Key Points
-
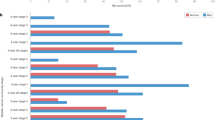
Several studies have reported gender as an independent factor that can influence incidence, recurrence and progression of urological malignancies, but data are inconsistent
-
Men have a threefold higher risk of developing bladder cancer than women
-
Women with bladder cancer are often diagnosed with higher tumour stage and tend to have a worse prognosis than men after adjusting for stage at the diagnosis
-
Men seem to have a higher incidence of upper tract urothelial carcinoma than women; however, survival outcomes might be independent of gender, but data are lacking
-
Men are more frequently diagnosed with renal cell carcinoma than women and also tend to have larger tumours of higher stage and grade
-
Smoking habits, occupational risk factors, tumour biology and sex steroid hormones and their receptors could all have a role in causing the observed gender disparities in patients with urological cancers
Abstract
A gender discrepancy exists in the incidence of both urothelial and kidney carcinomas, with more men presenting with these cancers than women. Men have a threefold greater risk of developing bladder cancer than women, but female gender has been identified as an independent adverse prognostic factor for both recurrence and progression of this disease. In particular, women with bladder cancer are often diagnosed with a higher tumour stage than men. Conclusive data on the influence of gender on outcomes of patients with upper tract urothelial carcinoma are currently lacking, although men seem to have a higher disease incidence, whereas survival outcomes might be independent of gender. Patients with renal cell carcinoma are more often men and they typically have larger tumours and higher stage and grade disease than women with this cancer. Smoking habits, tumour biology, occupational risk factors and sex steroid hormones and their receptors could have a role in these observed gender disparities. The majority of data support the theory that gender influences incidence and prognosis of urothelial and kidney cancers; men and women are different genetically and socially, making the consideration of gender a key factor in the clinical decision-making process. Thus, the inclusion of this variable in validated prognostic tables and nomograms should be discussed as a matter of importance.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Change history
20 October 2015
In the originally published article, the first line of the section on Bladder cancer epidemiology “Bladder cancer is the fourth most common cancer worldwide” should read “Bladder cancer is the fourth most common cancer in men and the seventeenth most common in women, worldwide”. This error has been corrected for the PDF and HTML versions of the article.
References
Page, D. C. 2003 Curt Stern Award address. On low expectation exceeded; or, the genomic salvation of the Y chromosome. Am. J. Hum. Genet. 74, 399–402 (2004).
Shastry, B. S. SNP alleles in human disease and evolution. J. Hum. Genet. 47, 561–566 (2002).
Kunath, F. et al. Is gender becoming relevant in uro-oncological research? A bibliographical analysis. World J. Urol. 31, 1065–1072 (2013).
Lucca, I., Fajkovic, H. & Klatte, T. Sex steroids and gender differences in nonmuscle invasive bladder cancer. Curr. Opin. Urol. 24, 500–505 (2014).
Kunath, F. et al. Is gender becoming relevant in uro-oncological research? A bibliographical analysis. World J. Urol. 31, 1065–1072 (2013).
Siegel, R., Naishadham, D. & Jemal, A. Cancer statistics, 2013. CA Cancer J. Clin. 63, 11–30 (2013).
Wallerand, H. et al. Targeted therapies in non-muscle-invasive bladder cancer according to the signaling pathways. Urol. Oncol. 29, 4–11 (2011).
Burger, M. et al. Epidemiology and risk factors of urothelial bladder cancer. Eur. Urol. 63, 234–241 (2013).
Shariat, S. F. et al. Outcomes of radical cystectomy for transitional cell carcinoma of the bladder: a contemporary series from the Bladder Cancer Research Consortium. J. Urol. 176, 2414–2422 (2006).
Horstmann, M., Witthuhn, R., Falk, M. & Stenzl, A. Gender-specific differences in bladder cancer: a retrospective analysis. Gend. Med. 5, 385–394 (2008).
American Cancer Society. cancer.org[online], (2014).
Davis-Dao, C. A. et al. Lower risk in parous women suggests that hormonal factors are important in bladder cancer etiology. Cancer Epidemiol. Biomarkers Prev. 20, 1156–1170 (2011).
Weibull, C. E., Eloranta, S., Altman, D., Johansson, A. L. V. & Lambe, M. Childbearing and the risk of bladder cancer: a nationwide population-based cohort study. Eur. Urol. 63, 733–738 (2013).
Weibull, C. E., Eloranta, S., Johansson, A. L. V., Altman, D. & Lambe, M. Reply to Silvia Selinski, Daniel Ovsiannikov, Jan G. Hengstler and Klaus Golka's Letter to the editor re: Caroline E. Weibull, Sandra Eloranta, Daniel Altman, Anna L. V. Johansson, Mats Lambe. Childbearing and the risk of bladder cancer: a nationwide population-based cohort study. Eur. Urol. 64, e81 (2013).
Daugherty, S. E. et al. Reproductive factors and menopausal hormone therapy and bladder cancer risk in the NIH-AARP Diet and Health Study. Int. J. Cancer 133, 462–472 (2013).
Cantwell, M. M., Lacey, J. V., Schairer, C., Schatzkin, A. & Michaud, D. S. Reproductive factors, exogenous hormone use and bladder cancer risk in a prospective study. Int. J. Cancer 119, 2398–2401 (2006).
Kluth, L. A. et al. Prognostic and Prediction Tools in Bladder Cancer: a comprehensive review of the literature. Eur. Urol. 68, 238–253 (2015).
Sylvester, R. J. et al. Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: A combined analysis of 2596 patients from seven EORTC trials. Eur. Urol. 49, 466–475 (2006).
Fernandez-Gomez, J. et al. Prognostic factors in patients with non-muscle-invasive bladder cancer treated with bacillus Calmette-Guérin: multivariate analysis of data from four randomized CUETO trials. Eur. Urol. 53, 992–1001 (2008).
Soave, A. et al. Gender-specific outcomes of bladder cancer patients: a stage-specific analysis in a contemporary, homogenous radical cystectomy cohort. Eur. J. Surg. Oncol. 41, 368–377 (2015).
Fajkovic, H. et al. Impact of gender on bladder cancer incidence, staging, and prognosis. World J. Urol. 29, 457–463 (2011).
Chamie, K. et al. Recurrence of high-risk bladder cancer: a population-based analysis. Cancer 119, 3219–3227 (2013).
Shariat, S. F. et al. The effect of age and gender on bladder cancer: a critical review of the literature. BJU Int. 105, 300–308 (2010).
Kluth, L. A. et al. Female gender is associated with higher risk of disease recurrence in patients with primary T1 high-grade urothelial carcinoma of the bladder. World J. Urol. 31, 1029–1036 (2013).
Soave, A. et al. Gender-specific outcomes of bladder cancer patients: A stage-specific analysis in a contemporary, homogenous radical cystectomy cohort. Eur. J. Surg. Oncol. 41, 368–377 (2014).
Messer, J. C. et al. Female gender is associated with a worse survival after radical cystectomy for urothelial carcinoma of the bladder: a competing risk analysis. Urology 83, 863–867 (2014).
Keck, B. et al. Female sex is an independent risk factor for reduced overall survival in bladder cancer patients treated by transurethral resection and radio- or radiochemotherapy. World J. Urol. 31, 1023–1028 (2013).
Boorjian, S. A., Zhu, F. & Herr, H. W. The effect of gender on response to bacillus Calmette-Guérin therapy for patients with non-muscle-invasive urothelial carcinoma of the bladder. BJU Int. 106, 357–361 (2010).
Puente, D. et al. Gender-related differences in clinical and pathological characteristics and therapy of bladder cancer. Eur. Urol. 43, 53–62 (2003).
Crivelli, J. J. et al. Effect of smoking on outcomes of urothelial carcinoma: a systematic review of the literature. Eur. Urol. 65, 742–754 (2014).
Rink, M. et al. Impact of smoking on outcomes of patients with a history of recurrent nonmuscle invasive bladder cancer. J. Urol. 188, 2120–2127 (2012).
Rink, M. et al. Smoking reduces the efficacy of intravesical bacillus Calmette-Guérin immunotherapy in non-muscle-invasive bladder cancer. Eur. Urol. 62, 1204–1206 (2012).
Jamal, A. et al. Current cigarette smoking among adults—United States, 2005–2013. MMWR Morb. Mortal. Wkly Rep. 63, 1108–1112 (2014).
Ng, M. et al. Smoking prevalence and cigarette consumption in 187 countries, 1980–2012 JAMA 311, 183–92 (2014).
Zhang, Y. Understanding the gender disparity in bladder cancer risk: the impact of sex hormones and liver on bladder susceptibility to carcinogens. J. Environ. Sci. Health. C. Environ. Carcinog. Ecotoxicol. Rev. 31, 287–304 (2013).
Miyamoto, H. et al. Expression of androgen and oestrogen receptors and its prognostic significance in urothelial neoplasm of the urinary bladder. BJU Int. 109, 1716–1726 (2012).
Boorjian, S. et al. Androgen receptor expression is inversely correlated with pathologic tumor stage in bladder cancer. Urology 64, 383–388 (2004).
Shortliffe, L. M. D., Ye, Y., Behr, B. & Wang, B. Testosterone Changes Bladder and Kidney Structure in Juvenile Male Rats. J. Urol. 191, 1913–1919 (2014).
Miyamoto, H. et al. Promotion of bladder cancer development and progression by androgen receptor signals. J. Natl Cancer Inst. 99, 558–568 (2007).
Jing, Y. et al. Activated androgen receptor promotes bladder cancer metastasis via Slug mediated epithelial-mesenchymal transition. Cancer Lett. 348, 135–145 (2014).
Gakis, G. & Stenzl, A. Gender-specific differences in muscle-invasive bladder cancer: the concept of sex steroid sensitivity. World J. Urol. 31, 1059–1064 (2013).
Izumi, K. et al. Androgen deprivation therapy prevents bladder cancer recurrence. Oncotarget 5, 12665–12674 (2014).
Wu, S. et al. Somatic mutation of the androgen receptor gene is not associated with transitional cell carcinoma: a 'negative' study by whole-exome sequencing analysis. Eur. Urol. 64, 1018–1019 (2013).
Mir, C. et al. Loss of androgen receptor expression is not associated with pathological stage, grade, gender or outcome in bladder cancer: a large multi-institutional study. BJU Int. 108, 24–30 (2011).
Hsu, I., Vitkus, S., Da, J. & Yeh, S. Role of oestrogen receptors in bladder cancer development. Nat. Rev. Urol. 10, 317–326 (2013).
Kauffman, E. C. et al. Estrogen receptor-β expression and pharmacological targeting in bladder cancer. Oncol. Rep. 30, 131–138 (2013).
Hsu, I. et al. Estrogen receptor alpha prevents bladder cancer via INPP4B inhibited akt pathway in vitro and in vivo. Oncotarget 5, 7917–7935 (2014).
Han, B., Cui, D., Jing, Y., Hong, Y. & Xia, S. Estrogen receptor β (ERβ) is a novel prognostic marker of recurrence survival in non-muscle-invasive bladder cancer potentially by inhibiting cadherin switch. World J. Urol. 32, 149–155 (2014).
Hsu, I. et al. Suppression of ERβ signaling via ERβ knockout or antagonist protects against bladder cancer development. Carcinogenesis 35, 651–661 (2014).
US National Library of Medicine. ClinicalTrials.gov[online],
US National Library of Medicine. ClinicalTrials.gov[online],
Garg, T. et al. Gender disparities in hematuria evaluation and bladder cancer diagnosis: a population based analysis. J. Urol. 192, 1072–1077 (2014).
Henning, A. et al. Do differences in clinical symptoms and referral patterns contribute to the gender gap in bladder cancer? BJU Int. 112, 68–73 (2013).
Cohn, J. A., Vekhter, B., Lyttle, C., Steinberg, G. D. & Large, M. C. Sex disparities in diagnosis of bladder cancer after initial presentation with hematuria: a nationwide claims-based investigation. Cancer 120, 555–561 (2014).
Raman, J. D., Messer, J., Sielatycki, J. A. & Hollenbeak, C. S. Incidence and survival of patients with carcinoma of the ureter and renal pelvis in the USA, 1973–2005 BJU Int. 107, 1059–1064 (2011).
Ehdaie, B., Shariat, S. F., Savage, C., Coleman, J. & Dalbagni, G. Postoperative nomogram for disease recurrence and cancer-specific death for upper tract urothelial carcinoma: comparison to American Joint Committee on Cancer staging classification. Urol. J. 11, 1435–1441 (2014).
Rouprêt, M. et al. European guidelines on upper tract urothelial carcinomas: 2013 update. Eur. Urol. 63, 1059–1071 (2013).
Green, D. A. et al. Urothelial carcinoma of the bladder and the upper tract: disparate twins. J. Urol. 189, 1214–1221 (2013).
Hurel, S. et al. Influence of preoperative factors on the oncologic outcome for upper urinary tract urothelial carcinoma after radical nephroureterectomy. World J. Urol. 33, 335–341 (2014).
Espiritu, P. N. et al. Effect of tumor size on recurrence-free survival of upper tract urothelial carcinoma following surgical resection. Urol. Oncol. 32, 619–624 (2014).
Xylinas, E. et al. Prediction of intravesical recurrence after radical nephroureterectomy: development of a clinical decision-making tool. Eur. Urol. 65, 650–658 (2014).
Tanaka, N. et al. The predictive value of positive urine cytology for outcomes following radical nephroureterectomy in patients with primary upper tract urothelial carcinoma: a multi-institutional study. Urol. Oncol. 32, 48.e19–48.e26 (2014).
Liu, J.-Y. et al. Age-specific effect of gender on upper tract urothelial carcinoma outcomes. Med. Oncol. 30, 640 (2013).
Shyr, C.-R. et al. The expression and actions of androgen receptor in upper urinary tract urothelial carcinoma (UUTUC) tissues and the primary cultured cells. Endocrine 43, 191–199 (2013).
Chen, C.-C. et al. Androgen receptor promotes the migration and invasion of upper urinary tract urothelial carcinoma cells through the upregulation of MMP-9 and COX-2. Oncol. Rep. 30, 979–985 (2013).
Brookman-May, S. D. et al. Time to recurrence is a significant predictor of cancer-specific survival after recurrence in patients with recurrent renal cell carcinoma—results from a comprehensive multi-centre database (CORONA/SATURN-Project). BJU Int. 112, 909–916 (2013).
Hew, M. N. et al. Age and gender related differences in renal cell carcinoma in a European cohort. J. Urol. 188, 33–38 (2012).
Ljungberg, B. et al. EAU guidelines on renal cell carcinoma: 2014 update. Eur. Urol. 67, 913–924 (2015).
Macleod, L. C. et al. Risk factors for renal cell carcinoma in the VITAL study. J. Urol. 190, 1657–1661 (2013).
Iseki, K. Gender differences in chronic kidney disease. Kidney Int. 74, 415–417 (2008).
El-Serag, H. B. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology 142, 1264–1273e1 (2012).
Doumas, M., Papademetriou, V., Faselis, C. & Kokkinos, P. Gender differences in hypertension: myths and reality. Curr. Hypertens. Rep. 15, 321–330 (2013).
Appelman, Y., van Rijn, B. B., Ten Haaf, M. E., Boersma, E. & Peters, S. A. E. Sex differences incardiovascular risk factors and disease prevention. Atherosclerosis 241, 211–218 (2015).
Karami, S., Daugherty, S. E. & Purdue, M. P. A prospective study of alcohol consumption and renal cell carcinoma risk. Int. J. Cancer 137, 238–242 (2014).
Lipworth, L. et al. Renal cell cancer histologic subtype distribution differs by race and sex. BJU Int. http://dx.doi.org/10.1111/bju.12950, (2014).
Steffens, S. et al. Clinical behavior of chromophobe renal cell carcinoma is less aggressive than that of clear cell renal cell carcinoma, independent of Fuhrman grade or tumor size. Virchows Arch. 465, 439–444 (2014).
Brannon, A. R. et al. Meta-analysis of clear cell renal cell carcinoma gene expression defines a variant subgroup and identifies gender influences on tumor biology. Eur. Urol. 61, 258–268 (2012).
Banks, R. E. et al. Genetic and epigenetic analysis of von Hippel-Lindau (VHL) gene alterations and relationship with clinical variables in sporadic renal cancer. Cancer Res. 66, 2000–2011 (2006).
Volpe, A. & Patard, J. J. Prognostic factors in renal cell carcinoma. World J. Urol. 28, 319–327 (2010).
Hofbauer, S. L. et al. Associations between presenting symptoms, clinicopathological parameters, and prognosis in a contemporary series of patients with renal cell carcinoma. Korean J. Urol. 55, 505–510 (2014).
Aron, M., Nguyen, M. M., Stein, R. J. & Gill, I. S. Impact of gender in renal cell carcinoma: an analysis of the SEER database. Eur. Urol. 54, 133–140 (2008).
May, M. et al. Gender differences in clinicopathological features and survival in surgically treated patients with renal cell carcinoma: an analysis of the multicenter CORONA database. World J. Urol. 31, 1073–1080 (2013).
Rampersaud, E. N. et al. The effect of gender and age on kidney cancer survival: younger age is an independent prognostic factor in women with renal cell carcinoma. Urol. Oncol. 32, 30.e9–13 (2014).
Kates, M., Korets, R., Sadeghi, N., Pierorazio, P. M. & McKiernan, J. M. Predictors of locally advanced and metastatic disease in patients with small renal masses. BJU Int. 109, 1463–1467 (2012).
Zucchetto, A. et al. Reproductive, menstrual, and other hormone-related factors and risk of renal cell cancer. Int. J. Cancer 123, 2213–2216 (2008).
Lee, J. E., Hankinson, S. E. & Cho, E. Reproductive factors and risk of renal cell cancer: the Nurses' Health Study. Am. J. Epidemiol. 169, 1243–1250 (2009).
Kutikov, A. et al. Anatomic features of enhancing renal masses predict malignant and high-grade pathology: a preoperative nomogram using the RENAL Nephrometry score. Eur. Urol. 60, 241–248 (2011).
Lane, B. R. et al. A preoperative prognostic nomogram for solid enhancing renal tumors 7 cm or less amenable to partial nephrectomy. J. Urol. 178, 429–434 (2007).
Yu, C.-P. et al. Estrogen inhibits renal cell carcinoma cell progression through estrogen receptor-β activation. PLoS ONE 8, e56667 (2013).
Stone, L. Kidney cancer: Androgen receptor —a new target in renal cell carcinoma? Nat. Rev. Urol. 11, 425 (2014).
He, D. et al. ASC-J9 suppresses renal cell carcinoma progression by targeting an androgen receptor-dependent HIF2α/VEGF signaling pathway. Cancer Res. 74, 4420–4430 (2014).
Williams, E. M., Higgins, J. P., Sangoi, A. R., McKenney, J. K. & Troxell, M. L. Androgen receptor immunohistochemistry in genitourinary neoplasms. Int. Urol. Nephrol. 47, 81–85 (2015).
Zhu, G. et al. The expression and evaluation of androgen receptor in human renal cell carcinoma. Urology 83, e19–e24 (2014).
Noh, S. J. et al. Acetylation status of P53 and the expression of DBC1, SIRT1, and androgen receptor are associated with survival in clear cell renal cell carcinoma patients. Pathology 45, 574–580 (2013).
Tan, C. et al. Impact of Gender in Renal Cell Carcinoma: The Relationship of FABP7 and BRN2 Expression with Overall Survival. Clin. Med. Insights. Oncol. 8, 21–27 (2014).
Mauermann, J. et al. Gender differences in benign renal masses. World J. Urol. 31, 1051–1057 (2013).
Van der Walt, J. D., Reid, H. A., Risdon, R. A. & Shaw, J. H. Renal oncocytoma. A review of the literature and report of an unusual multicentric case. Virchows Arch. A. Pathol. Anat. Histopathol. 398, 291–304 (1983).
Boorjian, S. A. et al. Hormone receptor expression in renal angiomyolipoma: clinicopathologic correlation. Urology 72, 927–932 (2008).
Lane, B. R. et al. Adult cystic nephroma and mixed epithelial and stromal tumor of the kidney: clinical, radiographic, and pathologic characteristics. Urology 71, 1142–1148 (2008).
De Martino, M., Böhm, M. & Klatte, T. Malignant solitary fibrous tumour of the kidney: report of a case and cumulative analysis of the literature. [German] Aktuelle Urol. 43, 59–62 (2012).
Rouprêt, M. et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Cell Carcinoma: 2015 Update. Eur. Urol. http://dx.doi.org/10.1016/j.eururo.2015.06.044.
Witjes, J. A. et al. EAU guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2013 guidelines. Eur. Urol. 65, 778–792 (2014).
Acknowledgements
I.L. was supported by the development fund of the CHUV-University Hospital and the European Urological Scholarship Program.
Author information
Authors and Affiliations
Contributions
I.L. researched data for and wrote the article, I.L., T.K., M.d.M. and S.F.S. contributed to the discussion of the content and all authors contributed to reviewing and editing the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Lucca, I., Klatte, T., Fajkovic, H. et al. Gender differences in incidence and outcomes of urothelial and kidney cancer. Nat Rev Urol 12, 585–592 (2015). https://doi.org/10.1038/nrurol.2015.232
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2015.232
This article is cited by
-
Changes in disease burden and global inequalities in bladder, kidney and prostate cancers from 1990 to 2019: a comparative analysis based on the global burden of disease study 2019
BMC Public Health (2024)
-
Impact of sex on the efficacy of immune checkpoint inhibitors in kidney and urothelial cancers: a systematic review and meta-analysis
World Journal of Urology (2023)
-
Cancer de la vessie: le challenge d’un suivi personnalisé en fonction du patient et des caractéristiques tumorales
Urologie in der Praxis (2023)
-
Molecular differences in renal cell carcinoma between males and females
World Journal of Urology (2023)
-
The germline mutational landscape of genitourinary cancers and its indication for prognosis and risk
BMC Urology (2022)