Abstract
We have investigated the relationship among the HIV-1 biologic phenotype, replicative capacity of virus isolates, HIV-RNA copy number in plasma, p24 antigenemia, CD4+ T lymphocyte counts in peripheral blood, and the clinical status in a cohort of 13 HIV-infected children younger than 12 mo of age, born of HIV-1 seropositive mothers. Six out of 13 HIV-1 isolates from these patients were classified as rapid/high and seven as slow/low. We have found a significantly positive correlation between the replication rate of HIV isolates and their capacity to induce syncytia in vitro. Most of the serial HIV-1 isolates obtained from infants with AIDS had the rapid/high phenotype and induced syncytia, whereas only two out of 23 HIV-1 isolates obtained from infants without AIDS showed these properties. In sequential analysis of HIV-1 isolates from infants with AIDS, the presence of viral isolates with rapid/high and SI phenotype was associated with higher levels of HIV-1 RNA in plasma, CD4+ T cell depletion, and clinical progression. By contrast, infants whose viruses exhibited nonsyncytium-inducing phenotype throughout the follow-up showed lower levels of HIV RNA, stable CD4+ T cell counts, and mild symptomatic HIV infection. Our findings indicate that infants who carried viruses with more cytopathic biologic phenotype and who had higher viral RNA coy numbers in blood were more likely to have lower CD4+ T cell counts and more likely to have AIDS.
Similar content being viewed by others
Main
In adults infected with HIV-1, an association between the in vitro phenotypic properties and replicative capacity of virus isolates and progression of disease has been described(1–4). Also, changes in phenotype, from NSI to SI HIV-1 strains are associated with a rapid decline in CD4+ lymphocyte counts and the progression to symptomatic disease(5). Furthermore, the biologic phenotype of HIV-1 isolates, as determined by the ability to replicate in MT-2 cells, is an independent marker for a poor prognosis(6).
Perinatally acquired HIV-1 infection follows a different clinical course than HIV-1 infection in adults, and the age at infection of HIV-1-infected children appears to be an important risk factor for disease progression(7–9). However, the described immunologic defects of HIV-1-infected children do not differ qualitatively from those described in adults(8, 10). Very little information exists concerning the relationship among in vitro phenotypic properties and the replicative capacity of HIV-1 isolates, the viral load, and the clinical manifestations of HIV-1 infection in pediatric patients(11–15). We have performed a prospective 28-mo follow-up of the evolution of HIV infection in a cohort of 13 HIV-infected children who were all less than 1 y of age. We have investigated the relationship among the HIV-1 biologic phenotype, replicative capacity of virus isolates, HIV-RNA copy number in plasma, p24 antigenemia, CD4+ T lymphocyte counts in peripheral blood, and the clinical status in this cohort of HIV-infected children.
METHODS
Patients. The patients included in the study were 64 infants admitted to our Division of Pediatrics at the University General Hospital of the Community of Madrid (ages ranging from 2 to 12 mo) who were born to HIV-1-infected mothers and had no history of hemophilia or blood transfusion. We performed a prospective follow-up lasting from 1 to 28 mo of the evolution of HIV infection in a cohort of 13 HIV-infected infants. The infants were classified according to the new Center for Disease Control and Prevention classification system for HIV infection in infants and children under 13 y of age(16).
Serologic analysis. Serum samples were tested for HIV-1-specific antibodies by Western blot (Pasteur-Sanofi)(17).
Extraction of RNA from plasma. RNA was extracted from plasma by a previously described method(18–19). Briefly, 200 μL of clarified plasma to which 200 μL of 5 M guanidinium thiocyanate had previously been added were extracted with phenol/chloroform and precipitated with isopropanol. The resulting pellet was then washed in 75% ethanol, dried, and dissolved in diethylpyrocarbonate-treated glass distilled water.
Reverse transcription and amplification of cDNA. HIV RNA was transcribed to cDNA using avian myeloblastosis virus reverse transcriptase(Boehringer Mannheim, Indianapolis, IN) by a previously described method(19, 20). Oligomers used for amplification included SK38, SK39, and SK19, all of whose sequences have been published previously(21). Biotinylation of SK38 and horseradish peroxidase labeling of probe SK19 were carried out as described previously(22). Amplification of HIV cDNA was carried out in 100μL of a reaction mixture containing 50 pmol of primers SK38 and SK39, 10 mM dNTP, 10 mM Tris (pH 8.3), 2.5 mM MgCl2, 50 mM KCl, and 2.5 U of recombinant Taq DNA polymerase (Perkin-Elmer, Norwalk, CT). The mixture was then overlaid with 50 μL of mineral oil. Tubes were placed in a DNA thermal cycler (Perkin-Elmer) for 30 cycles of amplification with the following program: 95 °C, 30 s; 55 °C, 30 s; and 72 °C, 60 s for denaturation, annealing, and extension, respectively. Negative and positive controls which included a standard curve were prepared by adding different amounts of a stock of HIV S61 virus (0, 1, 10, 50, 100, 500, 1000, 5000, and 10000 viral particles) to HIV seronegative control plasma.
Detection and quantitation of PCR products. To detect and quantitate the PCR products, 96-well microplates were coated with 100 μL of a 0.1 mg/mL solution of avidin (Sigma Chemical Co., St. Louis, MO) in 50 mM Na2CO3 (pH 9.6) overnight at room temperature. Wells were washed twice with PBS and then filled with 300 μL of a blocking solution containing 5 × Denhardt's solution, 1% gelatin (Sigma Chemical Co.), 250μg/mL sheared herring sperma DNA (Promega Biotech Inc., Madison, WI) and incubated at least overnight at 4 °C. Immediately before use, the blocking solution was aspirated from each well, and 5 μL of PCR product, 65 μL of a hybridization solution, containing 5 × saline sodium phosphate EDTA, 5× Denhardt's solution, and 1 pmol horseradish peroxidase-labeled SK19 HIV gag specific probe were added to each well. A capture and hybridization reaction was then carried out for 1 h at 42 °C. The 96-well microplates were washed five times with PBS containing 0.05% Tween-20. The horseradish peroxidase substrate O-phenylenediamine (Sigma Chemical Co.) was prepared at 0.6 mg/mL in 0.1 M citrate buffer (pH 5.5) containing 0.03% hydrogen peroxide. One hundred and fifty microliters of this substrate solution were added to each well. After 10 min, the reaction was stopped with 1 N H2SO4, and OD of each well was measured at 490 nm.
Detection of proviral DNA by PCR in PBMC. PBMC from all infants were analyzed for the presence of HIV-1 DNA by PCR with three different sets of nested primers specific for regions of the gag, pol, andenv genes (JA4 to JA7, JA17 to JA20, and JA13 to JA16, respectively) as previously described(23, 24). Briefly, the samples were first amplified for 24 cycles with the outer primers, then 0.1 (5μL) of the product from the first PCR reaction was amplified for 30 cycles with the inner primers. Preparation of samples was done in a biosafety laminar airflow hood, exclusively used for this purpose(25). Samples from all individuals gave positive signals with primers PCO3-PCO4 specific for the human β-globin gene(26) and were therefore suitable for amplification. Negative controls were included in each run and consisted of lysis buffer alone and samples from healthy blood donors. Positive controls consisted of samples from PBMC cultures infected with HIV-1 virus. The PCR product was analyzed by electrophoresis on 1.5% agarose gel stained by ethidium bromide. Samples were considered positive if at least two different primer sets repeatedly gave a specific amplification product.
Virus isolation. The HIV-1 virus was isolated by a microculture technique which is useful for pediatric patients, because it requires substantially fewer PBMC(27). PBMC were isolated from blood by Ficoll-Hypaque density gradient centrifugation (Pharmacia)(27, 28). Both viral culture and PCR assay were performed on the same sample; PBMC (2 × 106) from patients were cultured with an equal number of PBMC from healthy donors. Donor PBMS had been pretreated for 48 h with PHA (Difco Laboratories, Detroit, MI) in RPMI 1640(Life Technologies, Inc., Paisley, Scotland, UK) supplemented with 20% heat-inactivated fetal bovine serum, 5% IL-2 (Boehringer Mannheim), 100 IU/mL penicillin, and 100 μg/mL streptomycin (Life Technologies, Inc.). Fresh PBMC (2 × 106) were added to the culture once a week. Supernatants were collected twice a week and tested for the presence of p24 HIV-1 antigen with the use of a commercially available kit (Elavia-Ag I, Diagnostics Pasteur)(19). The criteria for a positive coculture and determination of the days to the first positive result were based on HIV p24 results obtained from biweekly culture samples(11). According to the lag phase before p24 antigen detection and to the level of p24 antigen production by PBMC, HIV-1 isolates from these patients were classified as rapid/high or slow/low. The HIV isolates were operatively defined as rapid replication output (rapid/high), because p24 antigen was detected in PBMC supernatants as early as 3 d after being cultured, and moreover they produced persistently high p24 levels. In contrast, HIV isolates that had a lag phase of ≥7 d and thereafter produced consistently much lower p24 levels were designated as slow/low.
Determination of the viral phenotype. PHA-stimulated PBMC were infected with cell-free supernatant collected from each virus isolate, and after 7-10 d, the infected PBMC were cocultured with the MT-2 cell line. Cultures were maintained in the same medium as described for the PBMC cultures but without IL-2. Half of the cultures were replaced with fresh culture medium two times a week. MT-2 cell and infected PBMC cultures were checked for syncytium formation under light microscopy(29).
HIV-p24 antigen assay. To improve detection of the levels of HIV-p24 antigen in serum, the circulating immune complexes were dissociated(ICD p24) by a method based on low pH treatment of the patient's sample before using an ELISA (ELAVIA-Ag I, diagnostics Pasteur)(19–24). Briefly, four volumes of serum were mixed with one volume of 0.5 N HCI. After incubation of the mixture for 90 min at room temperature, the treated patient's serum was neutralized with one volume of 0.5 NaOH, mixed, and immediately added in two wells of the reaction microplate. After this treatment on the patient's serum the ELISA procedure was performed according to the manufacturer's instructions.
Quantification of T cell subsets in peripheral blood. T lymphocyte subsets in peripheral blood were quantified by direct immunofluorescence using MAb of the T series and flow cytometry (FACScan, Becton Dickinson, Franklin Lakes, NJ) as previously described(17).
Statistics. The statistical differences in the values of HIV RNA viremia and in the percentages of CD4+ T lymphocytes between both groups of infants (group 1, six infants infected with rapid/high and SI HIV-1 isolates; group 2, seven infants infected with slow/low and NSI HIV-1 isolates) were analyzed by a nonparametric test (Mann-Whitney). To reassure the statistical significance of the differences in the percentages of CD4+ T cells between both groups of infants, an analysis of variance was used in which the age of infants was included as a covariate. Binomial distribution values were used to assure the significance of proportions of cases with AIDS in both groups of infants. Binomial distribution values were also used to assure the significance of proportions of cases with detectable p24 antigen in serum in both groups of infants. Association between variables was measured by means of the nonparametric Spearman's rank-correlation coefficients.
RESULTS
On the basis of nested PCR and viral culture findings, 13 (20%) of the 64 infants born from HIV-1 seropositive mothers were identified as infected with HIV-1. HIV-1 isolates with SI ability were isolated in 6 out of 13 (46%) infants, whereas NSI HIV-1 isolates were isolated in 7 out of 13 (54%)(Table 1). HIV-1 isolates were determined to have SI capacity by cocultivating the patient's PBMC either with healthy donor PBMC or MT-2 cell types.
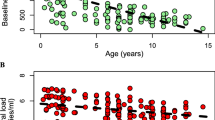
After coculturing the cells from the HIV+ infants with normal PHA-stimulated PBMC, two patterns of viral replication emerged. Six HIV isolates were operatively defined as rapid replication/high output(rapid/high) (Fig. 1A). By contrast, seven isolates were designated as slow/low (Fig. 1B). We have found a positive correlation between the replication rate of HIV isolates and their capacity to induce syncytia in vitro (Table 1).
HIV-1 replication on primary PBMC cocultures. PBMCs from HIV+ infants were cocultured with PHA-stimulated-PBMCs from healthy donors, and culture supernatants were tested for p24 HIV antigen. According to lag phase and slopes of the p24 production curves, HIV-1 isolates were classified as rapid/high (panel A) and slow/low (panel B).
Distinct differences were seen in the capacity of sequential isolates from nine infants to induce syncytium formation. Sequential isolates from patient nos. 8 to 11 who initially had NSI isolates remained unable to induce syncytium formation in MT-2 cell cultures irrespective of the time of isolation (Table 1). However, early HIV-1 isolates derived from patient nos. 6 and 13 who initially had NSI isolates were unable to induce syncytium formation, whereas later isolates induced syncytium formation in MT-2 cells (Table 1). Serial HIV-1 isolates derived from patient nos. 1, 2, and 4 who initially had SI isolates were uniformly able to induce syncytium formation irrespective of the time of isolation during follow up (Table 1). A direct association between syncytium formation in the MT-2 cell cultures with serial isolates from patient nos. 1, 2, 4, 6, and 13 and disease progression was observed.
HIV-1 ICD p24 antigen was detectable in the serum of 5 out of 13 (38%) HIV infected infants. In these infants four out of 5 (80%) had rapid/high and SI HIV-1 isolates. On the other hand, two out of 8 (28%) infants with negative p24 antigenemia had rapid/high and SI HIV-1 isolates (Table 1). These results indicate that there is a trend for the presence of detectable p24 antigen in serum to be associated with the SI capacity and the high replication rate of HIV-1 isolates, although this was not found to be statistically significant.
HIV-1 RNA in plasma was detectable in the 13 HIV-infected infants. At the initiation of the study, patients infected with rapid/high and SI HIV-1 isolates showed a significantly higher viral load than those with slow/low and NSI HIV-1 isolates (p < 0.001) (Table 2). We also analyzed the relationship among the percentage of CD4+ T lymphocytes, the viral phenotype, the viral replicative ability, and the viral load. Infants infected with rapid/high and SI HIV-1 isolates and with high levels of HIV RNA in plasma had a significantly lower percentage of CD4+ T cells and more severe disease than those with slow/low and NSI viral isolates and lower levels of HIV RNA (Table 2). The association of SI phenotype with lower CD4+ lymphocyte percentages was also statistically significant by using an analysis of variance in which the age of infants was included as a covariate (analysis of variance, p< 0.05). On the other hand, there was a strong negative correlation between the percentage of CD4+ T cells and the HIV RNA copy number/mL in plasma(r = -0.826).
The results of quantitative RNA PCR studies on sequential plasma samples from infants nos. 1, 2, and 6 showed an association between high levels of HIV RNA, SI phenotype, CD4+ T cell depletion, and clinical progression(Table 1). In infant no. 6, an increase in the levels of HIV-1 RNA was seen concurrent with the switch from NSI-slow/low to SI-rapid/high phenotype and with the CD4+ T cell decline. In contrast, infants whose viruses exhibited an NSI phenotype throughout the follow-up showed lower levels of HIV RNA, stable CD4+ T cell counts, and mild symptomatic HIV infection (Table 1).
In summary, the infants with more severe clinical symptoms carried the viruses with more cytopathic biologic characteristics, had higher viral load in blood, and had lower CD4+ T cell counts.
DISCUSSION
Recently, it has become increasingly important to know which are the virologic and immunologic factors that relate to the rapid or slow progression of HIV infection in pediatric patients(8, 30–36). However, correlation of viral burden, phenotype and replication rate, p24 antigen, CD4+ count, and clinical status has not been comprehensively analyzed in an HIV-infected pediatric population in the past. In HIV-infected children younger than 12 mo of age we have found a complete positive correlation between the replication rate of HIV isolates and their capacity to induce syncytia in vitro. Our studies in sequential HIV-1 isolates derived from HIV-infected infants showed that HIV-1 isolates with SI phenotype had increased levels of viral replication in PHA-stimulated PBMC cultures (rapid/high) compared with HIV-1 isolates with NSI phenotype that were slow/low. The ability of HIV-1 isolates to induce syncytia and their pattern of replication in vitro also correlated with the stage of the disease. Most of serial HIV-1 isolates obtained from infants with AIDS had the rapid/high phenotype and induced syncytia, whereas only two out of 23 HIV-1 isolates obtained from infants without AIDS showed these properties. This datum is in agreement with other recent studies in HIV-infected infants(11, 29) and in HIV-infected adults(4–6, 37, 38). However, two other studies in HIV-infected children(12, 13) have concluded that HIV-1 isolates from children with or without AIDS have similar in vitro biologic properties (viral phenotype and replication rate). This is a controversial subject that due to the limited sizes of the studies of the above-mentioned reports, requires further investigation in large scale prospective studies.
Virus load and virus phenotype have both been indicated as potential markers of disease progression in HIV infection(11, 14, 39, 40). In our study there was observed a significant association between the viral growth patternin vitro, the HIV-1 copy number in vivo, and the severity of HIV-1 infection. In sequential analysis of HIV-1 isolates from infants with AIDS, the presence of viral isolates with rapid/high and SI phenotype was associated with higher levels of HIV-1 RNA in plasma. In agreement with these results other authors have observed a direct association between clinical progression, increase in viral burden, and emergence of a more cytopathic viral phenotype(14, 39). Another study has shown that both rapid progression to AIDS and asymptomatic clinical courses were observed in infants with persistently high levels of virus(41). In three of our cases of infants with AIDS and with HIV-1 isolates with SI phenotype the substantial increase in the levels of HIV-1 RNA was observed associated with a profound CD4+ T cell decline. This datum is in agreement with another report in a HIV-infected adult population(39). It has been suggested that an increase in viral load linked with increased virulence of the HIV isolate may have a synergistic effect resulting in a rapid decline of CD4+T lymphocytes(39). Cumulatively, the findings in this study indicate that children who carried viruses with more cytopathic biologic phenotype and who had higher viral RNA copy numbers in their blood were more likely to have lower CD4+ cell counts and were more likely to have AIDS.
Using PCR for detection of HIV RNA in plasma we have found that all of the HIV-infected infants had an active replicative infection. However, p24 antigenemia was not always detected in the AIDS and non-AIDS children. Serum p24 antigen was positive in four out of six infants with rapid/high-type HIV-1 isolates and with high HIV-1 copy number, whereas the seven infants with slow/low-type HIV-1 isolates and a significantly lower HIV-1 copy number had undetectable or low levels of serum p24 antigen. There was not a good correlation between the p24 antigenemia and the number of HIV-1 copiesin vivo. Our results indicate that HIV detection by PCR in plasma is more sensitive than p24 antigenemia for the assessment of viral replicationin vivo in HIV-infected infants(40, 41).
The factors that influence the evolution of HIV infection in children are currently unknown but are likely to include both viral factors and host immunologic factors(42). The link between viral load, virus phenotype, and clinical course does not necessarily imply a cause an effect relationship. It is conceivable that, in certain children vertically infected with HIV, during the first year of life, the existence of an immature or deficient immune system could account for the intensive viral replication and dissemination(43).
This study has been limited to the evaluation of children ≤12 mo of age and suggests that in some patients the viral phenotype is fixed very early in life. Our investigation addresses multiple prognostic features of HIV-1 infection which may be helpful in characterizing prognostic groups in HIV-1-infected children.
Abbreviations
- HIV-1:
-
human immunodeficiency virus type 1
- SI:
-
syncytium-inducing
- NSI:
-
nonsyncytium-inducing
- PBMC:
-
peripheral blood mononuclear cell
- PCR:
-
polymerase chain reaction
- PHA:
-
phytohemagglutinin
References
Tersmette M, De Goede REY, Al BJ, Winkel I, Gruters B, Cuyper SHT, Huisman HG 1988 Differential syncytium-inducing capacity of human immunodeficiency virus isolates: frequent detection of syncytium-inducing isolates in patients with acquired immunodeficiency syndrome (AIDS) and AIDS-related complex. J Virol 62: 2026–2032
Cheng-Mayer C, Seto D, Tateno M, Levy JA 1988 Biologic features of HIV-1 that correlate with virulence in the host. Science 240: 80–82
Tersmette M, Lange JMA, De Goede REY, De Wolf F, Eftink-Schattenker JKM, Coutinho RA, Huisman JG, Goudsmit J, Miedema F 1989 Association between biological properties of human immunodeficiency virus variants and risk for AIDS and AIDS mortality. Lancet 1: 983–985
Asjo B, Morefeldt-Manson L, Albert J, Biberfeld G, Karlsson A, Lidman K, Fenyo EM 1986 Replicative capacity of human immunodeficiency virus from patients with varying severity of HIV infection. Lancet 2: 660–662
Tersmette M, Gruters RA, De Wolf F, De Goede REY, Lange JMA, Schellekens TNA, Gudsmit J, Huisman HG, Meidema F 1989 Evidence for a role of virulent human immunodeficiency virus (HIV) variants in the pathogenesis of acquired immunodeficiency syndrome: studies on sequential HIV isolates. J Virol 63: 2118–2125
Koot M, Vos AHV, Keet RPM, De Goede REY, Dercksen W, Terpstra FG, Coutinho RA, Miedema F 1992 HIV-1 biological phenotype in long-term infected individuals evaluated with an MT-2 cocultivation assay. AIDS 6: 49–54
Pizzo PA 1990 pediatric AIDS problems within problems. J Infect Dis 161: 316–325
Scott GB, Hutto C, Makuch RW 1989 Survival in children with perinatally acquired human immunodeficiency virus type 1 infection. N Engl J Med 321: 1791–1796
Goedert JJ, Kessler CM, Aledort L, Biggar RI, Andes WA, White GC, Drummoud JE, Vaidya K, Mann DL, Euster ME, Ragni MV, Lederman MM, Cohen AR, Bray GL, Rosenberg PS, Friedman RM, Higartner MW, Blattner WA, Kroner B, Gail MH 1989 A prospective study of human immunodeficiency virus type 1 infection and the development of AIDS in subjects with hemophilia. N Engl J Med 321: 1141–1148
Munoz A, Want MC, Bass S, Taylor MG, Kingsley LA, Johmiel JS, Folk BF, the Multicenter AIDS Cohort Study 1989 Acquired immunodeficiency syndrome (AIDS)-free time after human immunodeficiency virus type 1 (HIV-1) seroconversion in homosexual men. Am J Epidemiol 130: 530–539
De Rossi A, Giaquinto C, Ometto L, Mammano F, Zanotto C, Dunn D, Chieco-Bianchi L 1993 Replication and tropism of human immunodeficiency virus type 1 as predictors of disease outcome in infants with vertically acquired infection. J Pediatr 123: 929–936
Gupta P, Urbach A, Cosentino L, Thampatty P, Brady M 1993 HIV-1 isolates from children with or without AIDS have similar in vitro biologic properties. AIDS 7: 1561–1564
Spencer LT, Ogino MT, Dankner WM, Spector SA 1994 Clinical significance of human immunodeficiency virus type 1 phenotypes in infected children. J Infect Dis 169: 491–495
De Rossi A, Pasti M, Mammano F, Ometto L, Gianquinto C, Chieco-Bianchi L 1991 Perinatal infection by human immunodeficiency virus type 1 (HIV-1): relationship between proviral copy number in vivo, viral properties in vitro, and clinical outcome. J Med Virol 35: 283–289
Leibovitz E, Rigaud M, Pollack H, Lawrence R, Chandwani S, Krasinski K, Borkowsky W 1990 Pneumocystis carinii pneumonia in infants infected with the HIV with more than 450 CD4T lymphocytes per cubic millimeter. N Engl J Med 323: 531–533
Center for Diseases Control and Prevention 1994 Revised classification system for HIV-1 infection in children less than 13 years of age. MMWR 43: 1–13
Fernández-Cruz E, Desco M, Garcia Montes M, Longo N, Gonzalez B, Zabay JM 1990 Immunological and serological markers predictive of progression to AIDS in a cohort of HIV-infected drug users. AIDS 4: 987–994
Chomczynski P, Sacchi N 1987 Single step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Ann Biochem 162: 156–159
Muñoz-Fernández MA, Navarro J, García Montes M, Cosín M, Zabay JM, Fernández-Cruz E 1996 Quantification of low levels of HIV-1 RNA viremia in p24-antigen-negative asymptomatic HIV+ patients by use of the polymerase chain reaction. J Clin Microbiol 34: 404–408
Kawasadi ES 1990 Amplification of RNA. In: Innis MA, Gelfand DH, Sninsky JJ White TJ (eds) PCR Protocols: A Guide to Methods and Applications. Academic Press, Berkeley, CA. pp 21–27
Kellog DE, Kwok S 1990 Detection of human immunodeficiency virus. In: Innis MA, Gelfand DH, Sninsky JJ, White TJ (eds) PCR Protocols: A Guide to Methods and Applications. Academic Press, Berkeley, CA, 337–347
Holodniy M, Katzenstein DA, Sengupta S, Wang AM, Casipit C, Schwartz DH, Konrad M, Groves E, Merigan TC 1991 Detection and quantification of human immunodeficiency virus rna in patient serum by use of the polymerase chain reaction. J Infect Dis 163: 862–866
Albert J, Fenyo EM 1990 Simple sensitive, and specific detection of human immunodeficiency virus type 1 in clinical specimens by polymerase chain reaction with nested primers. J Clin Microbiol 28: 1560–1564
García R, Feijoó E, Guerrero MF, Górgola M, Muñoz-Fernández MA, Fernández-Cruz E, Ortíz F 1996 Immune complexes from HIV-1+ patients contains infectious virus able to infect normal lymphocytes. J Allergy Clin Immunol (in press)
Kwok S, Higuchi R 1989 Avoiding false positives with PCR. Nature 339: 237–238
Saiki RK, Scharf S, Faloona F, Mullis KB, Horn GT, Erlich HA, Acnheim N 1985 Enzymatic amplification of β-globin genomic sequences and restriction site analysis for diagnosis of sickle cell anemia. Science 230: 1350–1354
Erice A, Sannerud KJ, Leske VL, Aeppli D, Balfour HH Jr 1992 Sensitive microculture method for isolation of human immunodeficiency virus type 1 from blood leukocytes. J Clin Microbiol 30: 444–448
Navarro J, Pizarro A, Fernández-Cruz E, Fresno M, Muñoz-Fernández MA 1994 Pentoxifylline preferentially inhibits IL-10 production by HIV-1-infected human T cells. AIDS 8: 1192–1194
Scarlatti G, Hodara V, Rossi P, Muggiasca L, Bucceri A, Albert J, Fenyö EM 1993 Transmission of human immunodeficiency virus type 1 (HIV-1) from mother to child correlates with viral phenotype. Virology 197: 624–629
Blanche S, Rouzioux C, Moscato ML, Veber, F Mayaux MJ, Jacomet C, Tricoire J, Deville A, Vial M, Firtion G 1989 A prospective study of infants born to women seropositive for human immunodeficiency virus type 1: HIV infection in Newborns French Collaborative Study Group. N Engl J Med 320: 1643–1648
Blanche S, Tardieu M, Duliega AM, Rouzioux C, Le Deist F, Fukunaga K, Caniglia M, Jacomet C, Messiah A, Griscelli C 1990 Longitudinal study of 94 HIV symptomatic infants with materno-foetal HIV infection: evidence for a bimodal expression of clinical and biological symptoms. Am J Dis Child 144: 1210–1215
Auger I, Thomas P, De Gruttola V, Morse D, Moore D, Williams R, Truman B, Laurence CE 1988 Incubation period for pediatric AIDS patients. Nature 336: 575–577
Johnson JP, Nair P, Hines SE, Seiden SW, Alger L, Revie DR, O'Neil KM, Hebel R 1989 Natural history and serologic diagnosis of infants born to human immunodeficiency virus-infected women. Am J Dis Child 143: 1147–1153
Thomas P, Singht T, Williams R, Blum S 1992 Trends in survival for children with maternally transmitted acquired immunodeficiency syndrome in New York City, 1982-1989. Pediatr Infect Dis J 11: 34–39
Tovo PA, De Martino OM, Gabiano C 1992 Prognostic factors and survival in children with perinatal HIV-1 infection. Lancet 339: 1249–1253
Italian Register for HIV Infection In Children 1994 Features of children perinatally infected with HIV-1 surviving longer than 5 years. Lancet 343: 191–195
Jackson JBB, Kwok SY, Sninsky JS, Hopsicker JS, Sannerud KJ, Rhame FS, Henry K, Simpson M, Balfour HH Jr 1990 Human immunodeficiency virus type 1 detected in all seropositive symptomatic and asymptomatic individuals. J Clin Microbiol 28: 16–19
Boucher CAB, Lange JMA, Miedemal FF, Weverling GJ, Koot M, Mulder JW, Goudsmit J, Kellam P, Larder A, Tersmette M 1992 HIV-1 biological phenotype and the development of zidovudine resistance in relation to disease progression in asymptomatic individuals during treatment. AIDS 6: 1259–1264
Connor RI, Mohri H, Cao Y, Ho D 1993 Increased viral burden and cytopathicity correlate temporally with CD4+ T-lymphocyte decline and clinical progression in human immunodeficiency virus type 1-infected individuals. J Virol 67: 1772–1777
Escaich S, Ritter J, Rougier P, Lepot D, Lamelin JP, Sepetjam M, Trepo C 1991 Plasma viraemia as a marker of viral replication in HIV-infected individuals. AIDS 5: 1189–1194
Palumbo PE, Kwok S, Waters S, Wesley Y, Lewis D, Mickinney N, Bardeguez A, Connor EM, Oleske JM 1995 Viral measurement by polymerase chain reaction-based assays in human immunodeficiency virus-infected infants. J Pediatr 126: 592–595
Vigano A, Principi N, Villa ML, Riva C, Cupi L, Trabbattoni D, Shearer GM, Clerici M 1995 Immunologic characterization of children vertically infected with human immunodeficiency virus, with slow or rapid disease progression. J Pediatr 126: 386–374
Luzuriaga K, Koup RA, Pikota CA, Brettler DB, Sullivan JL 1991 Deficient human immunodeficiency virus type 1-specific cytotoxic T cell response in vertically infected children. J Pediatr 119: 230–236
Acknowledgements
The authors thank Dolores Garcia for her excellent technical assistance. We gratefully acknowledge the expert technical advice and interest of Dr. J. M. Zabay.
Author information
Authors and Affiliations
Additional information
Supported by Grant C134/90 from the Comunidad de Madrid, “Plan Regional de Investigación.”
Rights and permissions
About this article
Cite this article
Muñoz-Fernández, M., Obregón, E., Navarro, J. et al. Relationship of Virologic, Immunologic, and Clinical Parameters in Infants with Vertically Acquired Human Immunodeficiency Virus Type 1 Infection. Pediatr Res 40, 597–602 (1996). https://doi.org/10.1203/00006450-199610000-00014
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199610000-00014