Abstract
The purpose of this study was to clarify the role of endothelin (ET)-1 in the development of bronchopulmonary dysplasia (BPD). Tracheal aspirates were obtained from 27 newborn babies with respiratory distress (13 with BPD and 14 without BPD) who were mechanically ventilated. Production of superoxide anion(O-2) by rabbit alveolar macrophages was determined by preincubation with the tracheal aspirate supernatant (TAS) and stimulation with phorbol myristate acetate (PMA). O-2 production was demonstrated only when PMA was added to the experimental system and was enhanced with TAS of infants who later developed BPD compared with TAS from infants without BPD. The effects of ET-1 and ET-3 on O-2 production and the blockade by anti-ET-1 antibody and BQ123 (ET A receptor antagonist) were also examined. The enhancing effect was blocked by either anti-ET-1 antibody or BQ123. PMA-stimulated production of O-2 increased when cells were preincubated with several doses of ET-1 (5 × 10-13 to 2 × 10-12 M), whereas ET-3 was without effect. TAS contained significant amounts of immunoreactive ET-1, and there was a close positive correlation (r = 0.764) between the activity of O-2 production and immunoreactive ET-1 levels in TAS samples. These results may be interpreted to indicate that ET-1 synthesized by and secreted from tracheal epithelial cells and/or alveolar macrophages has a priming effect on alveolar macrophages to produce O-2, thus possibly contributing to the development of BPD.
Similar content being viewed by others
Main
Recent observations support the view that parenchymal inflammation of the lung could play a definitive role in the development of BPD(1–5). The predominant inflammatory cells within the alveoli are alveolar macrophages, which modulate inflammatory and immune responses mainly by the reactive oxygen metabolites(6–8). ET-1, a potent endothelium-derived vasoconstrictor peptide, has recently been shown to be implicated in tissue inflammation(9–11). ET-1-LI has been shown to be localized not only in vascular endothelial cells but also in bronchial epithelial cells(12–14). It has been proposed that ET-1 is involved in various bronchopulmonary abnormalities such as bronchial asthma and hypoxic lung injury(15–17). It has recently been demonstrated that ET-1 activates alveolar macrophages through a mechanism involving the arachidonic acid pathway(18). Millul et al.(18) speculated that the transduction pathway coupled to ET-1 receptors seemed to involve the stimulation of phosphatidylinositol diphosphate-specific phospholipase C. This transduction pathway is correlated with the stimulation of NADPH oxidase as well as the stimulation of arachidonic acid. We therefore attempted to demonstrate ET-1 in tracheal aspirates (TAS) from infants with or without BPD and the potential effect of ET-1 on O-2 production by rabbit alveolar macrophages.
METHODS
Compounds. BQ123 (ETA receptor antagonist) was purchased from Banyu Pharmaceutical (Tsukuba, Japan), ET-1, ET-3, and rabbit anti-ET-1 antibody from Peptide Institute Inc. (Osaka, Japan); Hanks balanced salt solution without phenol red from Sigma Chemical Co. (St. Louis, MO); MCLA from Tokyo Kasei (Tokyo, Japan); PMA and SOD of bovine erythrocytes from Wako Chemicals (Osaka, Japan); and Seppak C-18 cartridges from Amersham Int. Plc.(Tokyo, Japan).
Collection of tracheal aspirates. Tracheal aspirates were obtained at 2-4, 6-7, and 12-14 d of age from 27 premature infants who were placed on mechanical ventilation for respiratory distress(Table 1). Seven of the 14 infants who had not developed BPD were excluded from the study at 12-14 d of age because they had already been extubated. Informed consent was obtained from all patients' parents. The diagnosis of BPD was made retrospectively based on radiographic evidence of stage III or stage IV of BPD, requirement of extra oxygen of more than 25%, and respiratory distress at 28 d of age(19). Tracheal aspiration was performed by instillation of 0.5 mL of normal saline. To rinse the aspirates from the side wall of a catheter, 3 mL of saline were aspirated through the catheter into a plastic tube. Aspirates were centrifuged at 1,000× g for 10 min at 4°C, and TAS was frozen at -30°C until analyzed.
Preparation of alveolar macrophages. Alveolar macrophages were collected by bronchoalveolar lavage from Japanese white rabbits as described previously(20). After centrifugation, the cell pellet was resuspended at a final concentration of 4 × 105 cells/mL in Hanks balanced salt solution without phenol red containing antibiotics (100 U/mL penicillin, 100 μg/mL streptomycin). More than 95% of the cells consisted of alveolar macrophages. Viability of alveolar macrophages was more than 99%.
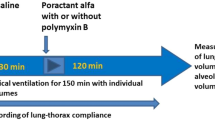
Generation of O-2 by alveolar macrophages. Ten microliters of MCLA (7 μM); 30 μL of TAS, ET-1, or ET-3 (5 × 10-13 to 2 × 10-12 M); and 440 μL of alveolar macrophages (2 × 105) were preincubated for 20 min at 37°C. To study the blocking effects of BQ123 and ET-1 antibody, TAS and alveolar macrophages were similarly preincubated with or without BQ123 (10-10 to 10-9 M), rabbit ET-1 anti-serum, or a nonimmune rabbit serum, followed by the addition of 10 μL of PMA (250 ng/mL) and a further incubation for 30 min at 37°C.
Determination of superoxide anion. MCLA-dependent chemiluminescence was measured with a computerized chemilumimeter (Biolumat LB9505, Berthold Japan K.K., Tokyo)(21). This reaction was suppressed by incubation of cells with SOD (30 U/mL) as would be expected from measurement of superoxide anion production; SOD-uninhibitable counts were subtracted as nonspecific counts. Total luminescence was quantified by integration of the areas under the curves during the experimental time of 30 min. Because there was a significant positive correlation between MCLA-dependent chemiluminescence and cytochrome c reduction, as described by Koga et al.(22) (n = 6, r = 0.992, y = 0.36 + 0.75x), superoxide anion production was calculated by this method.
Extraction of ET-1. ET-1 was extracted from TAS as described previously(23). Briefly, a 2-mL aliquot of TAS was applied to a preactivated SePpak C-18 cartridge. After they were washed with distilled water (10 mL), the materials adsorbed to the column were eluted with 2 mL of 0.1% trifluoroacetic acid/80% methanol, and the extracts were evaporated. The mean recovery of 125I-labeled ET added to TAS was 79.2± 2.5% (n = 5).
Measurement of ET-1. ET-1 was measured by a sandwich-enzyme immunoassay using two different anti-ET antibodies(24). The ET-1 antibodies cross-reacted 100% with ET-1 and 160% with ET-2, but less than 0.18% with ET-3, and 0.16% with big ET- 1. The minimum detectable quantity of ET-1 was 0.2 pg/well. The intra- and interassay coefficients of variance were less than 10%. Content of ET-1 was expressed as picograms/mg of albumin.
Effect of ET-1 on O-2 production. The effect of ET-1 on superoxide anion production by rabbit alveolar macrophages was determined by incubation with various doses of ET-1 followed by stimulation with PMA. To determine whether O-2 production stimulated with TAS involves endogenous ET-1 in the aspirates, experiments using anti-ET-1 antibody and BQ123 were performed (six samples from infants with BPD were used in each experiment). These data were expressed as inhibition (%) of superoxide anion production.
Statistical analysis. Data were expressed as the mean ± SD. Statistical analyses were performed by the two-way analysis of variance and the least significant difference test. A p value less than 0.05 was considered statistically significant.
RESULTS
Addition of ET-1 enhanced O-2 production by rabbit alveolar macrophages in a dose-dependent manner (5 × 10-13 to 2 × 10-12 M) only when PMA was added to the experimental system(Fig. 1), whereas ET-3 failed to enhance O-2 production; the approximate IC50 of ET-1 was 10-12 M. Superoxide anion production in the presence of TAS from infants with BPD was blocked by coincubation with rabbit anti-ET-1 serum, whereas a nonimmune rabbit serum at the same dilutions exerted no effect(Fig. 2). O-2 production stimulated with TAS was blocked by BQ123 (10-10 to 2.5 × 10-9 M)(Fig. 3).
Effect of ET-1 on O-2 production by rabbit alveolar macrophages. Each dose of ET-1 and alveolar macrophages were preincubated for 20 min at 37°C, PMA was added, and doses were further incubated for 30 min. Total MCLA-dependent luminescence was quantified by integration of the areas under the curves during the experimental time of 30 min. ET-specific luminescence was calculated as a total luminescence minus PMA-dependent luminescence. O-2 production was calculated using an index between MCLA-dependent luminescence and cytochrome c reduction. Controls were obtained with nonimmune serum (n = 6, mean± SD).
Normalized ET-1-LI levels in TAS from infants with BPD were significantly higher at 6-7 and 12-14 d of age than those from infants without BPD at corresponding ages (Fig. 4).
A significant difference in ET-1-LI levels was observed between 6-7 and 12-14 d of age at 6-7 and 12-14 d of age. Albumin contents (mg/L) of TAS from infants with and without BPD were as follows: 36 ± 12 versus 53 ± 34 at 2-4 d of age, 49 ± 27 versus 27 ± 13 at 6-7 d of age, and 32 ± 14 versus 24 ± 10 mg/L at 12-14 d of age, respectively.
TAS obtained at 6-7 and 12-14 d of age from infants who later developed BPD yielded significantly greater (p < 0.01) O-2 production by rabbit alveolar macrophages than TAS from infants without BPD(Fig. 5). There was, however, no significant difference at 2-4 d.
There was a significant (p < 0.01) positive correlation(r = 0.764) between O-2 production and ET-1-LI levels in TAS from the infants with or without BPD (Fig. 6).
DISCUSSION
We have demonstrated that the overproduction of both ET-1 and O-2 in the lungs occurs from the early stage of life in infants who later develop BPD, indicating that ET-1 may have a priming effect on alveolar macrophages to form oxygen radicals.
The pathology of BPD originates from the respiratory distress in early life through thickening and fibrosis of the bronchoalveolar walls(2, 3). The major predisposing factor in BPD is the pulmonary immaturity associated with premature birth(4). After an initial insult, injuries by oxidants, proteolytic enzymes, or both may be involved in the development of BPD(25–27). Alveolar macrophages increase from 2 to 45% of total inflammatory cells in intubated preterm infants treated for respiratory distress syndrome(1). Alveolar macrophages function not only as phagocytic cells but also as secretory cells to release various monokines involved in the inflammatory response as well as interaction with lymphocytes(7, 8), among which reactive O-2 metabolites modulate the inflammatory and immune responses. Free oxygen radicals thus produced have been shown to destroy cell membranes by lipid peroxidation(28). It is therefore considered that enhanced O-2 production by alveolar macrophages primed by ET-1 is in part involved in the etiology of BPD.
In this study, O-2 production by rabbit alveolar macrophages stimulated with TAS obtained between 6 and 14 d of age was significantly greater in infants with BPD than that in those without BPD. Superoxide production by TAS obtained from infants at 2-4 d of age was not different between infants with and without BPD. The mechanism of how O-2 production by alveolar macrophages is stimulated with TAS remains to be elucidated, but we observed a significant positive correlation between O-2 production of alveolar macrophages and ET-1 levels of TAS. These results suggest that ET-1 may have a potential effect on the development of BPD.
The present study further showed that rabbit alveolar macrophages would be stimulated by exogenous ET-1 but not by ET-3. We demonstrated that enhanced O-2 production by alveolar macrophages was inhibitable with anti-ET-1 antibody, but not with a control serum. In addition an ETA receptor antagonist (BQ123) completely inhibited O-2 production in alveolar macrophages stimulated with TAS. These results suggest that ET-1 may have a potential effect through an ETA receptor on alveolar macrophages. However, Millul et al.(18) demonstrated that ET-1 increased arachidonic acid production but not oxygen radicals in alveolar macrophages. In this study, O-2 production by alveolar macrophages induced by TAS was enhanced only when PMA was added to the experimental system. From these observations, it was considered that endogenous ET-1 in TAS has a priming effect on alveolar macrophages to generate O-2 mediated via ETA receptor.
The cellular mechanism by which ET-1 activates alveolar macrophages needs to be clarified. It has been reported that ET-1 activates alveolar macrophages by increasing cytosolic calcium levels and protein phosphorylation(30). It seems therefore likely that ET-1 stimulates phosphoinositide breakdown to trigger Ca2+ release in alveolar macrophages via ETA receptors. Alternatively, the finding that normalized ET-1 levels are higher in TAS from infants with BPD appears to indicate that there is a local production of ET-1 in the patients. Oxygen radicals produced by alveolar macrophages may stimulate the overproduction of ET-1 by bronchial epithelial cells and alveolar macrophages. It has been reported that free radicals enhance the release of ET-1 from vascular endothelia and alveolar macrophages(31, 32). Nagase et al.(33) demonstrated that ET may contribute to the inflammatory and hyperreactive process of the lung by enhancing the release of 15-hydroxyeicosatetraenoic acid and oxygen radicals in the distal lung unit. It should be noted that ET-1 production is enhanced in the airway epithelium in patients with symptomatic asthma(34). Thus, the interaction between ET-1 and alveolar macrophages may be present and the macrophage-epithelial cell axis also appears to be important for the pathogenesis of BPD. Taken together, it is presumed that the overproduction of ET-1 accompanied by O-2 production in the lung contributes to the development of BPD.
Abbreviations
- Anti-ET-1 serum:
-
anti-endothelin-1 antibody
- BPD:
-
bronchopulmonary dysplasia
- ET:
-
endothelin
- ETA receptor:
-
endothelin A receptor
- HBSS:
-
Hanks balanced salt solution
- LI:
-
like-immunoreactivity
- MCLA:
-
2-methyl-6-[p-methoxyphenyl]-3,7-dihydroimidazo[1,2-α]pyrazin-3-one
- O-2:
-
superoxide anion
- PMA:
-
phorbol myristate acetate
- SOD:
-
superoxide dismutase
- TAS:
-
tracheal aspirate supernatant
References
Merritt TA, Cochrane CG, Holcomb K, Bohl B, Hallman M, Strayer D, Edwards DK, Gluck L 1983 Elastase andδ1-proteinase inhibitor activity in tracheal aspirates during respiratory distress syndrome. J Clin Invest 72: 656–666
Merritt TA, Stuard ID, Puccia J, Wood B, Edwards DK, Finkelstein J, Shapiro DL 1981 Newborn tracheal aspirate cytology: classification during respiratory distress syndrome and bronchopulmonary dysplasia. J Pediatr 98: 949–956
Jacobson W, Morley CJ, South M 1992 Microscopic observations on tracheal aspirates from ventilated neonates. II. The onset of bronchopulmonary dysplasia and other changes. Eur J Pediatr 151: 204–207
Northway WH Jr 1992 Bronchopulmonary dysplasia: twenty-five years later. Pediatrics 89: 969–973
Heikinheimo M, Halila R, Marttinen E, Raivio K 1992 N-terminal propeptide of type III collagen in tracheal fluid and serum in preterm infants at risk for bronchopulmonary dysplasia. Pediatr Res 31: 340–344
Clement A, Chadelat K, Sardet A, Grimfeld A, Tournier G 1988 Alveolar macrophage status in bronchopulmonary dysplasia. Pediatr Res 23: 470–473
Clement A, Chadelat K, Masliah J, Housset B, Sardet A, Grimfeld A, Tournier G 1987 A controlled study of oxygen metabolite release by alveolar macrophages from children with interstitial lung disease. Am Rev Respir Dis 136: 1424–1428
Davies P 1985 Macrophages as effector cells. Fed Proc 44: 2925–2926
Yanagisawa M, Kurihara H, Kimura S, Tomobe Y, Kobayashi M, Mitsui Y, Yazaki Y, Goto K, Masaki T 1988 A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 332: 411–415
Brown KD, Littlewood CJ 1989 Endothelin stimulates DNA synthesis in Swiss 3T3 cells. Synergy with polypeptide growth factors. Biochem J 263: 977–980
Komuro I, Kurihara H, Sugiyama T, Takaku F, Yazaki Y 1988 Endothelin stimulates c-fos and c-myc expression and proliferation of vascular smooth muscle cells. FEBS Lett 238: 249–252
Koseki C, Imai M, Hirata Y, Yanagisawa M, Masaki T 1989 Autoradiographic distribution in rat tissues of binding sites for endothelin: a neuropeptide?. Am J Physiol 256:R858–R866
Rozengurt N, Springall DR, Polak JM 1990 Localization of endothelin-like immunoreactivity in airway epithelium of rats and mice. J Pathol 160: 5–8
Springall DR, Howarth PH, Counihan H, Djukanovic R, Holgate ST, Polak JM 1991 Endothelin immunoreactivity of airway epithelium in asthmatic patients. Lancet 337: 697–701
Mattoli S, Soloperto M, Marini M, Fasoli A 1991 Levels of endothelin in the bronchoalveolar lavage fluid of patients with symptomatic asthma and reversible airflow obstruction. J Allergy Clin Immunol 88: 376–384
Grunstein MM, Chuang ST, Schramm CM, Pawlowski NA 1991 Role of endothelin 1 in regulating rabbit airway contractility. Am J Physiol 260:L75–L82
Nomura A, Ninomiya H, Saotome M, Ohse H, Ishii Y, Uchida Y, Hirata F, Hasegawa S 1991 Multiple mechanisms of bronchoconstrictive responses to endothelin-1. J Cardiovasc Pharmacol 17( suppl): S213–S215
Millul V, Lagente V, Gillardeaux O, Boichot E, Dugas B, Mencia-Huerta J-M, Bereziat G, Braquet P, Masliah J 1991 Activation of guinea pig alveolar macrophages by endothelin-1. J Cardiovasc Pharmacol 17( suppl 7): S233–S235
Northway WH Jr, Rosan RC, Porter DY 1967 Pulmonary disease following respiratory therapy of hyaline membrane disease: bronchopulmonary dysplasia. N Engl J Med 276: 357–368
Kadiri C, Masliah J, Bachelet M, Vargaftig BB, Bereziat G 1989 Phospholipase A2-mediated release of arachidonic acid in stimulated guinea-pig alveolar macrophages: interaction with lipid mediators and cyclic AMP. J Cell Biochem 40: 157–164
Dahlgren C 1988 Analysis of luminol-dependent chemiluminescence from granule depleted neutrophil cytoplasts reveals two different light-emitting mechanisms. J Biolumin Chemilumin 2: 25–33
Koga S, Nakano M, Tero-Kubota S 1992 Generation of superoxide during the enzymatic action of tyrosinase. Arch Biochem Biophys 292: 570–575
Ando K, Hirata Y, Shichiri M, Emori T, Marumo F 1989 Presence of immunoreactive endothelin in human plasma. FEBS Lett 245: 164–166
Suzuki N, Matsumoto H, Kitada C, Masaki T, Fujino M 1989 A sensitive sandwich-enzyme immunoassay for human endothelin. J Immunol Methods 118: 245–250
O'Brodovich HM, Mellins RB 1985 Bronchopulmonary dysplasia. Am Rev Respir Dis 132: 694–709
Goetzman BW 1986 Understanding bronchopulmonary dysplasia. Am J Dis Child 140: 332–334
Ogden BE, Murphy SA, Saunders GC, Pathak D, Johnson JD 1984 Neonatal lung neutrophils and elastase/proteinase inhibitor imbalance. Am Rev Respir Dis 130: 817–821
Saugstad OD, Hallman M, Abraham JL, Epstein B, Cochrane C, Gluck L. 1984. Hypoxanthine and oxygen induced lung injury: a possible basic mechanism of tissue damage? Pediatr Res 18: 501–504
Johnston RB Jr, Kitagawa S 1985 Molecular basis for the enhanced respiratory burst of activated macrophages. Fed Proc 44: 2927–2932
Haller H, Schaberg T, Lindschau C, Lode H, Distler A 1991 Endothelin increases [Ca++]i, protein phosphorylation, and O-2 production in human alveolar macrophages. Am J Physiol 261:L478–L484
Prasad MR, Jones RM, Kreutzer DL 1991 Release of endothelin from cultured bovine endothelial cells. J Cell Cardiol 23: 655–658
Ehrenreich H, Anderson RW, Fox CH, Rieckmann P, Hoffman GS, Travis WD, Coligan JE, Kehrl JH, Fauci AS 1990 Endothelins, peptides with potent vasoactive properties, are produced by human macrophages. J Exp Med 172: 1741–1748
Nagase T, Fukuchi Y, Jo C, Teramoto S, Uejima Y, Ishida K, Shimizu T, Orimo H 1990 Endothelin-1 stimulates arachidonate 15-lipoxygenase activity and oxygen radical formation in the rat distal lung. Biochem Biophys Res Commun 168: 485–489
Vittori E, Marini M, Fasoli A, De Franchis R, Mattoli S 1992 Increased expression of endothelin in bronchial epithelial cells of asthmatic patients and effect of corticosteroids. Am Rev Respir Dis 146: 1320–1325
Acknowledgements
The authors thank Professor Minoru Nakano of Photon Medical Research Center, School of Medicine, Hamamatsu University, for his advice on chemiluminescence and Takao Souda for his expert analytical assistance.
Author information
Authors and Affiliations
Additional information
Supported in part by the Morinaga Hoshikai and the Mami Mizutani Foundation and Grants-in-Aid for Scientific Research of the Ministry of Culture and the Ministry of Health and Welfare (05454292) and the Ministry of Education, Science and Culture, of Japan.
Rights and permissions
About this article
Cite this article
Kojima, T., Hattori, K., Hirata, Y. et al. Endothelin-1 Has a Priming Effect on Production of Superoxide Anion by Alveolar Macrophages: Its Possible Correlation with Bronchopulmonary Dysplasia. Pediatr Res 39, 112–116 (1996). https://doi.org/10.1203/00006450-199601000-00016
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199601000-00016
This article is cited by
-
Inflammatory Mediators in the Immunobiology of Bronchopulmonary Dysplasia
Clinical Reviews in Allergy & Immunology (2008)