Abstract
Background:
Corresponding with the T helper cell type 1/T helper cell type 2 hypothesis, autoimmune and allergic diseases are considered pathologically distinct and mutually exclusive conditions. Co-occurrence of autoimmune disorders and allergy within patients, however, has been reported. Transgenerational co-occurrence of autoimmune and allergic disease has been less often described and may differ from the intra-patient results.
Aims:
To test the hypothesis that autoimmune disorders in parents are a risk factor for the development of an allergic disease in their offspring.
Methods:
Prospectively registered (by academic general practitioners) International Classifications of Primary Care (ICPC) for diagnoses of autoimmune disorders and allergy within families were evaluated (n=5,604 families) by performing multiple logistic regression analyses.
Results:
The presence of any ICPC-encoded autoimmune disorder in fathers appeared to be associated with an increased risk in their eldest children of developing an allergy (odds ratio (OR) 1.4, 95% CI 1.042 to 1.794). Psoriasis in fathers was particularly shown to be of influence (OR 1.5, 95% CI 1.061 to 2.117) and, although any ICPC-encoded autoimmune disease in mothers was found not to be of significance, the combined international code for registering rheumatoid arthritis/ankylosing spondylitis in mothers was OR 1.7 (95% CI 1.031 to 2.852).
Conclusions:
The occurrence of ICPC-encoded autoimmune disorders in parents, especially psoriasis and rheumatoid arthritis/ankylosing spondylitis, significantly increases the occurrence of allergic disease in their children. After validation in follow-up research in a larger sample, these results may lead to the inclusion of ‘parental autoimmune condition’ as a risk factor in the general practitioner's diagnostics of allergic disease.
Similar content being viewed by others
Introduction
Autoimmune disorders and allergy are chronic immune-mediated diseases characterised by inflammatory responses which, although considered to be distinct clinical immunological conditions, share important epidemiological similarities.1 These similarities seem to imply that autoimmune diseases and allergies share a common aetiology. Some indications for the plausibility of underlying similarities are the rise in prevalence of both these disease groups in the 20th century2,3 and a similar geographical distribution for both allergic and autoimmune disorders (i.e. their incidence increases with the distance from the Equator).3 This finding may be related to the level of development of a country and/or environmental factors. The increase in incidence of autoimmune and allergic disorders in developed countries was shown to stabilise after a period of increase whereas incidence rates continued to rise in most developing countries.4 The incidence of autoimmune disorders and allergic diseases among migrants adapts to that of the corresponding new area, suggesting an involvement of environmental factors.5 Environmental factors reported to be involved in both autoimmune and allergic diseases include breastfeeding,6,7 childhood diet,6 smoking,8 infections,3,8 vitamin D,8,9 and air pollution.10 Such environmental factors may affect phenotypic plasticity through epigenetic mechanisms.11–13 Similar genetic factors associated with autoimmune and allergic disease include the HLA DRB1 allele and polymorphisms in cytokine and Toll-like receptor genes.3,14–18 Monozygotic twins often show dissimilar penetration of autoimmune and allergic diseases, and such observations stress the importance of environmental, epigenetic, and/or genetic factors.3,18,19 Although potentially common underlying mechanisms are currently unknown, interaction between genetics and environment may explain the co-occurrence of autoimmune and allergic diseases.20,21
Importantly, both types of immune disorders are characterised by a detrimental immune response (against self-proteins or proteins from outside the body). Both disease types are characterised by an abundant reactivity of two opposing T helper (Th) cell subsets; a relative abundance of T helper type 1 (Th1) cells occurs in most autoimmune disorders whereas allergic diseases are associated with an abundance of Th2 cells.20,21 Cytokines produced by Th1 and Th2 cells exert reciprocal inhibitory effects, and this has provided mechanistic grounds to view these disorders within patients as being mutually exclusive.21–28 This Th1/Th2 paradigm, however, is at odds with recent findings on the co-existence of autoimmune disorders and allergies, which is more common than expected as shown in epidemiological research.21–24,26–28 However, the prevalence of allergies in patients with rheumatoid arthritis and diabetes mellitus type I compared with controls seems to be decreased. Transgenerational cooccurrence of autoimmune and allergic disease has been less often described and, in most of these studies, no valid measurement of allergic asthma took place.14,29–32 The results of well-designed familial co-occurrence studies may deviate from the intra-patient results.
Taking the common denominators of autoimmune disorders and allergic disease into account, we hypothesised that a parent-child positive relation exists between autoimmune disorders and allergies within families. Such an association, once confirmed, would emphasise the need for a shift in the current theoretical underpinnings that underscore immunological differences rather than similarities in the aetiology of these disease categories. We here report on a prospective epidemiological general practice-based study on the co-occurrence of autoimmune disorders and allergic disease in households.
Methods
Data available for testing the hypothesis consisted of all prospectively registered cases according to the International Classification of Primary Care (ICPC) for allergic and autoimmune disorders by the primary care morbidity registration network (RNH) allied to Maastricht University (August 2008).33 The autoimmune disorders for which an ICPC encoding exists are psoriasis, rheumatoid arthritis/ankylosing spondylitis, ulcerative colitis/Crohn's disease, diabetes mellitus type 1, and multiple sclerosis. Allergic disease ICPC codes are available for allergic asthma, hay fever, atopic dermatitis, and atopic conjunctivitis. This spectrum of autoimmune disorders or allergic diseases will now be referred to as ‘any autoimmune disorder’ or ‘any allergic disease’. ICPC encodings are given only by RNH physicians if the diagnosis was either supported by laboratory tests or if a medical specialist reported on it to the general practitioner. Data concerning households with two adults of opposing gender and at least one child aged ≥6 years were used, as only at this age can all allergic diagnoses be verified by diagnostic tests. The exact inclusion criteria for family relations and the results of a pilot study on the validation of these inclusion criteria are described in Appendix 1, available online at www.thepcrj.org.
Rheumatoid diseases represent a large number of patients diagnosed with an autoimmune disease, but no exclusive ICPC encoding for rheumatoid arthritis or ankylosing spondylitis exists. The ICPC code L88 represents both rheumatoid arthritis and ankylosing spondylitis. Considering its importance, a pilot study was carried out on the association of rheumatoid arthritis or ankylosing spondylitis in patients and allergic disease in their offspring at the Departments of Rheumatology at the Maastricht University Medical Centre, Maastricht and the Atrium Medical Centre, Heerlen. Information on this pilot study is described in Appendix 1, available online at www.thepcrj.org.
Statistics
The Statistical Package of Social Sciences (SPSS) Version 15.0 and Statistical Analysis Software (SAS) were used. Data used for answering the research questions were provided by the regional network of general practices associated with Maastricht University. Missing data in any of the variables necessary for the statistical analyses formed an exclusion criterion.
First, the statistical correlation between any autoimmune disorder in separate parents and the occurrence of any allergic disease in their offspring was evaluated (χ2 test). Second, tests for answering the main research question on the effect of any parental autoimmune disorder as registered by general practitioners on the allergic status of their children were conducted with multiple logistic regression models including any allergy in the children, allergic asthma, hay fever, and atopic dermatitis as the dependent variables. The independent variables ‘any autoimmune disorder’ in fathers and mothers separately, ‘any allergic disease’ in the fathers and mothers, respectively, ‘any autoimmune disorder’ in the children, children's age and gender were included in the analyses. For answering the second research question on the influence of specific autoimmune disorders in parents on the occurrence of allergy in their children, the variables representing ‘specific ICPC encoded autoimmune disorders’, instead of ‘any autoimmune disorder’ in the separate parents, were tested
For model fitting, two cases were differentiated: ‘one child only’ multiple logistic regression analysis versus ‘nested, siblings’ analyses, with an additional random effect (intercept). In the former case all available families were included in the analysis, which was conducted with either their eldest or only child; in the latter case, analysis was restricted to those families with more than one child. For models with random effects, logistic intraclass correlations (ICCs) are reported to express the degree of similarity among siblings within the same family (ICCs larger than zero indicate strong heterogeneity among families which could not be attributed to the measured sources of variation). More information on the statistical methodology used is provided in Appendix 1, available online at www.thepcrj.org.
Results
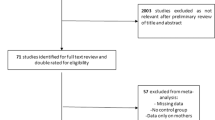
A dataset of 10,575 households resulted from the selection of families including at least one child. Because variables on both the father and the mother were assumed to be of influence and only families containing at least one child aged ≥6 years were included, only 5,604 families could be used in the analyses.
Children
A total of 9,904 children were included, comprising 5,604 eldest children and 4,300 younger siblings. Allergic disease in the eldest children was used as the primary outcome of the analyses. Data on allergic disease, any autoimmune diagnosis, age, and gender of all children included are presented in Table 1. Any allergic disease was diagnosed in 20% of the children included and autoimmune disorders were diagnosed in 1.5% of the children.
Parents
Information on the occurrence of specific autoimmune or allergic diseases (number and prevalence) in the separate parents, as included in both datasets, is presented in Table 2. Any allergic disease was diagnosed in 13–15% of parents whereas any autoimmune disorder was diagnosed in 5% of the parents. Psoriasis was the autoimmune disorder most often diagnosed in the parents followed by rheumatoid arthritis/ankylosing spondylitis. The occurrence of any autoimmune disorder and/or any allergic disease in parents, separately or both, and the corresponding occurrence of any allergic disease in the eldest children not corrected for additional possible confounding factors (χ2 analysis) are shown in Table 3.
Any allergic disease in offspring
The results of the logistic regression analyses on the association of any autoimmune condition in the parents and at least one ICPC-encoded allergic disease in their offspring are presented in Table 4. The results corrected for age and gender of the children, occurrence of allergic disease in the parents, and autoimmune status of mothers, fathers and children confirmed the χ2 outcome presented in Table 3. Allergy in the parents had the most evident effect on the development of allergic disease(s) in their eldest children. With respect to the original research question concerning intrafamilial co-occurrence of autoimmune and allergic disease, a significant positive effect was found for autoimmune disorders in fathers on the occurrence of any allergic disease in the children (eldest: OR 1.4, nested siblings: OR 1.4). The occurrence of autoimmune disorders in the mother did not seem to influence allergy development in the children. Male gender was shown to increase the chance of a child being diagnosed with any allergic disease. Registered autoimmune disorders in the children did not appear to have a statistically significant effect on the occurrence of any allergic disease; this variable was therefore excluded from the analysis.
Specific allergic diseases
In both the first child analysis and the analysis of siblings, rheumatoid arthritis/ankylosing spondylitis in the mothers was found to be associated with the respiratory allergies evaluated (asthma: first children OR 1.952; hay fever: first children OR 2.148, siblings OR 2.485). Psoriasis in the fathers did seem to be associated with the occurrence of atopic dermatitis in their first children only (OR 1.597).
All outcomes
The cohesiveness of the allergic outcome within families, expressed as the ICC, varied from 0.19 to 0.32.
Discussion
Main findings
Based on prospectively collected data as registered by general practitioners, we present evidence for a positive significant correlation between the diagnosis of parental autoimmune disorders and the risk of their children developing an allergic disease. The specific diagnosis of rheumatoid arthritis/ankylosing spondylitis in mothers and psoriasis in fathers appeared to be associated with an increased chance of developing an allergic disease in their children.
Strengths and limitations of this study
One strength of our study is that diagnoses of autoimmune disorders and allergic disease were used instead of laboratory outcomes. For the majority of autoimmune disorders in our dataset, no diagnostic autoantibodies are available. The use of autoantibody testing, if relevant for the type of disease suspected, is part of the diagnostic process (e.g. in rheumatoid arthritis). The results of these tests were not available for the researchers.
Families included in the study were selected based on the composition of the households (both parents living together, only children living at home, age of children ≥6 years) and therefore may not be representative of the total Dutch population. Most immune-mediated diseases in parents and children, however, did not deviate from the figures presented in the National Compass of Public Health or from the regional general practice morbidity registration, indicating no significant differences from the total Dutch population.34,35
Despite the fact that biological kinship was not always fully clear, validation of the selected families (n=595 households) by their general practitioners revealed that 89.4% of the parents and children selected were biologically related. In 10% of the families one of the adults (6% mothers, 4% fathers) was confirmed as a biological parent. In this respect, our dataset does not substantially deviate from a dataset encompassing ‘fully known biologic kinship’ and is therefore not expected to substantially affect the outcome.
Despite significant associations, a large proportion of variability in the probability of occurrence of any outcome was attributable to the random effect (ICC >20%). This means that there was still great variation among families that could not be explained by the measured factors.
The results of a pilot study on the influence of either rheumatoid arthritis or ankylosing spondylitis in parents, carried out to be able to distinguish between the two types of rheumatic disease clustered in the ICPC encoding available, indicate that the prevalence of a specific allergic disease in the offspring of parents with either rheumatoid arthritis (allergic asthma 17.5%, hay fever 39.4%) or ankylosing spondylitis (hay fever 23%, atopic dermatitis 25%) was higher than the reported prevalence known to be associated with the general Dutch population (allergic asthma 7–11%, hay fever 3–4%, atopic dermatitis 9–14%).36 Over-reporting of allergic diagnoses in children of parents participating in the pilot study, however, did not explain the higher incidence, as not all of the allergic diagnoses reported in their offspring were higher in prevalence compared with the general population. The occurrence of atopic dermatitis in children of parents with rheumatoid arthritis (9.0%) and allergic asthma in children of parents with ankylosing spondylitis (5.6%) were similar to the reported prevalence in the general Dutch population.36 Combined with our current analysis, we therefore deduce from these observations that rheumatoid arthritis in parents is specifically associated with a significant increase in the occurrence of (respiratory) allergic disease in their children. Findings that support this deduction include: (1) the lower prevalence of ankylosing spondylitis as opposed to rheumatoid arthritis in the Netherlands (0.1–0.4% vs. 1–2%);34,37–40 (2) the even lower occurrence in women (0.03–0.13%);37 and (3) the lack of influence of rheumatoid arthritis/ankylosing spondylitis in fathers on the occurrence of allergic disease in their eldest children in the analysis carried out.
Implications for future research, policy and practice
The results of the current study seem to indicate an intrafamilial association between autoimmune disorders — especially psoriasis, rheumatoid arthritis, and/or ankylosing spondylitis — and allergic disease.
An explanation for the higher occurrence of allergic disease in offspring, particularly of mothers diagnosed with rheumatoid arthritis, may indicate an association with female-specific influences. For instance, it may be that females diagnosed with rheumatoid arthritis more often choose not to breastfeed their children. Breast feeding is known to have a preventive effect on the development of both types of immune-mediated disease in children, but seems to be associated with an increased severity of rheumatoid arthritis in the mother who may therefore be advised against it.40
As in other studies researching the possible association between autoimmune disorders and allergic disease, environmental factors were not corrected for in this study. Follow-up research in larger cohorts is important to validate these novel findings — including a detailed documentation of relevant environmental factors — to address a possible role for epigenetic mechanisms in the relationship between immune-mediated disorders across generations.
In the current Dutch standards for general practitioners, an enhanced risk for the occurrence of (respiratory) allergy in children of autoimmune patients is not included in the protocol. If the results of a follow-up project validate the findings presented here, this may lead to the inclusion of the risk factor ‘autoimmune disorder in parent’ in the general practitioners' standards for allergic disease.
The dataset used in the current study was too small to estimate reliably the effect of parental diabetes mellitus type 1 or multiple sclerosis on the occurrence of allergic disease in their children. Similar limitations prevented the statistical analysis of possible relationships between autoimmune diseases in parents and conjunctivitis in their children.
Interpretation of findings in relation to previously published work
We report here on a parent-child relationship between autoimmune disorders and allergic disease. This, together with the previously described epidemiological findings on the co-occurrence of these types of disease within patients21,24,26,27 and among family members,14,29–32 supports the notion that autoimmune diseases and allergies can co-exist, in contrast to the currently held theoretical supposition that autoimmune disorders and allergies exclude one another.
A familial association of rheumatoid arthritis in patients and asthma in a parent or sibling has been previously reported, although no distinction was made between allergic asthma and non-allergic asthma.29
To our knowledge, specific data on the co-occurrence of autoimmune disorders in patients and allergic disease in their offspring has not previously been described. However, a number of studies contradict the epidemiological co-occurrence of autoimmune and allergic diseases within patients — for example, the EURODIAB project (diabetes mellitus type 1, OR 0.8, 95% CI 0.64 to 0.97) and the study by Rudwaleit et al. (rheumatoid arthritis, OR 0.6 (95% CI 0.41 to 0.81).25,23 This difference in study outcome may be related to the type of co-occurrence (i.e. within patients vs. transgenerational). Another explanation for the significant effects of psoriasis and rheumatoid arthritis/ankylosing spondylitis in parents on the prevalence of allergies in their children may be that the parental diagnoses were skewed for these autoimmune disorders because of their sheer prevalence; this could indicate that not only these specific autoimmune disorders but any autoimmune disorder in the parents is of interest. As only rheumatic diseases, inflammatory bowel diseases, and psoriasis have been shown to occur sufficiently often to be able to gain statistical significance, this assumption cannot be proven using the current dataset. The lack of data on the whole spectrum of autoimmune disorders and allergies may have influenced the current results and conclusions. The autoimmune disorders tested in our study, however, are a starting point for further research on possible relations between autoimmune disorders and allergy.
Somewhat surprisingly, the occurrence of (any) autoimmune disorder in the children (1.7%) did not affect the outcome. This unexpected outcome may be explained in part by the relatively low age (median 18.0 years) of the children in this study; according to the age-specific prevalence data for the Netherlands, most autoimmune disorders are known to develop at later ages.34
Allergies and autoimmune disorders are known to involve similar genetic and environmental factors.3,8,15,17 A growing number of studies report parent-of-origin dependent effects on the development of disease in offspring. These observations stress the possibility that environmental factors and epigenetic mechanisms, besides genetics, may be involved in transgenerational effects.41–44 The possible influence of a reluctance to breast feed children by patients with rheumatoid arthritis40 has been described earlier. Although genetics may contribute to the parent-of-origin effects observed in this study, the altered phenotypic expression (i.e. autoimmune disease vs. allergy) suggests an involvement of the (micro)environment during gametogenesis, embryogenesis, and/or postnatal development.45 However, in our data these genetics and epigenetics are not distinguished. Access to information on environmental factors that have been aetiologically associated with the occurrence of immune-mediated diseases would have facilitated a more precise demarcation of these two distinct sources of variation.
Conclusions
The research presented here was primarily focused on establishing a transgenerational relationship between autoimmune and (respiratory) allergic diseases. The results indicate that the presence of an autoimmune disorder in one or both parents generates a risk factor for allergic disease in their children. Autoimmune disorders in the father — specifically psoriasis — appear to represent a risk factor for the development of allergic disease (atopic dermatitis), while rheumatoid arthritis in mothers significantly affected the respiratory allergies asthma and hay fever as an outcome in their offspring. Our findings warrant further research into the common denominators in the pathogenesis of the whole spectrum of allergic disease and autoimmune disorders.
References
Ehlers S, Kaufmann SH . Infection, inflammation, and chronic diseases: consequences of a modern lifestyle. Trends Immunol 2010;31:184–90. http://dx.doi.org/10.1016/j.it.2010.02.003
Green A, Patterson CC . Trends in the incidence of childhood-onset diabetes in Europe 1989–1998. Diabetologia 2001;44(Suppl 3):B3–8. http://dx.doi.org/10.1007/PL00002950
Bach JF . The effect of infections on susceptibility to autoimmune and allergic diseases. N Engl J Med 2002;347:911–20. http://dx.doi.org/10.1056/NEJMra020100
Baumgart DC, Carding SR . Inflammatory bowel disease: cause and immunobiology. Lancet 2007;369:1627–40. http://dx.doi.org/10.1016/S0140-6736(07)60750-8
Eldeirawi K, McConnell R, Furner S, et al. Associations of doctor-diagnosed asthma with immigration status, age at immigration, and length of residence in the United States in a sample of Mexican American School Children in Chicago. J Asthma 2009;46:796–802.
Gearry RB, Richardson AK, Frampton CM, Dodgshun AJ, Barclay ML . Population-based cases control study of inflammatory bowel disease risk factors. J Gastroenterol Hepatol 2010;25:325–33. http://dx.doi.org/10.1111/j.1440-1746.2009.06140.x
Saarinen UM, Kajosaari M . Breastfeeding as prophylaxis against atopic disease: prospective follow-up study until 17 years old [see comments]. Lancet 1995;346:1065–9. http://dx.doi.org/10.1016/S0140-6736(95)91742-X
Myasoedova E, Crowson CS, Kremers HM, Therneau TM, Gabriel SE . Is the incidence of rheumatoid arthritis rising?: Results from Olmsted County, Minnesota, 1955–2007. Arthritis Rheum 2010;62:1576–82. http://dx.doi.org/10.1002/art.27425
Weiss ST, Litonjua AA . Maternal diet vs lack of exposure to sunlight as the cause of the epidemic of asthma, allergies and other autoimmune diseases. Thorax 2007;62:746–8. http://dx.doi.org/10.1136/thx.2007.079707
Gehring U, Wijga AH, Brauer M, et al. Traffic-related air pollution and the development of asthma and allergies during the first 8 years of life. Am J Respir Crit Care Med 2010;181:596–603. http://dx.doi.org/10.1164/rccm.200906-0858OC
Lumey LH, Stein AD . In utero exposure to famine and subsequent fertility: The Dutch Famine Birth Cohort Study. Am J Public Health 1997;87:1962–6. http://dx.doi.org/10.2105/AJPH.87.12.1962
Lumey LH, Stein AD . Offspring birth weights after maternal intrauterine undernutrition: a comparison within sibships. Am J Epidemiol 1997;146:810–19. http://dx.doi.org/10.1093/oxfordjournals.aje.a009198
Pembrey ME, Bygren LO, Kaati G, et al. Sex-specific, male-line transgenerational responses in humans. Eur J Hum Genet 2006;14:159–66. http://dx.doi.org/10.1038/sj.ejhg.5201538
Hemminki K, Li X, Sundquist J, Sundquist K . Familial association between type 1 diabetes and other autoimmune and related diseases. Diabetologia 2009;52:1820–8. http://dx.doi.org/10.1007/s00125-009-1427-3
Yang IA, Savarimuthu S, Kim ST, Holloway JW, Bell SC, Fong KM . Gene-environmental interaction in asthma. Curr Opin Allergy Clin Immunol 2007;7:75–82 http://dx.doi.org/10.1097/ACI.0b013e328012ce39.
McLeish S, Turner SW . Gene-environment interactions in asthma. Arch Dis Child 2007;92:1032–5. http://dx.doi.org/10.1136/adc.2006.112185
Mohan C . Environment versus genetics in autoimmunity: a geneticist's perspective. Lupus 2006;15:791–3. http://dx.doi.org/10.1177/0961203306070005
Bartunkova J, Kayserova J, Shoenfeld Y . Allergy and autoimmunity: parallels and dissimilarity: the yin and yang of immunopathology. Autoimmun Rev 2009;8:302–08. http://dx.doi.org/10.1016/j.autrev.2008.09.004
Ho SM . Environmental epigenetics of asthma: an update. J Allergy Clin Immunol 2010;126:453–65. http://dx.doi.org/10.1016/j.jaci.2010.07.030
Mossman TR, Cherwinsky MW, Bond MW, Giedlin MA, Coffman RL . Two types of murine helper T cell clones. I. Definition according to profiles of lymfokines activities and secreted properties. J Immunol 1986;136:2348–57.
Dales R, Chen Y, Lin M, Karsh J . The association between allergy and diabetes in the Canadian population: implications for the Th1-Th2 hypothesis. Eur J Epidemiol 2005;20:713–7. http://dx.doi.org/10.1007/s10654-005-7920-1
van Roon JA, Bijlsma JW . Th2 mediated regulation in RA and the spondyloarthropathies. Ann Rheum Dis 2002;61:951–4. http://dx.doi.org/10.1136/ard.61.11.951
Rudwaleit M, Andermann B, Alten R, et al. Atopic disorders in ankylosing spondylitis and rheumatoid arthritis. Ann Rheum Dis 2002;61:968–74. http://dx.doi.org/10.1136/ard.61.11.968
Simpson CR, Anderson WJ, Helms PJ, et al. Coincidence of immune-mediated diseases driven by Th1 and Th2 subsets suggests a common aetiology. A population-based study using computerized general practice data. Clin Exp Allergy 2002;32:37–42. http://dx.doi.org/10.1046/j.0022-0477.2001.01250.x
EURODIAB. Decreased prevalence of atopic diseases in children with diabetes. The EURODIAB Substudy 2 Study Group. J Pediatr 2000;137:470–4. http://dx.doi.org/10.1067/mpd.2000.109109
Kero J, Gissler M, Hemminki E, Isolauri E . Could TH1 and TH2 diseases coexist? Evaluation of asthma incidence in children with coeliac disease, type 1 diabetes, or rheumatoid arthritis: a register study. J Allergy Clin Immunol 2001;108:781–3. http://dx.doi.org/10.1067/mai.2001.119557
Sheikh A, Smeeth L, Hubbard R . There is no evidence of an inverse relationship between TH2-mediated atopy and TH1-mediated autoimmune disorders: Lack of support for the hygiene hypothesis. J Allergy Clin Immunol 2003;111:131–5. http://dx.doi.org/10.1067/mai.2003.8
Martino DJ, Prescott SL . Silent mysteries: epigenetic paradigms could hold the key to conquering the epidemic of allergy and immune disease. Allergy 2010;65:7–15. http://dx.doi.org/10.1111/j.1398-9995.2009.02186.x
Hemminki K, Li X, Sundquist J, Sundquist K . Familial associations of rheumatoid arthritis with autoimmune diseases and related conditions. Arthritis Rheum 2009;60:661–8. http://dx.doi.org/10.1002/art.24328
Sipetic S, Vlajinac H, Kocev N, Marinkovic J, Radmanovic S, Denic L . Family history and risk of type 1 diabetes mellitus. Acta Diabetol 2002;39:111–15. http://dx.doi.org/10.1007/s005920200028
D'Arienzo A, Manguso F, Astarita C, et al. Allergy and mucosal eosinophil infiltrate in ulcerative colitis. Scand J Gastroenterol 2000;35:624–31. http://dx.doi.org/10.1080/003655200750023598
Hemminki K, Li X, Sundquist K, Sundquist J . Familial association of inflammatory bowel diseases with other autoimmune and related diseases. Am J Gastroenterol 2010;105:139–47. http://dx.doi.org/10.1038/ajg.2009.496
Metsemakers JF, Hoppener P, Knottnerus JA, Kocken RJ, Limonard CB . Computerized health information in The Netherlands: a registration network of family practices. Br J Gen Pract 1992;42:102–06.
RIVM. Nationaal Kompas Volksgezondheid. 2011.
vandenAkker M, Metsemakers JFM, Limonard CBG, Knottnerus JA . General practice, a goldmine for research. Maastricht, 2004
Wijga AH, Beckers MC . [Complaints and illnesses in children in the Netherlands]. Ned Tijdschr Geneeskd 2011;155:A3464.
van der Linden S, Valkenburg HA, Cats A . Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum 1984;27:361–8. http://dx.doi.org/10.1002/art.1780270401
Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988;31:315–24.
(Reumafonds) AaMA. Ankylosing spondylitis. 2012. www.reumafonds.nl. http://dx.doi.org/10.1002/art.1780310302
Jorgensen C, Picot MC, Bologna C, Sany J . Oral contraception, parity, breast feeding, and severity of rheumatoid arthritis. Ann Rheum Dis 1996;55:94–8. http://dx.doi.org/10.1136/ard.55.2.94
Daxinger L, Whitelaw E . Understanding transgenerational epigenetic inheritance via the gametes in mammals. Nat Rev Genet 2012;13:153–62.
Feinberg AP . Phenotypic plasticity and the epigenetics of human disease. Nature 2007;447:433–40. http://dx.doi.org/10.1038/nature05919
Iwasaki M, Tsugane S . Risk factors for breast cancer: epidemiological evidence from Japanese studies. Cancer Sci 2011;102:1607–14. http://dx.doi.org/10.1111/j.1349-7006.2011.01996.x
Koppelman GH, Nawijn MC . Recent advances in the epigenetics and genomics of asthma. Curr Opin Allergy Clin Immunol 2011;11:414–19. http://dx.doi.org/10.1097/ACI.0b013e32834a9573
Kaati G, Bygren LO, Pembrey M, Sjostrom M . Transgenerational response to nutrition, early life circumstances and longevity. Eur J Hum Genet 2007;15:784–90. http://dx.doi.org/10.1038/sj.ejhg.5201832
Acknowledgements
Handling editor Mohammed Osman Yusuf
Statistical review Gopal Netuveli
We acknowledge the general practitioners of the research network allied to Maastricht University (RNH) for the prospective registration of all ICPC encodings regarding allergic and autoimmune disorders and for supplying those to us for research purposes. We thank all patients co-operating in the pilot research carried out in the preparation of the current manuscript for their kindness in giving relevant family health information and help in gaining more information on the difference in the association of rheumatoid arthritis and ankylosing spondylitis with allergic disease in their offspring.
Funding No funding was necessary for the research reported.
Author information
Authors and Affiliations
Contributions
The authors were all involved in writing the paper. AJ Knottnerus and T Maas were involved in designing the study. V Limapassos and T Maas carried out the statistical analyses.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflicts of interest in relation to this article.
Appendix 1. Transgenerational occurrence of allergic disease and autoimmunity. General practice based epidemiologic research
Appendix 1. Transgenerational occurrence of allergic disease and autoimmunity. General practice based epidemiologic research
A) Criteria for households to be included in the dataset of the current article and results of their validation
Introduction pilot: As general practitioners in The Netherlands do not encode family relations in their data, only information on presumable families (people living together in a household) could be used for answering the research question if autoimmune disease in patients does increase the occurrence of allergic disease in their children. To be eligible for inclusion in our dataset, the household should consist of 2 adults of different gender and minimally one child aged at least 6 years. The children living in the households selected were considered to be the offspring of the assumed parents if they differed at least 15 years in age from the adults but no more than 45 years from the suspected mother. If there were several children in a household that differed at least ten months in age, apart from twins, these children were assumed to be siblings.
Methods pilot: The inclusion criteria for family relations were validated in a subgroup of households (9.5%). This subgroup of households was evenly distributed over the general practices supplying the data. The general practitioners supplied their information if the parents and children in the households selected from their practice were biologically related (n±80 / practice).
Results of the pilot: The validation of the parent-child relationship in a subgroup of n=595 households, evenly distributed over the geographical area in which the general practices were situated, showed that in 89.4% of the households (n=528) both adults and children had a biologic relation. Ten percent of the children was related to one of the parents selected and of approximately 1% of the children biological relationship to any of the adults could be established.
Discussion pilot: Despite the fact that biological kinship was not always fully clear, validation of the selected families (n=595 households) by their general practitioners revealed that 89.4% of the parents and children selected were biologically related. In 10% of the families one of the adults (6% mothers, 4% fathers) was confirmed as a biological parent. In this respect, our dataset does not substantially deviate from a dataset encompassing fully known biologic kinship and is therefore not expected to affect outcome.
B) Pilot study on the association of rheumatoid arthritis and ankylosing spondylitis in patients and allergic disease in their children
Introduction: Rheumatoid diseases represent a large amount of patients diagnosed with an autoimmune disease but no exclusive ICPC encoding for rheumatoid arthritis or ankylosing spondylitis exists. Although these diseases have different pathology both the diagnoses rheumatoid arthritis and ankylosing spondylitis in patients are included in the ICPC code L88.
Methods (pilot study): Considering its relevance, a pilot study was carried out on the association of rheumatoid arthritis or ankylosing spondylitis specifically in patients and allergic disease in their offspring at the departments of rheumatology at the Maastricht University Medical Centre, Maastricht and the Atrium Medical Centre, Heerlen.
Consecutively, forty patients with rheumatoid arthritis and 36 patients with ankylosing spondylitis according to the modified New York criteria were interviewed by their rheumatologist, during their planned visit, on the occurrence of doctor's diagnosed allergic asthma, hay fever and/or atopic dermatitis in their eldest children from July till December 2011.33,34 Validated questions, as used in the International Asthma and Allergy Childhood study (ISAAC) were used for differentiation between the association between both rheumatoid arthritis and ankylosing spondylitis in patients and the occurrence of allergic disease in their offspring.
Results (pilot study): Pilot analysis on the occurrence of any allergic disease in the children of rheumatoid arthritis patients and those diagnosed with ankylosing spondylitis showed that allergy is diagnosed at equal frequency in their first born children. The specific allergic diseases, however, differed; allergic asthma (OR 15.3, 95% CI 1.430, 164.148) and/or hay fever (OR 4.3, 95% CI 1.114, 16.289) were significantly more prevalent in first born children of rheumatoid arthritis patients as compared to children of ankylosing spondylitis patients.
Discussion: The pilot results on the influence of either rheumatoid arthritis or ankylosing spondylitis in parents, carried out to be able to distinguish between both types of rheumatic disease as clustered in the ICPC encoding available, indicate that the specific allergic disease prevalence of offspring from both rheumatoid arthritis patients (allergic asthma 17.5%, hay fever 39.4%) and ankylosing spondylitis patients (hay fever 23%, atopic dermatitis 25%) was higher than the reported prevalence known to be associated with the general Dutch population (allergic asthma 7–11%, hay fever 34%, atopic dermatitis 9–14%).33 Over-reporting of allergic diagnoses in children of parents participating in the pilot study, however, did not explain the higher incidence, as not all of the allergic diagnoses reported in their offspring were higher in prevalence compared to the general population. The occurrence of atopic dermatitis in children of rheumatoid arthritis patients (9.0%) and allergic asthma in children of ankylosing spondylitis patients (5.6%), were similar to the reported prevalence in the general Dutch population.33 Combined with our current analysis, we therefore deduce from these observations that rheumatoid arthritis is specifically associated with a significant increase in the occurrence of respiratory allergic disease in their eldest children.
Findings that support this deduction include 1) the lower prevalence of ankylosing spondylitis as opposed to rheumatoid arthritis in the Netherlands (0.1 to 0.4 vs. 1–2%)34–37 2) the even lower occurrence in women (0.03 to 0.13%)35 3) the lack of influence of rheumatoid arthritis/ankylosing spondylitis in fathers on the occurrence of allergic disease in their eldest children in the analysis carried out.
C) Statistics
The statistical package of the social sciences (SPSS) version 15.0 and statistical analysis software (SAS) were used.
Tests for the effect of parental autoimmune disorders on the allergic status of their children were conducted with multiple logistic regression models. For model fitting, two cases were differentiated: ‘one child only’ multiple logistic regression analyses vs. ‘nested, siblings’ analyses. In the former case all available families were included in the analysis, which was conducted with either their eldest or only child; in the latter case, analysis was restricted to those families with more than one child.
To account for the nesting of children within families, a random intercept logistic model was fitted, with families being the first-level random factor. In this nested (all siblings within a family) data analysis, heterogeneity across families is captured by the random intercept variance, which accounts also for the correlation between siblings from the same family. This correlation arises from the fact that the siblings share family-specific but unobserved properties.
In the logistic regression analyses the variables that were included were the dependent variables any allergic disease in the children or the separate specific allergic disorders allergic asthma, hay fever or atopic dermatitis and the independent variables any autoimmune disorder in fathers and mothers separately or the specific autoimmune conditions rheumatoid arthritis/ankylosing spondylitis, psoriasis, inflammatory bowel diseases, any allergic disease in the separate parents, any autoimmune disorder in the children, the children's age and gender.
In all analyses variable selection was handled via the top down procedure (likelihood ratio tests), except for the mandatory variables age and sex of a child, any allergic disease in mothers and fathers separately. These were kept in the models irrespective of their statistical significance.
It should be noted that a nested model analysis with all available data (involving both one and more than one child families) was also performed. The results are omitted, to avoid redundancy (as they were similar to the ones presented). The reason for selecting the 2 steps approach, despite the potential for introducing bias in the process of dividing the target population, was more statistical than methodological. One-child families do not provide any information for the estimation of the variance of the occurrence of allergic disease between children within families (the ‘nesting parameter’, the random intercept variance). Besides, model convergence was considerably delayed.
Rights and permissions
About this article
Cite this article
Maas, T., Nieuwhof, C., Passos, V. et al. Transgenerational occurrence of allergic disease and autoimmunity: general practice-based epidemiological research. Prim Care Respir J 23, 14–21 (2014). https://doi.org/10.4104/pcrj.2013.00108
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.4104/pcrj.2013.00108
This article is cited by
-
Association between parental autoimmune disease and childhood atopic dermatitis varied by sex: a nationwide case–control study
Archives of Dermatological Research (2023)
-
The uni-directional association of atopic dermatitis and rheumatoid arthritis: a systematic review and meta-analysis
Archives of Dermatological Research (2023)
-
Atopy in children with the enthesitis-related arthritis (ERA) subtype of juvenile idiopathic arthritis is associated with a worse outcome
European Journal of Pediatrics (2015)