Abstract
Bacterial translocation (BT) from the gastrointestinal tract has been thought to play a role in the pathogenesis of septic complications in patients with chronic portal hypertension (PH) and obstructive jaundice. The purpose of this study was to investigate the incidence of BT and to assess the role of intestinal mucosal malondialdehyde (MDA) levels as an indicator of lipid peroxidation and polymorphonuclear neutrophil-derived myeloperoxidase (MPO) in chronic portal hypertensive and common bile duct-ligated rats. Twenty male rats were subjected to sham laparotomy (SL), 20 rats to calibrated portal vein constriction (PH), 20 rats to common bile duct ligation (CBDL), and 10 rats served as a nonoperated control group (NOP). After 4 wk, 10 animals of each operated group received 50 mg/kg allopurinol intraperitoneally, at 24 h, and again 2 h prior to estimation of BT, intestinal mucosal MDA, and MPO activities. In the NOP and SL groups, BT to the mesenteric lymph nodes (MLN) and spleen was present. In PH and in CBDL rats, BT to liver, portal vein, peritoneum, and caval vein occurred. Allopurinol treatment attenuated the frequence of BT in PH and decreased BT in CBDL rats significantly (p< 0.05). Ileal mucosal MDA levels (nanomoles/g) in untreated rats increased from 45,1 ± 7.9 in SL to 98.2 ± 9.1 in PH and to 102.2 ± 11 in CBDL rats (p < 0.01). In the allopurinol groups the increase of MDA to 49.1 ± 1.3 in PH, and 66.2 ± 2.2 in CBDL was significantly lower (p < 0.01). MPO activity (units/g) in the ileal mucosa increased in untreated rats from 319 ± 129 after SL to 866± 104 after PH and to 1016 ± 104 after CBDL (p < 0.01). Allopurinol significantly attenuated MPO activity to 369 ± 44 in PH, and to 372 ± 60 in CBDL animals (p < 0.01). In PH and CBDL rats significant BT, intestinal mucosal lipid peroxidation, and polymorphonuclear neutrophil-derived MPO activity occurred. Allopurinol reduced BT and improved intestinal mucosal MDA and MPO activities, suggesting that there might be an association between BT and intestinal mucosal lipid peroxidation.
Similar content being viewed by others
Main
According to some reports in chronic PH and obstructive jaundice, spontaneous bacterial peritonitis, cholangitis, bacteremia, and sepsis are complications resulting in high morbidity and mortality rates(1–3). Especially in patients with congenital biliary atresia, most postoperative complications are related to bacterial cholangitis and to chronic PH(4). The exact pathophysiologic mechanism of this increased risk of infection remains unclear. PH is a consequence of hepatic fibrosis and increased intrahepatic vascular resistance in long-term survivors with congenital biliary atresia. Recent studies have demonstrated that chronic PH disrupts the intestinal mucosal barrier and creates a predisposition to extraluminal egress of intestinal bacteria, a process termed BT(5–8). Chronic PH leads to a hyperdynamic splanchnic flow state, but intestinal mucosal hypoperfusion and hypoxia might also occur(9). It is believed that hypoxia initiates oxidative damage to the intestinal integrity by an increased conversion of xanthine dehydrogenase to XO and the formation of various oxygen-derived free radicals(10, 11). The small intestine is one of the richest sources of XO that triggers the initial generation of oxidants which leads to intestinal lipid peroxidation(12). Additional XO-derived reactive oxygen metabolites increase polymorphonuclear neutrophil accumulation in a vascular-compromised intestine, and oxygen metabolites are the most destructive toxins released from the neutrophils(13–15). These toxic oxygen metabolites disrupt the intestinal mucosal barrier function which prevents the egress of indigeneous intestinal bacteria(12).
On the basis of these considerations, the aim of this study was to investigate the incidence of BT in chronic portal hypertensive and common bile duct-ligated rats, and to assess the role of intestinal mucosal lipid peroxidation and polymorphonuclear neutrophil-derived MPO activity. We estimated ileal mucosal MDA, as an indicator of lipid peroxidation, and ileal mucosal MPO, as an indicator of activated neutrophils, and examined the effect of allopurinol, a competitive XO inhibitor(16).
METHODS
Seventy 4-wk-old male Sprague-Dawley rats (110-130 g of body weight) were used for these studies. All experiments were conducted with the permission of the animal research commission of the Ministery of Science of Austria following local guidelines for the care and use of laboratory animals. The rats received a standard pellet diet and water ad libitum and were housed in an environmentally controlled vivarium with a 12-h light-dark cycle. For all surgical procedures, anesthesia was induced by intraperitoneal injection of ketamine (100 mg/kg of body weight). The animals were randomly assigned to the NOP and to one of the three operative groups.
NOP. Ten rats were not operated and served as a control group to determine the normal rate of BT and ileal colonization.
SL. The 20 rats in the SL group were anesthetized, and under sterile conditions a 2-cm celiotomy was performed. The portal vein and the common bile duct were dissected free, and the abdominal wall was closed in two layers with interrupted absorbable 4-0 sutures.
Chronic PH. Chronic PH was produced in 20 rats by calibrated constriction of the portal vein as described by Chojkier and Groszmann(17). Briefly, through an upper midline incision the common portal vein was dissected free, and a ligature of 3-0 silk was placed around the vein. A 20-gauge blunt needle was placed alongside the vein, and the ligature was tied snugly to the needle and vein. The needle was removed to yield a calibrated stenosis of the portal vein.
CBDL. Twenty rats were subjected to obstructive jaundice induced by CBDL. Through an upper midline abdominal incision the common bile duct was identified and ligated with a 3-0 silk ligature. All ligatures were placed in the same position in all rats.
During the postoperative period all animals were fed a standard pellet diet and water ad libitum to assure similar nutritional intake.
Treatment groups. After 4 wk the three operated groups (SL, PH, CBDL) were divided into two subgroups of 10 animals each, in one untreated group, and in one treatment group. In the treatment group, animals received allopurinol 50 mg/kg intraperitoneally 24 h and again 2 h before analysis (The Wellcome Foundation Ltd., London, UK). In the untreated subgroups, aliquots of 0.9% saline were injected intraperitoneally.
Experimental design. Animals were weighed and reanesthetized with ketamine, and a laparotomy from the xiphoid to the pubis was performed. Using sterile technique, the skin flaps were reflected and the abdominal muscles were treated with 70% ethanol before the abdominal cavity was opened. The exposed viscera were swabbed with sterile cotton-tipped applicator sticks, which were placed immediately on blood agar plates. Portal pressure was measured after cannulating the superior mesenteric vein with a 21-gauge needle connected to a manometer filled with saline. The height of the right atrium was taken as the zero reference level.
Blood samples were collected from the inferior vena cava for the measurement of total bilirubin, aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, and lactate dehydrogenase with a Cobas Mira multianalyzer (Hoffmann LaRoche Ltd., Basel, Switzerland).
Aliquots of 0.1 mL of portal vein blood and inferior caval vein blood were plated onto blood agar. The central MLN complex was excised with sterile instruments. With use of separate instruments, the liver and spleen were removed to determine total organ weight. A 1.5-cm long part of the terminal ileum was excised, opened on its antimesenteric border, and washed in sterile 0.9% saline. The MLDs, parts of the liver, spleen, and ileum were weighed and placed in grinding tubes containing the 1:9 volume of sterile brain-heart infusion (BioMerieux, Marcy l'Etoile, France), and homogenized. Serial dilutions of the homogenates were carried out, and 0.1 mL of each dilution was plated an blood agar, endo agar, and MRS agar and incubated aerobically at 37°C for 48 h. The plates were evaluated for bacterial growth by standard bacteriologic technique. Any growth in the plates of bacteria of the same biotype as cultured in the ileum was considered positive and measured as a CFU/g.
For MDA and MPO determination, ileal mucosa was scraped off and weighed. All specimens were immediately frozen in liquid nitrogen until assay. Specimens of the the ileal mucosa were also taken to determine the dry weight. Dry weight was determined after incubation of specimens of ileal mucosa at 50°C for 48 h. MDA was determined as an index of lipid peroxidation according to the method of Wong et al.(18). MPO was assayed using the method of Krawisz et al.(19). MDA values were expressed as nanomoles/g of dry weight of ileal mucosa and MPO activities as units/g of dry weight of ileal mucosa.
Samples of jejunum, ileum, and liver were removed for histologic examination. The tissues were fixed in 10% buffered formalin, embedded in paraffin, cut into 2-3-μm serial sections, and stained with hematoxylin-eosin and chrome-aniline blue. A blind evaluation of the histologic sections was conducted by a pathologist.
Statistical analysis. The results are expressed as mean± SD. Data from experiments between the means of two groups were statistically tested using a t test, and analysis of variance was used to compare more than two groups. A p value of <0.05 or less was considered statistically significant in all analyses.
RESULTS
After 4 wk, all SL animals had a patent portal vein and common bile duct. In rats with a calibrated portal vein stenosis, a stenotic but patent portal vein with dilated mesenteric veins was present. All CBDL animals became visibly jaundiced with a cystic common bile duct remnant proximal of the ligature. In all animals, adequate portal constriction and bile duct ligation were confirmed. Weight gain, portal pressure, serum liver enzymes, and total liver and spleen weight are presented in Table 1. There was a significant difference in weight gain between SL and NOP rats and chronic PH and CBDL animals (p < 0.05). Mean portal pressures was significantly higher (p < 0.01) in all chronic PH and CBDL rats compared with the NOP and SL groups. Bilirubin, alanine aminotransferase, aspartate aminotransferase, and alkaline phosphatase were significantly elevated in the CBDL groups (p < 0.01), without a difference between treated and untreated rats. Total liver weight (expressed as percent of total body weight) demonstrated a significant increase only in CBDL animals(p < 0.01), and total spleen weight was 2-3-fold higher in all chronic PH and CBDL animals (p < 0.01).
BT and ileal colonization. In all animals, BT of enteric organisms to the spleen and MLDs occurred (Table 2). Whereas in the NOP and SL groups, 82% lactobacilli translocated, in the chronic PH and CBDL groups 75% enterococci and Escherichia coli were cultured from MLDs and spleen. Untreated PH and CBDL further resulted in BT to the peritoneum, caval vein blood, portal vein blood, and liver, which was not present in the NOP and SL groups. Translocating micro-organisms most often cultured were enterococci, E. coli, streptococci, and Pasteurella species. The quantitative analysis of translocating bacterias showed in the NOP and SL groups and in the allopurinol-treated chronic PH and CBDL groups CFU/g tissue between 100 and 1000 bacteria. In the untreated chronic PH and CBDL animals, the amount of translocating bacteria significantly increased to 1,000-10,000 bacteria per CFU/g tissue (p< 0.05).
In the allopurinol-treated group of chronic PH, no BT to the peritoneum, caval vein blood, and portal vein blood occurred. In CBDL animals, allopurinol treatment resulted in a significant decrease of BT (p < 0.05) to the portal vein and liver, and BT to peritoneum, caval vein blood, and portal vein blood was not found.
Chronic PH resulted in a significant bacterial overgrowth in the ileum(p < 0.05) of Gram-positive bacteria, whereas in CBDL rats a bacterial overgrowth with Gram-positive and Gram-negative intestinal bacteria was present, without any difference between untreated and allopurinol-treated animals (Table 2).
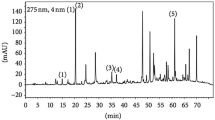
MDA and MPO assays (Figs. 1 and 2). MDA (nanomoles/g) in the ileal mucosa increased significantly (p< 0.01) in untreated chronic PH (98.2 ± 9.1) and untreated CBDL rats(102.2 ± 11) when compared with the NOP (43 ± 7.2) and SL rats(45.1 ± 7.9). Similarly, MPO activity (units/g) in the ileal mucosa was significantly elevated (p < 0.01) in untreated chronic PH (866± 104) and CBDL animals (1016 ± 104) when compared with the NOP(342 ± 98) and SL group (319 ± 129). In the allopurinol-treated groups (SL, 36.4 ± 1.6; PH, 49.1 ± 1.3; CBDL, 66.2 ± 2.2), significant lower MDA levels were present (p < 0.01). MPO activity in allopurinol treated animals rose from 281 ± 47 in SL to 369± 44 in chronic PH and to 372 ± 60 in CBDL animals, and these levels were significantly lower compared with the untreated groups of chronic PH and CBDL (p < 0.01).
Histology. Sections of the liver and jejunum and ileum were examined by light microscopy. The liver was normal in all SL and chronic PH rats. CBDL resulted in fine nodular changes of the liver parenchyma. Microscopically, periportal fibrosis, biliary hyperplasia, and bile duct proliferation were present (grade III of liver fibrosis) without any differences between untreated and allopurinol-treated animals. In the ileum, the mucosa, lamina propria, and submucosa were without any visible histopathology in all untreated and treated SL, chronic PH, and CBDL animals. In the jejunum a mild mucosal atrophy with decreased villus height was present.
DISCUSSION
Patients with chronic PH and obstructive jaundice have an increased susceptibility to severe infections, spontaneous bacterial peritonitis, cholangitis, and bacteremia(2, 3, 20). The incidence of these complications in adults is reported in the literature as ranging between 8% and 25%, reaching a mortality of 78%(1, 2). Ninety-five percent of these infections are caused by aerobic organisms of enteric origin(21). In infants, one of the most common cholestatic diseases is congenital biliary atresia. Since the introduction of hepatic portoenterostomy by Kasai, a jaundice disappearance rate of 81% was achieved(22). The main complication of hepatic portoenterostomy is cholangitis, with a reported incidence ranging from 40 to 60%(22). Its occurrence can result in cessation of bile flow, and repeated attacks can cause progressive deterioration of liver function leading to biliary cirrhosis. The exact mechanism causing cholangitis is unclear. Whether it is an ascending bacterial infection, reaching intrahepatic bile ducts via the portoenterostomy, or an hematogeneous spread of intestinal bacteria to the liver is still under discussion(23, 24). The second complication after portoenterostomy for biliary atresia is PH, frequently present in long-term survivors, and caused by progressive hepatic fibrosis.
Several clinical and experimental studies were undertaken to define mechanisms which lead to disruption of intestinal mucosal barrier function and translocation of indigeneous bacteria in PH and obstructive jaundice(5, 7, 8). Isolated chronic PH is characterized by a pathologic increase of portal pressure and the formation of a network of portasystemic collaterals, diverting the portal blood stream to the systemic circulation, bypassing a normal liver. PH increases microvascular intestinal blood flow, but this is associated with a 41-51% decrease of intestinal arterial pressure, thus leading to hypoperfusion and hypoxia(9, 25). This hyperdynamic circulatory state with splanchnic vasodilatation but mucosal hypoperfusion produces structural changes in the bowel mucosa initiated by mucosal hypoxia and by activation of intestinal mucosal XO(6, 7, 26). Generated oxygen-derived free radicals act as promotors for increased intestinal permeability, and they trigger attractants which have the ability to release a complex of reactive oxygen metabolites that can destroy normal cells and disolve connection tissue(27). An ongoing oxidative stress leads to a continuing cell membrane lipid peroxidation and cell death(28–30). In previous studies the role of lipid peroxidation on intestinal permeability and liver injury by activating XO, and the subsequent generation of oxygen-derived free radicals triggering BT has been detected in intestinal and hepatic ischemic conditions(12, 13, 15). However, until now there was no information about the relationship between BT and intestinal lipid peroxidation in chronic PH and CBDL.
In this study we investigated BT and the role of intestinal mucosal lipid peroxidation and polymorphonuclear neutrophil-derived intestinal MPO activity in growing rats with chronic PH and CBDL, and we evaluated the effect of allopurinol, a competitive XO inhibitor.
In the NOP and SL groups, BT only to the MLN and spleen was present. This corresponds to previous studies were BT was found under normal conditions, and it is believed that this phenomenon of BT to the MLN and spleen is a physiologic process which is necessary for immunologic maturation(31, 32).
Chronic PH, isolated or as a sequelae of hepatic fibrosis, leads to a vascular congestion of the bowel with chronic hypoxemia of the intestinal mucosa, and it disrupts the normal intestinal ecology, resulting in bacterial overgrowth. An increased conversion of xanthine dehydrogenase to XO in intestinal hypoxemic conditions is a well known phenomenon(14). XO alters intestinal mucosal membranes by lipid peroxidation and promotes polymorphonuclear neutrophil infiltration into the bowel triggered by XO derived free radical metabolites(12). XO and polymorphonuclear neutrophil accumulation mediate tissue damage by the release of toxic oxygen products, and so may further increase intestinal permeability for bacteria(27, 33). In chronic PH our results showed an increase of BT and a significant ileal bacterial overgrowth with Gram-positive bacteria. BT to the peritoneum, vena cava, portal vein, and liver occurred, indicating a systemic invasion of enteric bacteria. This is in contrast to other studies, where BT occurred only in acute PH or in chronic PH in association with hemorrhagic shock(6, 7). In a previous study in young piglets with acute PH induced by temporary portal vein occlusion and portal reperfusion, we found significant BT to portal blood, liver, spleen, and MLN, and the incidence of BT was similar to the present study of chronic PH(34). These reported differences in BT might be attributed to the fact that we analyzed growing animals after 4 wk of PH, whereas in the other studies BT was investigated after 14 d of PH in adult animals(6, 7). A further possible explanation for the differences in BT between growing and adult animals might be a decreased resistance of the intestinal mucosal barrier function against bacteria during the maturation of intestinal integrity(35). Ileal mucosal lipid peroxidation and polymorphonuclear neutrophil-derived MPO activity in the ileal mucosa increased significantly in untreated PH animals. Allopurinol treatment in chronic PH rats decreased BT, ileal mucosal MDA, and MPO activities.
In obstructive jaundice, the absence of intestinal bile flow, impaired reticuloendothelial system function and immunity, intestinal bacterial overgrowth, and physical disruption of the gut mucosal barrier by secondary chronic PH explain the high incidence of infectious complications(5, 8, 36, 37). The absence of intestinal bile flow alters the gut microflora, and the lack of intraluminal secretory IgA together with an impaired Kupffer cell function promote BT(38–40). High plasma concentrations of lipid peroxides in obstructive jaundice are believed to be an important mediator not only for liver fibrosis, but also for intestinal bacterial colonization and neutrophil infiltration into the bowel(15, 30). In CBDL, the incidence of positive bacterial cultures increased, and bacteria of enteric origin could be cultured in the portal vein, vena cava, liver, spleen, and MLNs. There was additionally a significant ileal bacterial overgrowth with Gram-positive and Gram-negative bacteria. Significant intestinal lipid peroxidation and polymorphonuclear neutrophil derived MPO activity occurred. Allopurinol treatment improved BT and intestinal MDA and MPO activities.
Allopurinol, a competitive XO inhibitor and free radical scavenger, was effective in inhibiting intestinal mucosal lipid peroxidation in PH and CBDL rats, which resulted in decreased MDA levels in the ileal mucosa. Subsequently, polymorphonuclear neutrophil-derived MPO activity in the ileal mucosa was significantly lower, indicating that lipid peroxides may act as chemoattractants for polymorphonuclear neutrophils. Prevention of lipid peroxidation reduces polymorphonuclear neutrophil infiltration into the intestinal mucosa. Both decreased mucosal MDA and MPO levels were associated with a significantly lower incidence of BT, despite a bacterial overgrowth in the ileum. Considering this, bacterial overgrowth itself cannot be the principle mechanism responsible for BT in PH and CBDL animals. Under light microscopy, the jejunum and ileum of chronic PH and CBDL rats were without any major histopathologic findings. Histologic alterations in chronic PH and CBDL are believed to occur at the subcellular levels in the intestinal mucosa. Alterations of cell membranes and disruption of tight junctions may initiate an increased bacterial adherence to the mucosa cell, which is an important step in the translocation process, and promote the intra- and intercellular escape of intestinal bacteria(41, 42). Out of these considerations, in chronic PH and CBDL rats, intestinal mucosal lipid peroxidation might play an associated role required for BT. Electron microscopic investigations and intestinal permeability studies will be necessary to investigate the exact mechanisms of how bacterias leave the intestinal lumen in chronic PH and CBDL rats through an apparently intact mucosa as present in light microscopic examinations. The mechanism leading to BT is probably a disruption of the intestinal barrier at subcellular levels,e.g. tight junctions, or at other levels of the intestine by lipid peroxidation or by toxic metabolites released from activated polymorphonuclear neutrophils. But the exact mechanism of BT in chronic PH and CBDL rats could not be clarified in the present study.
In this study in growing rats with chronic PH and CBDL we have found significant BT, intestinal mucosal lipid peroxidation, and polymorphonuclear neutrophil-derived mucosal MPO activity. BT in chronic PH and CBDL rats was associated with significant intestinal mucosal lipid peroxidation and by subsequent activation of polymorphonuclear neutrophils. Allopurinol, a competitive XO inhibitor, significantly reduced BT, intestinal mucosal lipid peroxidation, and mucosal MPO activity in chronic PH and CBDL rats. However, the clinical relevance of the present study in growing rats remains speculative, because rats are very different from humans with respect to distribution of XO activities in the liver and intestine(43–45). But essential data concerning the intestinal and hepatic activity of XO in humans with PH and cholestasis are lacking and remain to be studied.
Abbreviations
- BT:
-
bacterial translocation
- CBDL:
-
common bile duct ligation
- CFU:
-
colony-forming unit
- MLN:
-
mesenteric lymph node
- MDA:
-
malondialdehyde
- MPO:
-
myeloperoxidase
- NOP:
-
nonoperative group
- PH:
-
portal hypertension
- SL:
-
sham laparotomy
- XO:
-
xanthine oxidase
References
Gilgert JA, Kamath PS 1995 Spontaneus bacterial peritonitis: an uptate. Mayo Clin Proc 70: 365–370
Mihas AA, Toussaint J, Hsue HS, Dotherow P, Achord JL 1992 Spontaneous bacterial peritonitis in cirrhosis: clinical and laboratory features, survival and prognostic indicators. Hepatogastroenterol 39: 520–522
Chiba T, Ohi R, Nio M, Ibrahim M 1991 Late complications in long-term survivors of biliary atresia. Eur J Pediatr Surg 2: 22–25
Ohi R, Nio M, Chiba T 1990 Long-term follow-up after surgery for patients with biliary atresia. J Pediatr Surg 25: 442–445
Deitch EA, Sitting K, Li M, Berg RD, Specian RD 1990 Obstructive jaundice promotes bacterial translocation from the gut. Am J Surg 159: 79–84
Sorell WT, Quigley EMM, Jin G, Johnson TJ, Rikkers LF 1993 Bacterial translocation in portal-hypertensive rat: studies in basal conditions and on exposure to hemorrhagic shock. Gastroenterology 104: 1722–1726
Garcia-Tsao G, Albillos A, Barden GE, West AB 1993 Bacterial translocation in acute and chronic portal hypertension. Hepatology 17: 1081–1085
Llovet JM, Bartoli R, Planas R, Cabre E, Jiminenez M, Urban A, Ojanguren I, Arnal J, Gassull MA 1994 Bacterial translocation in cirrhotic rats. Its role in the development of spontaneous bacterial peritonitis. Gut 35: 1648–1652
Vorobioff J, Bredfeldt JE, Groszmann RI 1983 Hyperdynamic circulation in portal hypertensive rat model: a primary factor for maintenance of chronic portal hypertension. Am J Physiol 244:G52–G56
Deitch EA, Ma WJ, Ma L, Berg R, Specian RD 1989 Endotoxin induces bacterial translocation: a study of mechanisms. Surgery 106: 292–300
Deitch EA, Taylor M, Grisham M, Ma L, Bridges W, Berg R 1989 Endotoxin induces bacterial translocation and increases xanthine oxidase activity. J Trauma 29: 1679–1683
Otamiri T 1989 Oxygen radicals, lipid peroxidation, and neutrophil infiltration after small-intestinal ischemia and reperfusion. Surgery 105: 593–599
Liao XP, She YX, Liu SL, Li M 1995 Injurious effects of oxygen free radicals on human intestinal epithelial cells and their prevention. Pediatr Surg Int 10: 97–100
Miller DM, Grover TA, Nayini N, Aust SD 1993 Xanthine oxidase-an iron-dependent lipidperoxidation. Arch Biochem Biophys 301: 1–7
Muriel P, Suarez OR 1994 Role of lipid peroxidation in biliary obstruction. J Appl Toxicol 14: 423–426
Das DK, Engelman RM, Clement R, Otani H, Prasad MR, Rao PS 1987 Role of XO-inhibitors as free radical scavenger: a novel mechanism of allopurinol and oxypurinol in myocardial salvage. Bichem Biophys Res Commun 148: 314–319
Chojkier M, Groszmann RJ 1981 Measurement of portal-systemic shunting in the rat using γ-labeled microspheres. Am J Physiol 240:G371–G357
Wong SHY, Knight JA, Hopfer SM, Zaharia O, Leach CN, Sunderman FW 1987 Lipidperoxides in plasma as measured by liquid-chromatographic separation of malondialdehyde-thiobarbituric acid adduct. Clin Chem 33: 214–222
Krawisz JE, Sharon P, Stenson WF 1984 Quantitative assay for acute intestinal inflammation based on myeloperoxidase activity: assessment of inflammation in rat and hamster models. Gastroenterology 87: 1344–1350
Wyke RJ 1987 Problems of bacterial infection in patients with liver disease. Gut 28: 623–641
Garcia-Tsao G 1992 Spontaneous bacterial peritonitis. Gastroenterol Clin North Am 21: 257–275
Ohi R, Ibrahim M 1992 Biliary atresia. Semin Pediatr Surg 1: 115–124
Altman RP, Chandra R, Lilly JR 1975 Ongoing cirrhosis after successful portoenterostomy. J Pediatr Surg 10: 685–691
Laurent J, Gauthier F, Bernard O, Hadchovel N, Odievre N, Valayer J, Alagille D 1990 Long-term outcome after surgery for biliary atresia. Gastroenterology 99: 1795–1797
Blanchet L, Lebrec D 1982 Changes in splanchnic blood flow in portal hypertensive rats. Eur J Clin Invest 12: 327–331
Deitch EA, Bridges W, Baker J, Ma JW, Ma L, Grisham MB, Granger N, Specian RD, Berg R 1988 Hemorrhagic shock-induced bacterial translocation is reduced by xanthine oxidase inhibition or inactivation. Surgery 104: 191–198
Weiss SJ 1989 Tissue destruction by neutrophils. N Eng J Med 320: 365–376
Comporti M 1989 Three models of free radical induced cell injury. Chem Biol Interact 72: 1–7
Tripple DL, Yee AW, Jones DP 1976 The pathophysiological significance of lipid peroxidation in oxidative cell injury. Hepatology 7: 377–387
Kato S, Kawase T, Alderman J 1990 Role of xanthine oxidase in ethanol-induced lipid peroxidation in rats. Gastroenterology 98: 203–210
Berg RD, Garlington AW 1979 Translocation of certain indigenous bacteria from the gastrointestinal tract to the mesenteric lymph nodes and other organs in a gnotobiotic mouse model. Infect Immun 23: 403–411
Steffen EK, Berg RD, Deitch EA 1988 Comparison of translocation rates of various indigenous bacteria from the gastrointestinal tract to the mesenteric lymph node. J Infect Dis 157: 1032–1038
Van Bebber IP, Boekholz WK, Goris RJ 1989 Neutrophil function and lipid peroxidation in a rat model of multiple organ failure. J Surg Res 47: 471–475
Schimpl G, Höllwarth ME, Khoschsorur G, Sixtl-Voigt B, Mayr J, Fasching G, Haberlik A, Steinwender G, Rieberer ML, Gössler R 1994 Effect of a portojugular shunt and allopurinol on bacterial translocation induced by temporary portal vein occlusion. Pediatr Surg Int 9: 254–257
Smith SD, Cardona MA, Wishnev SA, Kurchubasche AG, Rowe MI 1992 Unique characteristics of the neonatal intestinal mucosal barrier. J Pediatr Surg 27: 333–338
Ding JW, Andersson R, Soltesz V, Willen R, Bengmark S 1993 The role of bile and bile acids in bacterial translocation in obstructive jaundice rats. Eur Surg Res 25: 11–19
Rimola A, Soto R, Bory F, Arroyo V, Piera C, Rodes J 1984 Reticuloendothelial system phagocytic activity in cirrhosis and its relation to bacterial infections and prognosis. Hepatology 4: 53–58
Sung JY, Costerton JW, Shaffer EA 1992 Defense system in the biliary tract against bacterial infection. Digest Dis Sci 37: 689–696
Slocum MM, Sittig KM, Specian RD, Deitch EA 1990 Absence of intestinal bile promotes bacterial translocation. Am Surg 159: 79–84
Van Bossuyt H, Desmaretz C, Gaeta GB, Wisse E 1990 The role of bile acids in the development of endotoxemia during obstructive jaundice in the rat. J Hepatol 10: 274–279
Alexander JW, Boyce ST, Babcock GF, Gianotti L, Peck MD, Dunn DL, Pyles T, Childress CP, Ash SK 1990 The process of microbial translocation. Ann Surg 121: 496–512
Wells CL, Maddaus MA, Simmons RL 1988 Proposed mechanisms for the translocation of intestinal bacterias. Rev Infect Dis 10: 958–969
Parks DA, Granger DN 1986 Xanthine oxidase: biochemestry, distribution, and physiology. Acta Physiol Scand Suppl 548: 87–99
Wajner M, Harkness RA 1989 Distribution of xanthine dehydrogenase and oxidase activities in human and rabbit tissues. Biochim Biophys Acta 991: 79–84
Vettenranta K, Raivo KO 1990 Xanthine oxidase during human fetal development. Pediatr Res 27: 286–288
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Schimpl, G., Pesendorfer, P., Steinwender, G. et al. Allopurinol Reduces Bacterial Translocation, Intestinal Mucosal Lipid Peroxidation, and Neutrophil-Derived Myeloperoxidase Activity in Chronic Portal Hypertensive and Common Bile Duct-Ligated Growing Rats. Pediatr Res 40, 422–428 (1996). https://doi.org/10.1203/00006450-199609000-00010
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199609000-00010
This article is cited by
-
Bacterial Translocation to Mesenteric Lymph Nodes Increases in Chronic Portal Hypertensive Rats
Digestive Diseases and Sciences (2010)
-
Plasma redox status is impaired in the portacaval shunted rat – the risk of the reduced antioxidant ability
Comparative Hepatology (2008)
-
The role of nuclear factor-kappa B in bacterial translocation in cholestatic rats
Pediatric Surgery International (2006)
-
The Effect of Caffeic Acid Phenethyl Ester on Bacterial Translocation and Intestinal Damage in Cholestatic Rats
Digestive Diseases and Sciences (2006)
-
Tumor Necrosis Factor‐α, Interleukin‐1β and Nitric Oxide: Induction of Liver Megamitochondria in Prehepatic Portal Hypertensive Rats
World Journal of Surgery (2005)