transplacental transfer rate on a fat basis of 60%(38) was assumed and the known maternal concentration in blood fat and the data of body weight and body composition at birth and 11 mo(29) were used (corresponding to a 5.8-fold dilution of the PCDD/PCDF body burden at birth). On this basis, a total concentration of 3.0 pg of I-TEq/g of fat had to be expected, and the value of 2.4 pg of I-TEq/g of fat actually measured seems to be in agreement with our assumptions.
Our findings are in accordance with surprisingly low PCDD/PCDF concentrations reported for formula-fed sudden infant death syndrome infants(5–7, 39). In these infants (age 10-36 wk) a mean concentration of 3.5 pg of I-TEq/g of fat was measured in adipose tissue, whereas the value was about 10 pg of I-TEq/g of fat in stillborn infants. In contrast to our results, small postmorten differences were observed between most breast-fed and the formula-fed sudden infant death syndrome infants. However, only five (out of 15) were exclusively breast-fed for more than 2 mo, and of these the two with the longest history of full breast-feeding (13 and 19 wk) indeed had relatively high PCDD/PCDF values of 36.0 and 29.6 pg of I-TEq/g of fat, respectively, agreeing with the results of our study.
“Dioxin-like” coplanar PCBs 126 and 169, additionally analyzed in blood fat, were found to resemble the tetra- to hexachlorinated dioxins and furans in their toxicokinetic behavior (Fig. 1). The surprisingly low concentrations of these compounds in the stool aliquot of infant B-2 cannot yet be explained.
Conclusion. From the results presented, we conclude that accumulation of PCDDs and PCDFs in breast-fed infants is as high as would be expected on the basis of intake data and assuming complete absorption, a passive distribution following mainly that of fat in the body and a negligible elimination during the 1st y of life. Concern about possible adverse health effects requires a thorough risk assessment which has to include other lipophilic and biologically persistent compounds such as PCBs or organochlorine pesticides also accumulating in the food chain. Several studies have tried to evaluate unwanted clinical effects or minor alterations in sensitive biologic functions in children exposed pre- and postnatally to relatively high background PCDD/PCDF/PCB levels. Most of the reported findings, e.g. neurodevelopmental effects(40), changes in lymphocyte subpopulations(41), or endocrinologic parameters(42), are borderline, and we hesitate to interpret them as adverse health effects causally related to xenobiotic exposure. Consequently, we see no reason to call for restrictions or limitations on breast-feeding, the benefits of which have been demonstrated for children in industrialized and much more so in developing countries. Nevertheless, the aim remains to reduce the environmental contamination as much as possible. In this respect, the reports of decreasing PCDD/PCDF concentrations in human milk over recent years in European countries(17–19, 43) raise hope for improvement.
Abbreviations
- PCDD:
-
polychlorinated dibenzo-p-dioxin
- PCDF:
-
polychlorinated dibenzofuran
- T4CDD/T4CDF:
-
tetrachlorinated dibenzo-p-dioxin/furan
- P5CDD/P5CDF:
-
pentachlorinated dibenzo-p-dioxin/furan
- H6CDD/H6CDF:
-
hexachlorinated dibenzo-p-dioxin/furan
- H7CDD/H7CDF:
-
heptachlorinated dibenzo-p-dioxin/furan
- OCDD/OCDF:
-
octachlorinated dibenzo-p-dioxin/furan
- PCB:
-
polychlorinated biphenyl
- PCB 77:
-
3,3′,4,4′-tetrachlorobiphenyl
- PCB 126:
-
3,3′,4,4′,5-pentachlorobiphenyl
- PCB 169:
-
3,3′,4,4′,5,5′-hexachlorobiphenyl
- I-TEq:
-
international toxicity equivalent
References
Beck H, Dross A, Mathar W 1994 PCDD and PCDF exposure and levels in humans in Germany. Environ Health Perspect 102 ( suppl 1): 173–185.
Neubert D 1988 Significance of pharmacokinetic variables in reproductive and developmental toxicity. Xenobiotica 18 ( suppl 1): 45–58.
Hagenmaier H, Wiesmüller T, Golor G, Krowke R, Helge H, Neubert D 1990 Transfer of various polychlorinated dibenzo-p-dioxins and dibenzofurans (PCDDs and PCDFs) via placenta and through milk in a marmoset monkey. Arch Toxicol 64: 601–615.
Bowman RE, Schantz SL, Weerasinghe NCA, Gross ML, Barsotti DA 1989 Chronic dietary intake of 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) at 5 or 25 parts per trillion in the monkey: TCDD kinetics and dose-effect estimate of reproductive toxicity. Chemosphere 18: 243–252.
Beck H, Dross A, Kleemann WJ, Mathar W 1990 PCDD and PCDF concentrations in different organs from infants. Chemosphere 20: 903–910.
Beck H, Kleemann WJ, Mathar W, Palavinskas R 1994 PCDD and PCDF levels in different organs from infants. II. Organohalogen Compounds 21: 259–264.
Kreuzer PE, Päpke O, Baur C, Filser JG 1993 Pharmacokinetic modelling of the body burden of 2,3,7,8-tetrachlorodibenzo-p-dioxin in man over the entire lifetime validated by measured data. Fundam Clin Pharmacol 7: 368
Jödicke B, Ende M, Helge H, Neubert D 1992 Fecal excretion of PCDDs/PCDFs in a 3-month-old breast-fed infant. Chemosphere 25: 1061–1065.
Abraham K, Hille A, Ende M, Helge H 1994 Intake and fecal excretion of PCDDs, PCDFs, HCB and PCBs (138, 153, 180) in a breast-fed and a formula-fed infant. Chemosphere 29: 2279–2286.
Horstmann M, McLachlan MS 1994 Textiles as a source of polychlorinated dibenzo-p-dioxins and dibenzofurans (PCDD/F) in human skin and sewage sludge. Environ Sci Pollut Res 1: 15–20.
Päpke O, Ball M, Lis ZA, Scheunert K 1989 PCDD/PCDF in whole blood samples of unexposed persons. Chemosphere 19: 941–948.
Sagunski H, Päpke O, Herrmann T, Landgraff O, Schönfelder C, Wessel M, Koss G 1993 Selection of specific polychlorinated biphenyl congeners: analytical and toxicological aspects. Organohalogen Compounds 14: 129–135.
Stephens RD, Rappe C, Hayward DG, Nyren M, Startin J, Esboll A, Carlé J, Yrjänheikki EJ 1992 World Health Organisation international intercalibration study on dioxins and furans in human milk and blood. Anal Chem 64: 3109–3117.
Fomon SJ, Ziegler EE, Thomas LN, Jensen RL, Filer LJ 1970 Excretion of fat by normal full-term infants fed various milks and formulas. Am J Clin Nutr 23: 1299–1313.
Andersen DH 1945 Celiac syndrome. 1. Determination of fat in feces; reliability of two chemical methods and of microscopic estimate; excretion of feces and of fecal fat in normal children. Am J Dis Child 69: 141–151.
Sievers E, Oldigs HD, Schulz-Lell G, Schaub J 1993 Faecal excretion in infants. Eur J Pediatr 152: 452–454.
Alder L, Beck H, Mathar W, Palavinskas R 1994 PCDDs, PCDFs, PCBs, and other organochlorine compounds in human milk. Levels and their dynamics in Germany. Organohalogen Compounds 21: 39–44.
Fürst P, Fürst C, Wilmers K 1994 Human milk as a bioindicator for body burden of PCDDs, PCDFs, organochlorine pesticides, and PCBs. Environ Health Perspect 102 ( suppl 1): 187–193.
Päpke O, Ball M, Lis A, Wuthe J 1996 PCDD/PCDFs in humans, follow-up of background data for Germany, 1994. Chemosphere 32: 575–582.
Frommberger R 1993 Belastung des Säuglings mit Dioxinen und Furanen durch Säuglingsnahrung des Handels im Vergleich zur Belastung durch Humanmilch. Dtsch Lebensm Rundsch 89: 137–142.
Körner W, Dawidowsky N, Hagenmaier H 1993 Fecal excretion rates of PCDDs and PCDFs in two breast-fed infants. Chemosphere 27: 157–162.
McLachlan MS 1993 Digestive tract absorption of polychlorinated dibenzo-p-dioxin, dibenzofurans, and biphenyls in a nursing infant. Toxicol Appl Pharmacol 123: 68–72.
Pluim HJ, Wever J, Koppe JG, Van der Slikke JW, Olie K 1993 Intake and faecal excretion of chlorinated dioxins and dibenzofurans in breast-fed infants at different ages. Chemosphere 26: 1947–1952.
Dahl P, Lindström G, Wiberg K, Rappe C 1995 Absorption of polychlorinated biphenyls, dibenzo-p-dioxins and dibenzofurans by breast-fed infants. Chemosphere 30: 2297–2306.
Van den Berg M, De Jongh J, Poiger H, Olson JR 1994 The toxicokinetics and metabolism of polychlorinated dibenzo-p-dioxins(PCDDs) and dibenzofurans (PCDFs) and their relevance for toxicity. Crit Rev Toxicol 24: 1–74.
Rappe C, Andersson R 1992 Levels of PCDDs and PCDFs in human feces. Organohalogen Compounds 9: 195–198.
Iida T, Hirakawa H, Matsueda T, Nakagawa R, Takenaka S, Morita K, Narazaki Y, Fukamachi K, Takahashi K, Yoshimura H 1992 Levels of polychlorinated biphenyls and polychlorinated dibenzofurans in the blood, subcutaneous adipose tissue and stool of Yusho patients and normal subjects. Toxicol Environ Chem 35: 17–24.
Leading Article 1969 The origin of fecal fat. Lancet 2: 627–628.
Fomon SJ, Haschke F, Ziegler EE, Nelson SE 1982 Body composition of reference children from birth to age 10 years. Am J Clin Nutr 35: 1169–1175.
Rozman K 1985 Intestinal excretion of toxic substances. Arch Toxicol Suppl 8: 87–93.
Mühlebach S, Wyss PA, Bickel MH 1991 The use of 2,4,5,2′,4′,5′-hexachlorobiphenyl (6-CB) as an unmetabolizable lipophilic model compound. Pharmacol Toxicol 69: 410–415.
Abraham K, Wiesmüller T, Brunner H, Krowke R, Hagenmaier H, Neubert D 1989 Elimination of various polychlorinated dibenzo-p-dioxins and dibenzofurans (PCDDs and PCDFs) in rat faeces. Arch Toxicol 63: 75–78.
Patterson DG, Needham LL, Pirkle JL, Roberts DW, Bagby J, Garett WA, Andrews JS, Falk H, Bernert JT, Sampson EJ, Houk VN 1988 Correlation between serum and adipose tissue levels of 2,3,7,8-tetrachlorodibenzo-p-dioxin in 50 persons from Missouri. Arch Environ Contam Toxicol 17: 139–143.
Schecter A, Päpke O, Ball M, Ryan JJ 1991 Partitioning of dioxins and dibenzofurans: whole blood, blood plasma and adipose tissue. Chemosphere 23: 1913–1919.
Wuthe J, Link B, Walther J, Päpke O, Hagenmaier H, Frommberger R, Lillich W, Rack J 1993 Dioxin and furan (PCDD/PCDF) levels in human blood from persons living in a contaminated area. Chemosphere 27: 287–293.
Kodama H, Ota H 1980 Transfer of polychlorinated biphenyls to infants from their mothers. Arch Environ Health 35: 95–100.
Fürst P, Krüger C, Meemken HA, Groebel W 1989 PCDD and PCDF levels in human milk-dependence on the period of lactation. Chemosphere 18: 439–444.
Abraham K, Steuerwald U, Päpke O, Ball M, Lis A, Weihe P, Helge H 1995 Concentrations of PCDDs, PCDFs and PCBs in human perinatal samples from Faroe Islands and Berlin. Organohalogen Compounds 26: 213–218.
Beck H 1995 Occurrence in food, human issues and human milk. In: The Toxicology Forum: Chlorinated Organic Chemicals. Their Effect on Human Health and the Environment (Berlin, Germany, September 19-21, 1994). Toxicology Forum Inc., Washington DC, pp 216–247.
Brouwer A, Ahlborg UG, Van den Berg M, Birnbaum LS, Boersma ER, Bosveld B, Denison MS, Gray LE, Hagmar L, Holene E, Huisman M, Jacobson SW, Jacobson JL, Koopman-Esseboom C, Koppe JG, Kulig BM, Morse DC, Muckle G, Peterson RE, Sauer PJJ, Seegal RF, Smits-Van Prooije AE, Touwen BCL, Weisglas-Kuperus N, Winneke G 1995 Functional aspects of developmental toxicity of polyhalogenated aromatic hydrocarbons in experimental animals and human infants. Eur J Pharmacol 293: 1–40.
Dewailly É, Bruneau S, Laliberté C, Belles-Iles M, Weber JP, Ayotte P, Roy R 1993 Breast milk contamination by PCBs and PCDDs/PCDFs in arctic Quebéc: preliminary results on the immune status of Inuit infants. Organohalogen Compounds 13: 403–406.
Koopman-Esseboom C, Morse DC, Weisglas-Kuperus N, Lutkeschipholt IJ, Van der Paauw CG, Tuinstra LGMT, Brouwer A, Sauer PJJ 1994 Effects of dioxins and polychlorinated biphenyls on thyroid hormone status of pregnant woman and their infants. Pediatr Res 36: 468–473.
WHO 1995 Second round of exposure studies on levels of PCBs, PCDDs and PCDFs in human milk. Summary report on a WHO meeting (Berlin, March 23-24, 1994). World Health Organisation, Copenhagen
Acknowledgements
The authors thank especially Bruno, Daniel, Jasmin, and Lena and their parents for participation and for outstanding cooperation. We also express our gratitude to Ursula Steenken for accurate sample cleanup, to Gerda Post for skillful gas chromatography/mass spectrometry operation, and to Iris Suckrau for participation in analysis at the Lebensmitteluntersuchungsamt (Oldenburg). Additionally, we express our thanks for performing the sophisticated cleanup and measurements to Anton Lis, Bernd Schilling, Holger Jürgensen, and Peter Ebsen at the ERGO Forschungsgesellschaft (Hamburg). We also thank Hans Beck, Michael Becker, and Diether Neubert for helpful suggestions, and Markus Schülke for help in preparing the manuscript.
Author information
Authors and Affiliations
Additional information
Supported by the Research Budget of the Pediatric Department.
Rights and permissions
About this article
Cite this article
Abraham, K., Knoll, A., Ende, M. et al. Intake, Fecal Excretion, and Body Burden of Polychlorinated Dibenzo-p-dioxins and Dibenzofurans in Breast-Fed and Formula-Fed Infants. Pediatr Res 40, 671–679 (1996). https://doi.org/10.1203/00006450-199611000-00005
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199611000-00005
This article is cited by
-
Fremdstoffe und Krankheitserreger in der Muttermilch
Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz (2018)
-
Risks of dioxins resulting from high exposure via breast-feeding?
Archives of Toxicology (2017)
-
Assessment of questionnaire-based PCB exposure focused on food frequency in birth cohorts in Japan
Environmental Science and Pollution Research (2017)
-
Dioxin effects on neonatal and infant thyroid function: routes of perinatal exposure, mechanisms of action and evidence from epidemiology studies
International Archives of Occupational and Environmental Health (2006)
-
Breast milk and lipid intake distributions for assessing cumulative exposure and risk
Journal of Exposure Science & Environmental Epidemiology (2005)