Abstract
Extremely preterm infants have been shown capable of producing glucose at a rate comparable to that of term infants, but virtually no data are available on their capacity for lipolysis and gluconeogenesis. To address this issue, we studied the flux of glycerol and its gluconeogenic contribution to hepatic glucose output by determining the endogenous plasma appearance rate of glycerol (glycerol Ra) and its conversion to glucose in 10 newborn infants, 24-27 wk of gestational age. The study was performed during the 1st d of life by tracer dilution technique using[6,6-2H2]glucose and [2-13C]glycerol given as constant rate i.v. infusions. Plasma isotopic enrichments of the tracers were obtained by gas chromatography/mass spectrometry. Endogenous glycerolRa ranged from 2.4 to 21.6 (median 5.0)μmol·kg-1·min-1, of which 31.5% (25.6-64.4%) was converted to glucose. The glucose production rate averaged 17.5 ± 5.4 μmol·kg-1·min-1 (3.2 ± 1.0 mg·kg-1·min-1), of which 5.0% (1.6-37.6%) was derived from glycerol. The results show that extremely preterm infants, despite limited fat stores, are capable of generating glycerol at a rate within the range reported for term and near term newborns. The infants were also capable of converting part of this glycerol to glucose, providing a contribution to hepatic glucose production comparable to that found in more mature newborns.
Similar content being viewed by others
Main
At birth, the transplacental supply of nutrients is abruptly interrupted, and the newborn infant must produce its own glucose from endogenous substrate stores until feedings are established(1, 2). Initially, glucose is generated mainly from glycogen, but the glycogen stores can provide substrate for only a few hours(3). Therefore, gluconeogenesis from endogenous and exogenous sources of fat and protein is crucial to meet the metabolic requirements, particularly those of the CNS. The initiation of lipolysis and gluconeogenesis is promoted by the hormonal and enzymatic changes occurring over the first 24 h of life, particularly the rapid decrease of the insulin/glucagon ratio(4), but also the high postnatal concentrations of catecholamines, cortisone, and TSH(4–9).
High concentrations of FFA and glycerol as well as rapidly decreasing RQ have been demonstrated soon after birth, indicating an early onset of lipolysis and lipid oxidation(10–14). A few studies have also addressed glycerol kinetics in term and near-term infants in the postnatal period using a stable isotope technique(12, 13, 15). The results from these studies demonstrate considerably higher plasma appearance rates of glycerol in newborn infants compared with fasting adults(16). In the newborns, the major part of glycerol was converted to glucose, contributing 5-20% of hepatic glucose production(12, 13, 15). These findings suggest that fat is an important substrate in the early postnatal period. In extremely preterm infants (<28 wk of gestation) the small glycogen stores(17) are rapidly depleted, and new glucose must be generated from other sources to preserve normoglycemia. We and others(18–22) have shown that these infants can produce glucose at rates close to those reported for term infants at least for short periods of time. To the best of our knowledge neither glycerol turnover nor gluconeogenic contribution of glycerol has previously been determined in this population. Thus, the purpose of the present study was to assess the endogenous appearance rate of glycerol as an indicator of lipolysis, and the utilization of glycerol as a gluconeogenic substrate in extremely preterm infants during the 1st d of life.
METHODS
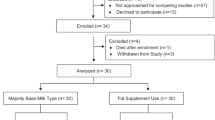
Subjects. The subjects of the study were 10 newborn infants, 26± 1 wk of gestation (Table 1). The gestational age of the infants was estimated by ultrasound examination during pregnancy and was confirmed by maternal menstrual history. All infants were delivered at Uppsala University Hospital and admitted to the neonatal intensive care unit. The study was approved by the Human Ethics Committee of the Medical Faculty of the University of Uppsala. Parental consent was obtained after oral and written information was provided.
The birth weights of the infants ranged from 665 to 1173 g(Table 1), which is within ± 2 SD of the means of the Swedish growth chart(23) (Table 1). Seven of the infants were delivered vaginally (nos. 1, 2, 4, 6, 7, 9, and 10) and three by cesarean section (nos. 3, 5, and 8). All Apgar scores were >7 at 5 and 10 min. The infants were nursed in incubators with a relative ambient humidity of 85-90%. Four of them (nos. 1, 2, 5, and 8) needed intermittent positive pressure ventilation, because of the infant respiratory distress syndrome. The other six infants (nos. 3, 4, 6, 7, 9, and 10) had a mild respiratory disease, requiring treatment with continuous positive airway pressure. All of the infants were normoventilated and normoxemic, 7/10 on air and 3/10 with an oxygen supply of 25, 35, and 60%, respectively. They were clinically stable and had a normal pH and body temperature (36.5-37.5 °C). Theophylline (Aminophylline, Kabi Vitrum, Stockholm, Sweden) (6 mg·kg-1·d-1) was given as apnea prophylaxis to 6/10 infants (nos. 3, 5, 6, 7, 9, and 10). Six of the infants (nos 2, 3, 6, 7, 9, and 10) received antibiotics because of preterm rupture of the membranes, but none of them showed any clinical signs of infection.
The infants were studied at a postnatal age of 17 ± 6 h(Table 1). All were given glucose parenterally directly after birth at a mean rate of 22.78 ± 3.72μmol·kg-1·min-1 (4.1 ± 0.67 mg·kg-1·min-1) until the start of the study. One infant (no. 1) had not been fed orally before the study. The other nine infants had been given small amounts of breast milk (0.5-2 mL every 2 h) from 2 h of age, but had not been orally fed for a minimum of 4 h (4-18 h)(Table 1) before the study. The total intake (parenteral and oral) during the 1st d of life was 65 mL·kg-1.
Isotope tracers. The tracers used were[6,6-2H2]glucose (isotopic purity, 98 atom%) and[2-13C]glycerol (isotopic purity, 98 atom%), purchased from Cambridge Isotope Laboratories, Woburn, MA. The [6,6-2H2]glucose and[2-13C]glycerol were dissolved in a 0.9% saline solution in concentrations of 4.5 and 1.2 mg·mL-1, respectively. The solutions were sterile in microbiologic cultures and pyrogen-free when tested by the Limulus lysate method(24).
Study design. A peripheral vein catheter was inserted for infusion of the tracers and unlabeled glucose, whereas blood samples were obtained from an umbilical artery catheter, inserted for clinical care purposes. To avoid contamination with glucose, catheters used for blood sampling were rinsed and infused with saline throughout the entire study period.
The tracers were administered simultaneously as a primed constant rate infusion for 2 h. For [6,6-2H2]glucose, the priming dose was 27.19 ± 2.06 μmol·kg-1 (4.90 ± 0.37 mg·kg-1), given over 5 min, followed by an infusion rate of 0.66± 0.06 μmol·kg-1·min-1 (0.12 ± 0.01 mg·kg-1·min-1). For [2-13C]glycerol, a priming dose of 14.65 ± 1.28 μmol·kg-1 was given followed by an infusion rate of 0.33 ± 0.03μmol·kg-1·min-1. All infants also received an infusion of 10% glucose given at a rate of 10.0 ± 2.7μmol·kg-1·min-1 (1.8 ± 0.5 mg·kg-1·min-1). No episodes of hypoglycemia(plasma glucose ≤1.6 mM) occurred. The tracer and the unlabeled glucose were infused with calibrated volumetric pumps (IMED 965 micro, IMED, Oxford, England). Blood samples (300 μL/sample; totally 3.1 ± 0.7% of the estimated blood volume) were obtained before the start of the tracer infusion and then every 10 min during the last hour of the 2-h study period. The samples were collected in ice-cold EDTA tubes.
Chemical procedures. Plasma was immediately separated by centrifugation, and the plasma glucose concentration was measured within 5 min by the glucose oxidase-peroxidase method in a glucose analyzer, Ames Minilab 1(Bayer AG, Leverkusen, Germany) as described earlier(18). The remaining plasma was frozen at -70 °C pending further analysis. An internal standard of[1,1,2,3,3-2H5]glycerol (isotopic purity 98%) purchased from Cambridge Isotope Laboratories (Woburn, MA) was added to the plasma samples for quantitation of plasma glycerol. Plasma proteins were precipitated with acetone, and the pentaacetate derivative of glucose and triacetate derivative of glycerol were prepared by addition of equal amounts of pyridine and acetic anhydride. The isotopic enrichments of [6,6-2H2]glucose,[2-13C]glycerol, and [1,1,2,3,3-2H5]glycerol were determined by gas chromatography/mass spectrometry. To control for possible variations in the chemical and gas chromatography/mass spectrometry procedures, glucose and glycerol standards as well as plasma standards of known glucose and glycerol enrichments were always processed along with the study samples. A Finnigan SSQ 70 mass spectrometer (Finnigan MAT, San José, CA) equipped with a Varian 3400 gas chromatograph (Varian Associates Inc., Sunnyvale, CA) with a nonpolar (DB 1) capillary column (15 m× 0.25 mm) was used. The temperature of the oven was set to 180 and 130°C for glucose and glycerol, respectively. Chemical ionization with methane was used with selective monitoring of ions. For glucose the ions monitored were m/z 331, 332, and 333 reflecting unlabeled,13 C-enriched (M + 1) and dideuterated glucose (M + 2). For glycerolm/z 159, 160 and 164 corresponded to unlabeled glycerol,13 C-labeled glycerol (M + 1) and the 5-deuterated internal standard (M+ 5)(15).
The concentrations of insulin and glucagon in plasma were analyzed in microsamples using an RIA technique as described earlier(22, 25). Because of the small plasma volumes available, portions of plasma obtained during the steady state periods were pooled. In two infants (nos. 9 and 10), the amount of plasma available was insufficient for analysis of glucagon, and in another infant (no. 2) neither insulin nor glucagon could be analyzed. TSH was analyzed by noncompetitive sandwich immunofluoroassay (Delfia h TSH Ultra, Wallac OY, Turku, Finland).
Calculations. The glycerol concentrations in plasma were calculated from the ion current ratio 159/164 during periods of approximate steady state (mean CV 9.0 ± 4.4%)(12, 26) using a standard curve. The standard solutions were prepared by adding an amount of the internal standard, equal to that added to the plasma samples, to increasing amounts of unlabeled glycerol. The corresponding CV for plasma glucose concentration was 7.1 ± 3.2%. Appearance rates of glucose and glycerol were calculated from isotopic enrichments of[6,6-2H2]glucose and [2-13C]glycerol obtained during the periods of approximate steady state (mean CV of m/z 333/331, 3.3± 2.6% and of m/z 160/159, 6.1 ± 2.6%), using standard curves obtained by gradually increasing amounts of labeled glucose and glycerol in relation to the corresponding unlabeled compounds. GPR and endogenous glycerol Ra were calculated as follows: GPR = (i × 100/IE) - GIR; endogenous glycerolRa = i × 100/IE where i is the infusion rate of the tracer, IE the isotopic enrichment of the tracer in plasma [given as labeled (tracer)/unlabeled substrate in%], and GIR is the infusion rate of unlabeled glucose(17). GlucoseRa = GPR + exogenous unlabeled and labeled glucose.
In addition, the fraction of glycerol converted to glucose and the fraction of glucose derived from glycerol were calculated from the 13C enrichment of glucose reflected by m/z 332/331 as described by Bougnères et al.(12) and Patel and Kalhan(13).
It was not possible to calculate enteral contributions to the appearance rates of glucose and glycerol. Because the amounts of breast milk given were small and the period without oral feeding before study was at least 4 h(Table 1) a potential enteral contribution of glucose or glycerol must have been very small and was considered negligible.
Statistical analysis. Data are presented as mean ± SD or when not normally distributed as median and range. Spearman's rank test and linear regression analyses were used to test for statistical significance of variables related to plasma appearance rates of glycerol and glucose as well as to GPR, fraction of glycerol converted to glucose, and fraction of hepatic glucose production derived from glycerol. A χ2 test was used to evaluate the influence of theophylline on the appearance rates of glucose and glycerol as well as GPR.
RESULTS
Approximate steady state was achieved 60-90 min after the start of the tracer infusions. The endogenous appearance rate of glycerol and GPR were calculated over these periods lasting for 30-60 min. The endogenous glycerol appearance rate had a median value of 5.0μmol·kg-1·min-1 (2.4-21.6) and the plasma glycerol concentration a median value of 144.5 μmol·L-1(25-1046) (Table 2). About one-third, median 31.5%(25.6-64.4%), of the produced glycerol was converted to glucose.
The glucose production rates ranged from 9.2 to 27.5μmol·kg-1·min-1 (1.7-5.0 mg·kg-1·min-1) with a mean of 17.5 ± 5.4μmol·kg-1·min-1 (3.2 ± 1.0 mg·kg-1·min-1) (Table 2) of which 5.0% (1.6-37.6%) was derived from glycerol. The plasma glucose values ranged from 1.8 to 5.1 mM with a mean of 3.1 ± 1.1 mM(Table 2).
Concentrations of insulin, glucagon, and TSH were also measured during steady state. Insulin and TSH averaged 9.4 ± 5.8 mU·L-1(n = 9) and 5.4 ± 2.5 mU·L-1, respectively, and the median for glucagon was 340 pg·L-1 (range 225-966)(n = 7) (Table 3).
The fraction of hepatic glucose output derived from glycerol was significantly correlated to endogenous glycerol Ra(r = 0.92; p < 0.001) (Fig. 1). Endogenous glycerol Ra as well as the fraction of GPR derived from glycerol were inversely correlated to the insulin concentration in plasma (rs = -0.90; p< 0.01 and rs = -0.85; p < 0.01, respectively). In addition endogenous glycerol Ra was inversely correlated to the lowest recorded body temperature after birth(rs = -0.72; p < 0.05).
Endogenous glycerol Ra did not correlate significantly to gestational age, birth weight, postnatal age, length of period without oral feeding, oral intake before study, GPR, or glucoseRa (Spearman's rank test). Medication with theophylline did not significantly affect endogenous glycerolRa, glucose Ra, or GPR.
DISCUSSION
The results of the present study show that extremely preterm infants(<28 wk) are capable of lipolysis and gluconeogenesis from glycerol on the 1st d of life. These findings show that enzymes and hormones regulating lipolysis and gluconeogenesis are functioning soon after birth. To the best of our knowledge, lipolysis and/or gluconeogenesis from glycerol have previously not been studied in extremely preterm infants. Furthermore, the issues of lipolysis and gluconeogenesis of newborn infants have been addressed only by a limited number of studies(12, 13, 15, 21, 27). These studies, performed in term and near-term infants, showed that alanine contributed about 10% and glycerol 5-20% of hepatic glucose production. The endogenous plasma glycerol appearance rate and the gluconeogenic contribution from glycerol found in our extremely preterm infants varied markedly, but the major part still fell within the ranges reported for the term and slightly preterm infants(12, 13, 15). Only about one-third of glycerol appearing in plasma was converted to glucose compared with the reported 70-90% in more mature infants(12, 13, 15). This finding may indicate that the gluconeogenic pathway via the triose phosphate pool is not completely developed at this gestational age. However, because gluconeogenesis from glycerol correlated directly with the endogenous glycerol Ra, substrate availability may also be a factor limiting gluconeogenesis.
Even if minor, the contribution of glycerol to hepatic glucose output may be crucial to preserve normoglycemia in the extremely preterm infant with its high glucose requirement due to a large brain/body weight ratio(19). In addition, lipolysis not only generates glycerol but also FFA, essential in supporting the process of gluconeogenesis and as precursors for ketone bodies, an alternative important energy fuel for the brain(26, 28, 29).
The intersubject variation with regard to glycerol was greater in our population of preterm infants than in those comprising more mature infants(12, 13, 15). This is not surprising considering the study group was extremely immature. Methodologic reasons for the variation can be excluded, because great precautions were taken to avoid errors in analytical procedures. The study population was homogenous with regard to gestational age and birth weight and included only selected,“healthy” infants with uncomplicated deliveries. However, prenatal factors, such as maternal illness and metabolic status as well as drugs given during pregnancy and delivery, may have an effect on fetal accumulation of body fuel stores and neonatal metabolism.
Factors related to delivery, e.g. fetal and neonatal distress, acidosis, and cooling may also be of importance. The inverse correlation between the lowest temperature recorded after birth and the endogenous glycerol Ra, found in our infants, may indicate that cooling after birth increases lipolysis, probably via the action of catecholamines and TSH(7, 9).
Differences in postnatal age and delivery of exogenous glucose before the study may have influenced utilization of the glycogen stores, resulting in a varying contribution of glucose from glycogenolysis. Furthermore, hormonal changes, occurring in the immediate postnatal period, certainly influence lipolysis and gluconeogenesis. Thus, high catecholamines observed in preterm infants during the first postnatal hours(6) may stimulate lipolysis and gluconeogenesis(30), whereas insulin inhibits both processes(4, 30, 31). Our findings of an inverse relationship between plasma insulin concentration and endogenous glycerol Ra as well as its contribution to hepatic glucose output is consistent with an inhibitory effect of insulin on lipolysis and gluconeogenesis. In contrast, no relationship was found between glucagon or the insulin/glucagon quotient and glycerol kinetics. Inasmuch as the present study was performed at a mean postnatal age of 17 h, the lack of correlation between concentrations of TSH and glycerol production may be due to the fact that rapid changes in TSH concentrations occur as early as the 1st h after birth(9). Although reported data on neonatal glycerol metabolism vary among studies, the appearance and conversion rates of glycerol, as well as its gluconeogenic contribution obtained after 4-6 h without oral feeding, are considerably higher than those reported for adults after an overnight fast(16, 32). These findings indicate that glycerol is a more important gluconeogenic substrate in the early neonatal period than in adult life.
In conclusion the results of this study show that preterm infants are capable of lipolysis during the 1st d of life. In addition, they can use part of the mobilized glycerol for glucose production, thus indicating the presence of functional endocrine and enzyme systems regulating lipolysis and gluconeogenesis. In comparison with term infants, a smaller part of glycerol is converted to glucose, suggesting a less active gluconeogenic pathway.
Abbreviations
- CV:
-
coefficient of variation
- GPR:
-
glucose production rate
- Ra:
-
appearance rate
References
Senior B, Wolsdorf JI 1979 Substrates, gluconeogenesis and hypoglycemia in children. Pediatr Clin North Am 26: 171–185
Ogata ES 1986 Carbohydrate metabolism in the fetus and neonate and altered neonatal glucoregulation. Pediatr Clin North Am 33: 25–45
Bougnères PF 1987 Stable isotope tracers and the determination of fuel fluxes in newborn infants. Biol Neonate 52 ( suppl 1): 87–96
Girard J, Ferré P, Pégorier J-P, Dueé P-H 1992 Adaptation of glucose and fatty acid metabolism during perinatal period and suckling weaning transition. Physiol Rev 72: 507–562
Eliot RJ, Lam R, Leake RD, Hobel CJ, Fisher DA 1980 Plasma catecholamine concentrations in infants at birth and during the first 48 hours of life. Pediatr Res 96: 311–315
Mehandru PL, Assel BG, Nuamah IF, Fanaroff AA, Kalhan SC 1993 Catecholamine response at birth in preterm newborns. Biol Neonate 64: 82–88
Padbury JF, Diakomandis ES, Hobel CJ, Perelman A, Fisher DA 1981 Neonatal adaptation: sympatho-adrenal response to umbilical cord cutting. Pediatr Res 15: 1483–1487
Marcus C, Ehren H, Bolme P, Arner P 1988 Regulation of lipolysis during the neonatal period. Importance of thyrotropin. J Clin Invest 82: 1793–1797
Marchini G, Persson B, Jonsson N, Marcus C 1995 Influence of body temperature on thyrotropic hormone release and lipolysis in the newborn infant. Acta Pediatr 84: 1284–1288
Persson B, Gentz J 1966 The pattern of blood lipids, glycerol and ketone bodies during the neonatal period, infancy and childhood. Acta Paediatr Scand 55: 353–362
Hawdon JM, Ward Platt MP, Aynsley-Green A 1992 Patterns of metabolic adaptation for preterm and term infants in the first neonatal week. Arch Dis Child 67: 357–365
Bougnères PF, Karl IE, Hillman LS, Bier DM 1982 Lipid transport in the human newborn. Palmitate and glycerol turnover and the contribution of glycerol to neonatal hepatic glucose output. J Clin Invest 70: 262–270
Patel D, Kalhan S 1992 Glycerol metabolism and triglyceride-fatty acid cycling in the human newborn: effect of maternal diabetes and intrauterine growth retardation. Pediatr Res 31: 52–58
Cross KW, Tizard JPM, Trythall DAH 1957 The gaseous metabolism of the newborn infant. Acta Pediatr Scand 46: 265–285
Fjeld CR, Cole FS, Bier DM 1992 Energy expenditure, lipolysis, and glucose production in preterm infants treated with theophylline. Pediatr Res 32: 693–698
Bortz MW, Paul P, Haff AC, Holmes WL 1972 Glycerol turnover and oxidation in man. J Clin Invest 51: 1537–1546
Widdowson EM, Spray CM 1951 Chemical development in utero. Arch Dis Child 26: 205–214
Sunehag A, Ewald U, Larsson A, Gustafsson J 1993 Glucose production rate in extremely immature neonates (<28 wk) studied by use of deuterated glucose. Pediatr Res 33: 97–1001
Bier DM, Leake RD, Moey WH, Arnold KJ, Gruenke LD, Sperling MA, Kipnis DM 1977 Measurement of “true” glucose production rates in infancy and childhood with 6,6-dideuteroglucose. Diabetes 26: 1016–1023
Tyrala EE, Chen X, Boden G 1994 Glucose metabolism in the infant weighing less than 1100 grams. J Pediatr 125: 283–287
Kalhan SC, Bier DM, Savin SM, Adam PAJ 1978 Estimation of glucose turnover and 13C recycling in the human newborn by simultaneous [1-13C]glucose and [6,6-2H2]glucose tracers. J Clin Endocrinol Metab 1980: 456–460
Sunehag A, Gustafsson J, Ewald U 1994 Extremely immature infants respond to glucose infusion with incomplete suppression of glucose production. Pediatr Res 36: 550–555
Niklasson A, Ericson A, Fryer J G, Karlberg J, Lawrence C, Karlberg P 1991 An update of the Swedish reference standards for weight, length and head circumference at birth for given gestational age (1977-1981). Acta Paediatr Scand 80: 756–762
Guideline on validation of the Limulus amebocyte lysate test as an end-product endotoxin test for human and animal parenteral drugs, biological products, and medical devices. Food and Drug Administration, U.S.A., December 1987
Faloona GR, Unger RH 1974 Glucagon radioimmunoassay technique. In: Jaffe BM, Behrman HE (eds) Methods of Hormone Radioimmunoassay, Vol 1. Academic Press, New York, pp 317–330
Bougnères PF, Lemmel C, Ferré Bier DM 1986 Ketone body transport in the human neonate and infant. J Clin Invest 77: 42–48
Frazer TE, Karl IE, Hillman LS, Bier DM 1981 Direct measurement of gluconeogenesis from [2,3-13C2]alanine in the human neonate. Am Physiol E615–E621
Owen OE, Morgan AP, Kemp HG, Sullivan JM, Herrera MG, Cahill GF Jr 1967 Brain metabolism during fast. J Clin Invest 46: 1589–1595
Persson B, Settergren G, Dahlquist G 1972 Cerebral arteriovenous difference of acetoacetate and D-β-hydroxybutyrate in children. Acta Paediatr Scand 64: 17–24
Cowett RM 1991 Neonatal glucose metabolism. In: Cowett RM (ed) Principles of Perinatal-Neonatal Metabolism. Springer-Verlag, New York pp 356–389
Arner P, Bolinder J, Östman J 1983 Glucose stimulation of the antilipolytic effect of insulin in humans. Science 20: 1057–1058
Beylot M, Martin C, Beaufrere B, Riou JP, Mornex R 1987 Determination of steady-state and nonsteady-state glycerol kinetics in humans using deuterium-labeled tracer. J Lipid Res 28: 414–422
Acknowledgements
The authors thank Elisabeth Söderberg, Gert Hedow, the staff of the NICU Uppsala University Children's Hospital, Anders Ingvast, and Ulf Bondesson, SVA Uppsala, for skillful assistance, as well as Claes Göran Östensson and Elvy Sandberg, Karolinska Institute, Stockholm, for analyses of insulin and glucagon.
Author information
Authors and Affiliations
Additional information
Supported by grants from the Swedish Medical Research Council (Projects 4792 and 11282), Novo Nordisk Pharma AB, the Samaritan Foundation, the Gillberg Foundation, the General Maternity Hospital Foundation, the Jerring Foundation, the Swedish Society for Medical Research, and the Mutual Group Life Insurance Company, Stockholm, Sweden.
Rights and permissions
About this article
Cite this article
Sunehag, A., Ewald, U. & Gustafsson, J. Extremely Preterm Infants (<28 Weeks) Are Capable of Gluconeogenesis from Glycerol on Their First Day of Life. Pediatr Res 40, 553–557 (1996). https://doi.org/10.1203/00006450-199610000-00007
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199610000-00007
This article is cited by
-
Hyperglycemia and prematurity: a narrative review
Pediatric Research (2023)
-
Increased and early lipolysis in children with long‐chain 3‐hydroxyacyl‐CoA dehydrogenase (LCHAD) deficiency during fast
Journal of Inherited Metabolic Disease (2015)
-
Increased lipolysis in LCHAD deficiency
Journal of Inherited Metabolic Disease (2007)