Abstract
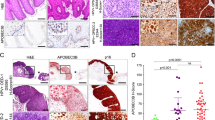
Head and neck squamous cell carcinoma (HNSCC) is the sixth most common malignancy worldwide, and patient outcomes using current treatments remain poor. Tumor development is etiologically associated with tobacco or alcohol use and/or human papillomavirus (HPV) infection. HPV-positive HNSCCs, which frequently harbor wild-type p53, carry a more favorable prognosis and are a biologically distinct subgroup when compared with their HPV-negative counterparts. HPV E7 induces expression of the human DEK gene, both in vitro and in vivo. In keratinocytes, DEK overexpression is sufficient for causing oncogenic phenotypes in the absence of E7. Conversely, DEK loss results in cell death in HPV-positive cervical cancer cells at least in part through p53 activation, and Dek knockout mice are relatively resistant to the development of chemically induced skin papillomas. Despite the established oncogenic role of DEK in HPV-associated cervical cancer cell lines and keratinocytes, a functional role of DEK has not yet been explored in HNSCC. Using an established transgenic mouse model of HPV16 E7-induced HNSCC, we demonstrate that Dek is required for optimal proliferation of E7-transgenic epidermal cells and for the growth of HNSCC tumors. Importantly, these studies also demonstrate that DEK protein is universally upregulated in both HPV-positive and -negative human HNSCC tumors relative to adjacent normal tissue. Furthermore, DEK knockdown inhibited the proliferation of HPV-positive and -negative HNSCC cells, establishing a functional role for DEK in human disease. Mechanistic studies reveal that attenuated HNSCC cell growth in response to DEK loss was associated with reduced expression of the oncogenic p53 family member, ΔNp63. Exogenous ΔNp63 expression rescued the proliferative defect in the absence of DEK, thereby establishing a functional DEK-ΔNp63 oncogenic pathway that promotes HNSCC. Taken together, our data demonstrate that DEK stimulates HNSCC cellular growth and identify ΔNp63 as a novel DEK effector.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Forastiere AA, Ang KK, Brizel D, Brockstein BE, Burtness BA, Cmelak AJ et al. Head and neck cancers. J Natl Compr Canc Netw 2008; 6: 646–695.
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM . Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010; 127: 2893–2917.
Gillison ML, Koch WM, Capone RB, Spafford M, Westra WH, Wu L et al. Evidence for a causal association between human papillomavirusand a subset of head and neck cancers. J Natl Cancer Inst 2000; 92: 709–720.
Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tan PF et al. Human papillomavirus and survival of patients with oropharyngeal cancer. New Engl J Med 2010; 363: 24–35.
Kimple RJ, Smith MA, Blitzer GC, Torres AD, Martin JA, Yang RZ et al. Enhanced radiation sensitivity in HPV-positive head and neck cancer. Cancer Res 2013; 73: 4791–4800.
Gupta S, Kong W, Peng Y, Miao Q, Mackillop WJ . Temporal trends in the incidence and survival of cancers of the upper aerodigestive tract in Ontario and the United States. Int J Cancer 2009; 125: 2159–2165.
Wise-Draper TM, Draper DJ, Gutkind JS, Molinolo AA, Wikenheiser-Brokamp KA, Wells SI . Future directions and treatment strategies for head and neck squamous cell carcinomas. Transl Res 2012; 160: 167–177.
von Lindern M, Fornerod M, van Baal S, Jaegle M, de Wit T, Buijs A et al. The translocation (6;9), associated with a specific subtype of acute myeloid leukemia, results in the fusion of two genes, dek and can, and the expression of a chimeric, leukemia-specific dek-can mRNA. Mol Cell Biol 1992; 12: 1687–1697.
Alexiadis V, Waldmann T, Andersen J, Mann M, Knippers R, Gruss C . The protein encoded by the proto-oncogene DEK changes the topology of chromatin and reduces the efficiency of DNA replication in a chromatin-specific manner. Genes Dev 2000; 14: 1308–1312.
Wise-Draper TM, Allen HV, Thobe MN, Jones EE, Habash KB, Munger K et al. The human DEK proto-oncogene is a senescence inhibitor and an upregulated target of high-risk human papillomavirus E7. J Virol 2005; 79: 14309–14317.
Wise-Draper TM, Allen HV, Jones EE, Habash KB, Matsuo H, Wells SI . Apoptosis inhibition by the human DEK oncoprotein involves interference with p53 functions. Mol Cell Biol 2006; 26: 7506–7519.
Wise-Draper TM, Morreale RJ, Morris TA, Mintz-Cole RA, Hoskins EE, Balsitis SJ et al. DEK proto-oncogene expression interferes with the normal epithelial differentiation program. Am J Pathol 2009; 174: 71–81.
Wise-Draper TM, Mintz-Cole RA, Morris TA, Simpson DS, Wikenheiser-Brokamp KA, Currier MA et al. Overexpression of the cellular DEK protein promotes epithelial transformation in vitro and in vivo. Cancer Res 2009; 69: 1792–1799.
Jabbar S, Strati K, Shin MK, Pitot HC, Lambert PF . Human papillomavirus type 16 E6 and E7 oncoproteins act synergistically to cause head and neck cancer in mice. Virology 2010; 407: 60–67.
Strati K, Lambert PF . Role of Rb-dependent and Rb-independent functions of papillomavirus E7 oncogene in head and neck cancer. Cancer Res 2007; 67: 11585–11593.
Herber R, Liem A, Pitot H, Lambert PF . Squamous epithelial hyperplasia and carcinoma in mice transgenic for the human papillomavirustype 16 E7 oncogene. J Virol 1996; 70: 1873–1881.
Khodadoust MS, Verhaegen M, Kappes F, Riveiro-Falkenbach E, Cigudosa JC, Kim DS et al. Melanoma proliferation and chemoresistance controlled by the DEK oncogene. Cancer Res 2009; 69: 6405–6413.
Privette Vinnedge LM, McClaine R, Wagh PK, Wikenheiser-Brokamp KA, Waltz SE, Wells SI . The human DEK oncogene stimulates beta-catenin signaling, invasion and mammosphere formation in breast cancer. Oncogene 2011; 30: 2741–2752.
Carro MS, Spiga FM, Quarto M, Di Ninni V, Volorio S, Alcalay M et al. DEK Expression is controlled by E2F and deregulated in diverse tumor types. Cell Cycle 2006; 5: 1202–1207.
Lu ZL, Luo DZ, Wen JM . Expression and significance of tumor-related genes in HCC. World J Gastroenterol 2005; 11: 3850–3854.
Bradford CR, Zhu S, Ogawa H, Ogawa T, Ubell M, Narayan A et al. P53 mutation correlates with cisplatin sensitivity in head and neck squamous cell carcinoma lines. Head Neck 2003; 25: 654–661.
Deyoung MP, Ellisen LW . p63 and p73 in human cancer: defining the network. Oncogene 2007; 26: 5169–5183.
Moll UM, Slade N . p63 and p73: roles in development and tumor formation. Mol Cancer Res 2004; 2: 371–386.
Su X, Chakravarti D, Flores ER . p63 steps into the limelight: crucial roles in the suppression of tumorigenesis and metastasis. Nat Rev Cancer 2013; 13: 136–143.
Parkin DM, Bray F, Ferlay J, Pisani P . Global cancer statistics, 2002. CA Cancer J Clin 2005; 55: 74–108.
Leemans CR, Braakhuis BJ, Brakenhoff RH . The molecular biology of head and neck cancer. Nat Rev Cancer 2011; 11: 9–22.
Liu S, Wang X, Sun F, Kong J, Li Z, Lin Z . DEK overexpression is correlated with the clinical features of breast cancer. Pathol Int 2012; 62: 176–181.
Privette Vinnedge LM, Ho SM, Wikenheiser-Brokamp KA, Wells SI . The DEK oncogene is a target of steroid hormone receptor signaling in breast cancer. PLoS One 2012; 7: e46985.
Sitwala KV, Adams K, Markovitz DM . YY1 and NF-Y binding sites regulate the transcriptional activity of the dek and dek-can promoter. Oncogene 2002; 21: 8862–8870.
Alexandrova EM, Petrenko O, Nemajerova A, Romano RA, Sinha S, Moll UM . DeltaNp63 regulates select routes of reprogramming via multiple mechanisms. Cell Death Differ 2013; 20: 1698–1708.
Truong AB, Kretz M, Ridky TW, Kimmel R, Khavari PA . p63 regulates proliferation and differentiation of developmentally mature keratinocytes. Genes Dev 2006; 20: 3185–3197.
Koster MI, Dai D, Marinari B, Sano Y, Costanzo A, Karin M et al. p63 induces key target genes required for epidermal morphogenesis. Proc Natl Acad Sci USA 2007; 104: 3255–3260.
Pignon JC, Grisanzio C, Geng Y, Song J, Shivdasani RA, Signoretti S . p63-expressing cells are the stem cells of developing prostate, bladder, and colorectal epithelia. Proc Natl Acad Sci USA 2013; 110: 8105–8110.
Mills AA, Zheng B, Wang XJ, Vogel H, Roop DR, Bradley A . p63 is a p53 homologue required for limb and epidermal morphogenesis. Nature 1999; 398: 708–713.
Yang A, Schweitzer R, Sun D, Kaghad M, Walker N, Bronson RT et al. p63 is essential for regenerative proliferation in limb, craniofacial and epithelial development. Nature 1999; 398: 714–718.
Romano RA, Smalley K, Magraw C, Serna VA, Kurita T, Raghavan S et al. DeltaNp63 knockout mice reveal its indispensable role as a master regulator of epithelial development and differentiation. Development 2012; 139: 772–782.
Stransky N, Egloff AM, Tward AD, Kostic AD, Cibulskis K, Sivachenko A et al. The mutational landscape of head and neck squamous cell carcinoma. Science 2011; 333: 1157–1160.
Kappes F, Fahrer J, Khodadoust MS, Tabbert A, Strasser C, Mor-Vaknin N et al. DEK is a poly(ADP-ribose) acceptor in apoptosis and mediates resistance to genotoxic stress. Mol Cell Biol 2008; 28: 3245–3257.
Hoskins EE, Morris TA, Higginbotham JM, Spardy N, Cha E, Kelly P et al. Fanconi anemia deficiency stimulates HPV-associated hyperplastic growth in organotypic epithelial raft culture. Oncogene 2009; 28: 674–685.
Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol 2011; 29: 4294–4301.
Rocco JW, Leong CO, Kuperwasser N, DeYoung MP, Ellisen LW . p63 mediates survival in squamous cell carcinoma by suppression of p73-dependent apoptosis. Cancer Cell 2006; 9: 45–56.
Strati K, Pitot HC, Lambert PF . Identification of biomarkers that distinguish human papillomavirus (HPV)-positive versus HPV-negative head and neck cancers in a mouse model. Proc Natl Acad Sci USA 2006; 103: 14152–14157.
Acknowledgements
This work was supported by the Clinical Scientist Training Program at the University of Cincinnati (TWD), Public Health Service Grant R01 CA116316 from the NIH (SIW), NIH Training Grant T32ES007250 (AKA) and R00 CA160639 from the NIH (RJK). All flow cytometric data were acquired using equipment in the Research Flow Cytometry Core in the Division of Rheumatology at Cincinnati Children’s Hospital Medical Center, supported in part by NIH AR-47363, NIH DK78392 and NIH DK90971. We would like to acknowledge the CCHMC pathology core with excellent technical support by Meredith Taylor for Ventana HPV in situ hybridization, Dr Madhavi Kadakia for providing the HA-ΔNp63 construct, Marie Matrka for providing protein lysates, and expert technical support by Dr Ronald Waclaw for use of his Leica microscope.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Adams, A., Hallenbeck, G., Casper, K. et al. DEK promotes HPV-positive and -negative head and neck cancer cell proliferation. Oncogene 34, 868–877 (2015). https://doi.org/10.1038/onc.2014.15
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/onc.2014.15
This article is cited by
-
Nuclear expression of AFF2 C-terminus is a sensitive and specific ancillary marker for DEK::AFF2 carcinoma of the sinonasal tract
Modern Pathology (2022)
-
DEK-AFF2 fusion-associated papillary squamous cell carcinoma of the sinonasal tract: clinicopathologic characterization of seven cases with deceptively bland morphology
Modern Pathology (2021)
-
Determining the molecular landscape and impact on prognosis in HPV-associated head and neck cancer
Cancers of the Head & Neck (2020)
-
Role of the DEK oncogene in the development of squamous cell carcinoma
International Journal of Clinical Oncology (2020)
-
DEK is required for homologous recombination repair of DNA breaks
Scientific Reports (2017)