Abstract
BACKGROUND:
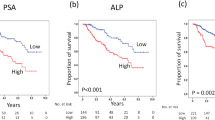
Selecting appropriate candidates for postprostatectomy radiotherapy is challenging, because adverse pathological features cannot accurately predict clinical recurrence. Biomarkers that identify residual disease activity may assist clinicians when counseling patients on the risks, benefits and costs of secondary treatment. NADiA ProsVue PSA slope results ⩽2.0 pg ml−1 month−1 are predictive of a reduced risk of clinical recurrence; however, its clinical utility has not yet been studied.
METHODS:
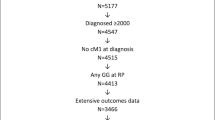
We prospectively enrolled men treated by radical prostatectomy in a multicenter, institutional review board-approved clinical trial. At postsurgical follow-up, investigators (N=17) stratified men into low-, intermediate- or high-risk groups for prostate cancer recurrence based on clinicopathological findings and other factors. Investigators documented their initial treatment plan for each subject and serially collected three serum samples for ProsVue testing. After the ProsVue result was reported, investigators recorded whether or not the initial treatment plan was changed. The proportion of cases referred for secondary treatment before and after ProsVue was reported, and the significance of the difference determined.
RESULTS:
Complete assessments were reported for 225 men, 128 (56.9%) of whom were stratified into intermediate- and high-risk groups. Investigators reported that they would have referred 41/128 (32.0%) at-risk men for secondary treatment. However, after results were known, they referred only 15/128 (11.7%) men. The difference in proportions (−20.3%, 95% confidence interval (CI) −29.9 to −10.3%) is significant (P<0.0001). Odds of a referral was significantly reduced after results were reported (odds ratio 0.28, 95% CI 0.15–0.54, P<0.0001).
CONCLUSIONS:
Knowledge of a ProsVue result had significant impact on the final treatment plan. A ProsVue result ⩽2.0 pg ml−1 month−1 significantly reduced the proportion of men at risk of recurrence who otherwise would have been referred for secondary treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Siegel R, Naishadham D, Jemal A . Cancer statistics, 2013. CA Cancer J Clin 2013; 63: 11–30.
Moul JW, Wu H, Sun L, McLeod DG, Amling C, Lance R et al. Epidemiology of radical prostatectomy for localized prostate cancer in the era of prostate-specific antigen: an overview of the Department of Defense Center for Prostate Disease Research national database. Surgery 2002; 132: 213–219.
Cooperberg MR, Broering JM, Kantoff PW, Carroll PR . Contemporary trends in low risk prostate cancer: risk assessment and treatment. J Urol 2007; 178 (3 Pt 2): S14–S19.
Cohn JA, Wang CE, Lakeman JC, Silverstein JC, Brendler CB, Novakovic KR et al. Primary care physician PSA screening practices before and after the final U.S. Preventive Services Task Force recommendation. Urol Oncol 2014; 32: e23–e30.
Tosoian JJ, Trock BJ, Landis P, Epstein JI, Partin AW, Walsh PC et al. Active surveillance program for prostate cancer: an update of the Johns Hopkins experience. J Clin Oncol 2011; 29: 2185–2190.
Budaus L, Spethmann J, Isbarn H, Schmitges J, Beesch L, Haese A et al. Inverse stage migration in patients undergoing radical prostatectomy: results of 8916 European patients treated within the last decade. BJU Int 2011; 108: 1256–1261.
Silberstein JL, Vickers AJ, Power NE, Fine SW, Scardino PT, Eastham JA et al. Reverse stage shift at a tertiary care center: escalating risk in men undergoing radical prostatectomy. Cancer 2011; 117: 4855–4860.
Louis AS, Kalnin R, Maganti M, Pintilie M, Matthew AG, Finelli A et al. Oncologic outcomes following radical prostatectomy in the active surveillance era. Can Urol Assoc J 2013; 7: e475–e480.
Wilt TJ, Brawer MK, Jones KM, Barry MJ, Aronson WJ, Fox S et al. Radical prostatectomy versus observation for localized prostate cancer. N Engl J Med 2012; 367: 203–213.
Epstein JI, Pizov G, Walsh PC . Correlation of pathologic findings with progression after radical retropubic prostatectomy. Cancer 1993; 71: 3582–3593.
Swanson GP, Riggs M, Hermans M . Pathologic findings at radical prostatectomy: risk factors for failure and death. Urol Oncol 2007; 25: 110–114.
Lughezzani G, Briganti A, Karakiewicz PI, Kattan MW, Montorsi F, Shariat SF et al. Predictive and prognostic models in radical prostatectomy candidates: a critical analysis of the literature. Eur Urol 2010; 58: 687–700.
Amling CL, Bergstralh EJ, Blute ML, Slezak JM, Zincke H . Defining prostate specific antigen progression after radical prostatectomy: what is the most appropriate cut point? J Urol 2001; 165: 1146–1151.
Pound CR, Partin AW, Eisenberger MA, Chan DW, Pearson JD, Walsh PC . Natural history of progression after PSA elevation following radical prostatectomy. JAMA 1999; 281: 1591–1597.
Boorjian SA, Thompson RH, Tollefson MK, Rangel LJ, Bergstralh EJ, Blute ML et al. Long-term risk of clinical progression after biochemical recurrence following radical prostatectomy: the impact of time from surgery to recurrence. Eur Urol 2011; 59: 893–899.
Freedland SJ, Humphreys EB, Mangold LA, Eisenberger M, Dorey FJ, Walsh PC et al. Risk of prostate cancer-specific mortality following biochemical recurrence after radical prostatectomy. JAMA 2005; 294: 433–439.
D’Amico AV, Moul JW, Carroll PR, Sun L, Lubeck D, Chen M-H . Surrogate end point for prostate cancer-specific mortality after radical prostatectomy or radiation therapy. J Natl Cancer Inst 2003; 95: 1376–1383.
Zhou P, Chen MH, McLeod D, Carroll PR, Moul JW, D'Amico AV . Predictors of prostate cancer-specific mortality after radical prostatectomy or radiation therapy. J Clin Oncol 2005; 23: 6992–6998.
Eggener SE, Scardino PT, Walsh PC, Han M, Partin AW, Trock BJ et al. Predicting 15-year prostate cancer specific mortality after radical prostatectomy. J Urol 2011; 195: 869–875.
McDermed JE, Sanders R, Fait S, Klem RE, Sarno MJ, Adams TH et al. Nucleic acid detection immunoassay for prostate specific antigen based on immuno-PCR methodology. Clin Chem 2012; 58: 732–740.
Moul JW, Lilja H, Semmes OJ, Lance RS, Vessella RL, Flei8sher M et al. NADiA ProsVue prostate-specific antigen slope is an independent prognostic marker for identifying men at reduced risk of clinical recurrence of prostate cancer after radical prostatectomy. Urology 2012; 80: 1319–1327.
Thompson IM, Valicenti R, Albertsen PC, Davis BJ, Goldenberg SL, Hahn C et al. Adjuvant and salvage radiotherapy after prostatectomy: AUA/ASTRO guideline. J Urol 2013; 190: 441–449.
Cooperberg MA, Hilton JF, Carroll PR . The CAPRA-S score: a straightforward tool for improved prediction of outcomes after radical prostatectomy. Cancer 2011; 117: 5039–5046.
Punnen S, Freedland SJ, Presti JC Jr, Aronson WJ, Terris MK, Kane CJ et al. Multi-institutional validation of the CAPRA-S score to predict disease recurrence and mortality after radical prostatectomy. Eur Urol 2013; 65: 1171–1177.
Sarno MJ, Davis CS . Robustness of ProsVue™ linear slope for prognostic identification of patients at reduced risk for prostate cancer recurrence: Simulation studies on effects of analytical imprecision and sampling time variation. Clin Biochem 2012; 45: 1479–1482.
Moreira DM, Presti JC, Aronson WJ, Terris MK, Kane CJ, Amling CL et al. Natural history of persistently elevated prostate specific antigen after radical prostatectomy: results from the SEARCH database. J Urol 2009; 182: 2250–2256.
Krupski TL, Kwan L, Litwin MS . Sociodemographic factors associated with postprostatectomy radiotherapy. Prostate Cancer Prostatic Dis 2005; 8: 184–188.
Showalter TN, Ohri N, Teti KG, Foley KA, Keith SW, Trabulsi EJ et al. Physician beliefs and practices for adjuvant and salvage radiation therapy after prostatectomy. Int J Radiat Oncol Biol Phys 2012; 82: e233–e238.
Kim SP, Tilburt JC, Karnes RJ, Ziegenfuss JY, Han LC, Shah ND et al. Variation in treatment recommendations of adjuvant radiation therapy for high-risk prostate cancer by physician specialty. Urology 2013; 82: 807–812.
Williams SB, Gu X, Lipsitz SR, Nguyen PL, Choueiri TK, Hu JC . Utilization and expense of adjuvant cancer therapies following radical prostatectomy. Cancer 2011; 117: 4846–4854.
Hodges JC, Lotan Y, Boike TP, Benton R, Barrier A, Timmerman RD . Cost-effectiveness analysis of SRBT versus IMRT: an emerging initial radiation treatment option for organ-confined prostate cancer. Am J Manag Care 2012; 18: e186–e193.
Moul JW . When should we pull the trigger for post-radical prostatectomy radiotherapy? Eur Urol 2012; 62: 488–490.
Acknowledgements
Arista Molecular, a subsidiary of Beckman Coulter Diagnostics, provided final support to cover the costs for the collection and transportation of patient samples; the CLIA laboratory assayed specimens for each patient and reported the NADiA ProsVue slope results to the clinical sites.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
MT, JMD and MR are employees of Beckman Coulter. The other authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Prostate Cancer and Prostatic Diseases website
Supplementary information
Rights and permissions
About this article
Cite this article
Moul, J., Chen, D., Trabulsi, E. et al. Impact of NADiA ProsVue PSA slope on secondary treatment decisions after radical prostatectomy. Prostate Cancer Prostatic Dis 17, 280–285 (2014). https://doi.org/10.1038/pcan.2014.25
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2014.25