Abstract
Patients with anorexia nervosa (AN) frequently suffer from a mild degree of anemia and from moderate leukopenia on top of their undernourished state and metabolic disarrangements. To evaluate in vitro granulopoiesis and its relationship to cytokine production and undernutrition, we have studied 10 adolescent girls with moderate AN (age range, 13.5-18.0). Study methods included assessment of peripheral blood (PB) granulocyte-macrophage colony-forming cells (GM-CFC) of the patients and age-matched controls, and determination of plasma and conditioned medium (CM) of mononuclear cells levels of IL-1, IL-3, IL-6, granulocyte-macrophage colony-stimulating factor(GM-CSF) and tumor necrosis factor (TNF), all of which may play a role in GM-CFC growth regulation. GM-CFC numbers were significantly lower in AN patients compared with the normal controls (13.09 ± 11.15versus 39.33 ± 26.61 colonies/5 × 105 cells,p < 0.01). No inhibitory effect was found in either plasma or CM of patients with AN. However, when CM were applied to non-recombinant human GM-CSF-stimulated normal bone marrow GM-CFC targets, the number of colonies stimulated by the CM of patients with AN was significantly lower than those stimulated by the CM of the controls (73.5 ± 20.1 versus 113.0 ± 11.6, p < 0.025). GM-CSF concentrations in CM were significantly lower in patients with AN compared with normal controls, but no such differences were found in IL-1, IL-3, IL-6, or TNF concentrations. These results indicate defective in vitro granulopoiesis in AN patients, manifested by a reduction of both GM-CFC and GM-CSF. It has to be determined whether these changes are the result of the basic disease process or are they due to malnutrition.
Similar content being viewed by others
Main
Patients with AN frequently suffer from a mild degree of anemia and from moderate leukopenia(1–3). Despite neutropenia, BM is only rarely hypoplastic. Indeed, an increment in neutrophil counts in response to a hydrocortisone injection suggests a normal BM neutrophil reserve in these patients(4). A wide variety of cytokines have been shown to affect nutritional status(5, 6) as well as to affect the process of hematopoiesis(7). Our present knowledge sustains the notion that IL-3, and to a lesser extent GM-CSF, plays a major role in multipotent hematopoietic stem cell survival, proliferation, and differentiation, whereas erythropoietin, granulocyte-CSF, microphage-CSF, and IL-5 in their proliferation and maturation into their end stage products, erythrocytes, neutrophils, monocytes, and eosinophils, respectively. IL-1, IL-4, and IL-6, are cofactors in these processes as well as being tentative physiologic inhibitors(8).
The aim of the present study was to assess the in vitro growth of GM-CFC as well as the levels and interactions of certain cytokines in PB of subjects suffering from AN to understand the interaction of undernutrition and granulopoiesis.
METHODS
Patients. Ten adolescent girls, previously diagnosed as suffering from AN, were studied before initiating therapy. Patients characteristics and hematologic data are given in Table 1. All patients fulfilled the DSM III criteria for AN(9). Patients' age ranged from 13.5 to 18.0 y, and their history of dieting ranged from 6 to 24 mo; patients lost between 10 and 30% of their previous weight. All of the postmenarcheal patients had secondary amenorrhea, which lasted for 4 to 18 mo. None of the patients had any infection when entering the study. All the patients were admitted to a pediatric ward and treated by a behavioral approach and were seen at least once a week by a psychiatrist. Seven age- and sex-matched healthy controls were used for the study. The study was approved by the Human Subject Review Committee of the Kaplan Hospital and an informed consent was obtained from each patient before the study.
Collection and preparation of PB and BM cells. PB cells were obtained from the patients and age-matched healthy controls. Normal BM samples were obtained after informed consent from hematologically normal patients undergoing open heart surgery. PB and BM were heparinized with 10 U/mL sodium heparin. The low density (<1.077 g/mL) mononuclear fractions were isolated by Ficoll-Hypaque gradient sedimentation (Pharmacia Fine Chemical, Uppsala, Sweden). Separated peripheral MNC were washed with PBS, pH 7.2, and suspended for 24 h in RPMI 1640 medium, supplemented with antibiotics and 10% heat-inactivated FCS (RPMI-FCS).
Assay for GM-CFC. PB MNC were then incubated at 5 × 106/mL for 96 h in Iscove's modified Delbecco's medium with 30% FCS, containing rhGM-CSF (10 ng/mL) before plating, to amplify the number of PB GM-CFC. The MNC were then washed twice in PBS. The PB cells were then plated at 5 × 105/mL in 1 mL of McCoy's 5A modified medium containing 0.3% agar, 30% FCS, and in some experiments 10 ng of rhGM-CSF (specific activity 5 × 106 colony-forming units/mg of protein; Behringwerkeag, Marburg, Germany) was added to the gelling agar in 35-mm plastic Petri dishes. Cultures were incubated for 7 d in an atmosphere of 5% CO2 at 37 °C. Colonies consisting of >50 cells were scored in triplicate cultures. 2-hydroxy-3-napholic acid anilide-chloroacetate esterase(Sigma Chemical Co., St. Louis, MO) was used to stain the granulocytic colonies(10).
Preparation of CM. Low density MNC (5 × 106/mL) from PB were incubated overnight in RPMI. Cell-free CM were harvested after 24 h of incubation.
The effect of patients' plasma and CM on GM-CFC assay. Patients' plasma and CM with and without rhGM-CSF were tested in normal BM GM-CFC assay, as described for the PB GM-CFC assay but with 2 × 105 BM cells/mL of culture.
The effect of anti TNF-α antibody on BM GM-CFC. In some experiments any resident TNF-α in the CM or plasma was neutralized with a MAb (Boehringer Mannheim, Germany) at a concentration sufficient to neutralize 100 ng/mL, before its evaluation in semisolid cultures of normal BM cells, with and without rhGM-CSF.
Assays for IL-1, IL-3, IL-6, and GM-CSF. Serum and CM levels of cytokines, IL-1, IL-3, IL-6, GM-CSF, and TNF, were measured by solid phase ELISA. This assay employs the quantitative “sandwich” enzyme immunoassay technique. A MAb specific for the IL molecule has been precoated onto the polystyrene microtiter plate. Standards and samples are introduced into the wells and the IL present is bound by the immobilized antibody. After washing away any unbound proteins, the second enzyme-linked polyclonal or MAb specific to the IL is added to the wells to “sandwich” the IL immobilized during the first incubation. After a wash to remove any unbound antibody-enzyme reagent, a substrate solution is added to the wells, and color develops in proportion to the amount of IL bound in the initial step. The color development is stopped, and the intensity of the color is measured. A curve is prepared, ploting the OD versus the concentration of given IL in the standard wells. By comparing the OD of the samples to this standard curve, the concentration of the IL in unknown samples is then determined.
Statistical analysis. When colony counts were made for patients with AN versus controls on different days, the two groups were compared by the Friedman rank test, with days serving as blocks. As the distribution of cytokine concentrations was nonnormal, nonparametric tests were used for all comparisons. The Wilcoxon two-sample test was used for comparisons of patients with AN versus controls. The effect of changing experimental conditions, using the same subjects, was tested by the Wilcoxon paired-difference test.
RESULTS
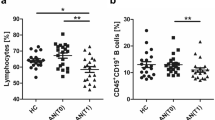
PB GM-CFC colonies of triplicate cultures of 5 × 105 cells were found to be significantly lower in patients with AN compared with their numbers in the normal controls, 13.09 ± 11.15 versus 39.33± 26.61, respectively, colonies/5 × 105 cells (p< 0.01). The addition of plasma of either patients with AN or controls to non-rhGM-CSF stimulated BM GM-CFC assay did not cause any significant change in their numbers (Fig. 1). A significant difference between patients with AN and controls was found when CM were added to non-GM-CSF stimulated BM GM-CFC (73.5 ± 20.1 versus 113.0± 11.6, colonies/2 × 105 cells, p < 0.025)(Fig. 1). No differences were found when the same procedure was repeated in rhGM-CSF-stimulated BM GM-CFC (122.3 ± 15.2versus 137.0 ± 7.1) (Fig. 1).
No differences were found in non-GM-CSF stimulated BM GM-CFC assay of anorectic subjects when TNF-α was neutralized with MAb(Fig. 2).
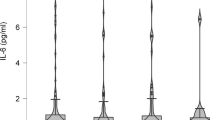
GM-CSF concentrations in PB MNC CM were significantly lower in patients with AN compared with normal controls, but no differences were found in IL-1, IL-3, IL-6, or TNF-α concentrations in either plasma or CM of PB MNC from both patients and controls (Table 2).
DISCUSSION
Our results indicate a significant reduction in the numbers of GM-CFC in peripheral blood of patients with AN, compared with healthy controls. This decrease was not found to be associated with a possible inhibitory factor either in the plasma or in CM from PB MNC cultures of these patients. Apart from this observation, decreased levels of GM-CSF were found in CM of patients with AN compared with healthy controls. No such differences could be identified in other cytokines such as: IL-1, IL-3, IL-6, or TNF. Both results may coincide and suggest a granulopoietic defect in AN, affecting the myeloid progenitors (GM-CFC) and the availability of their regulator (GM-CSF). Although no absolute neutropenia was seen in most of our patients, their white blood cell count was on the lower side as observed by different investigators in the past(1–3).
The reduction in GM-CFC in patients with AN may be caused by two possible mechanisms. On the one hand, a decreased number of progenitor cells at the BM, or inhibition of their release. This in turn may cause a decrease in their absolute numbers in the PB, reflected as reduced PB GM-CFC. On the other hand, reduced PB GM-CFC may be indicative of the presence of defective granulopoietic-committed stem cells in their response to GM-CSF, along with reduced GM-CSF production or secretion by PB MNC. This could be attributed to either the inherent abnormality of these cells, as part of the basic pathology of AN or, more likely, to toxic damage to these cells, secondary to malnutrition and the metabolic abnormalities.
Hypocellular BM in patients with AN has been previously reported by some investigators and was found to be associated with gelatinous transformation to mucopolysaccharides. This was supported by BM biopsies as well as imaging facilities such as magnetic resonance imaging(11) but not with progenitor culture assay. The lack of correlation between the defective in vitro granulopoiesis and the absence of in vivo neutropenia may imply that these patients were not sick enough to cause an overt neutropenia within the wide range of normal leukocyte counts.
Changes in cytokine production in patients with AN have been previously reported(12). We have previously reported increased TNF-α production in CM of PB MNC of patients with AN but not in other chronically undernourished patients(13). In the present study no such increase was found. The difference may be due to either different assay methods or to the relatively better nutritional and metabolic status of our present patients. However, the addition of anti-TNF-α antibodies to AN CM did not cause any increment in their BM GM-CFC stimulation capacity. This further supports the probability that TNF-α did not play a role in the reduced numbers of GM colonies as previously suggested in other clinical situations(14). Recently, a reduced concentration of IL-1 has been shown in malnourished children with kwashiorkor and marasmus(15) and in patients with AN (V. Barak, L. Baider, T. Peretz, S. Stephanos, and A. Kaplan De Nour, unpublished data). These and our findings may on the one hand only be a result of an impaired protein-caloric balance, but, on the other hand, the specific deficiency in IL-1 similar to the isolated deficiency of GM-CSF in our study, may indicate a specific involvement of different cytokines in different nutritional and growth disorders.
We have previously shown that PMN of patients with AN are impaired in several aspects such as superoxide production(16) and cell-mediated cytotoxicity(17). The results of the present study, showing defective granulopoiesis in these patients, complement the assumption that AN is indeed associated with impairment of granulopoietic functions.
Abbreviations
- AN:
-
anorexia nervosa
- GM:
-
granulocyte-macrophage
- CSF:
-
colony-stimulating factor
- CFC:
-
colony-forming cells
- BM:
-
bone marrow
- CM:
-
conditioned medium
- MNC:
-
mononuclear cells
- PB:
-
peripheral blood
- rh:
-
recombinant human
- TNF:
-
tumor necrosis factor
References
Mant MJ, Faragher BS 1972 The haematology of anorexia nervosa. Br J Haematol 23: 737–749
Warren MP, Vande Wiele RL 1973 Clinical and metabolic features of anorexia nervosa. Am J Obstet Gynecol 435: 49
Devuyst O, Lambert M, Rodhain J, Lefebvre C, Coche E 1993 Haematological changes and infectious complications in anorexia nervosa: a case-control study. Q J Med 86: 791–799
Bowers TK, Eckert E 1978 Leukopenia in anorexia nervosa. Lack of increased risk of infection. Arch Intern Med 138: 1520–1523
Grimble KF 1989 Cytokines: their relevance to nutrition. J Clin Nutr 43: 217–230
Hori T, Nakashima T, Take S, Kaizuka Y, Mori T, Katafuchi T 1991 Immune cytokines and regulation of body temperature, food intake and cellular immunity. Brain Res Bull 27: 309–313
Nakayama N, Hatake K, Miyajima A, Arai K, Yokota T 1989 Colony-stimulating factors, cytokines nd hematopoiesis. Cur Opin Immunol 2: 68–77
Olofsson TB 1990 Growth regulation of hematopoietic cells. Acta Oncol 30: 889–902
American Psychiatric Association Task Force on Nomenclature and Statistics: Diagnostic and Statistical Manual of Mental Disorders, Ed. 4, 1995 APA, Washington, DC, pp 539-545
Phillips PG, Chikkappa G, Bunson PS 1983 A triple stain technique to evaluate monocyte, neutrophil and eosinophil proliferation in soft agar cultures. Exp Hematol 11: 10
Vande Berg BC, Malghem J, Devuyst O, Maldague BE, Lambert MJ 1994 Anorexia nervosa: correlation between MR appearance of bone marrow and severity of disease. Radiology 193: 859–864
Bessler H, Karp L, Notti I, Apter A, Tyano S, Djaldetti M, Weizman R 1993 Cytokine production in anorexia nervosa. Clin Neuropharmacol 16: 237–243
Vaisman N, Hahn T 1991 Tumor necrosis factor-α and anorexia-cause or effect? Metabolism 40: 720–723
Broxmeyer HE, Williams DE, Lu L, Cooper S, Anderson SL, Beyer GS, Hoffman R, Rubin BY 1986 The suppressive influence of human tumor necrosis on bone marrow hematopoietic progenitor cells from normal donors and patients with leukemia: synergism of tumor necrosis and interferon. J Immunol 136: 4487
Bhaskaram P, Sivakumar B 1986 Interleukin-1 in malnutrition. Arch Dis Child 61: 182–185
Vaisman N, Tabachnic E, Hahn T, Voet H, Guy N 1992 Superoxide production during refeeding in patients with anorexia nervosa. Metabolism 41: 1097–1099
Vaisman N, Hahn T, Dayan Y, Schattner A 1990 The effect of different nutritional status on cell-mediated cyto-toxicity. Immunol Lett 24: 37–42
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Vaisman, N., Barak, Y., Hahn, T. et al. Defective in Vitro Granulopoiesis in Patients with Anorexia Nervosa. Pediatr Res 40, 108–111 (1996). https://doi.org/10.1203/00006450-199607000-00019
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199607000-00019
This article is cited by
-
Tumour necrosis factor alpha and oxidative stress as maintaining factors in the evolution of anorexia nervosa
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2012)