Abstract
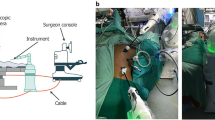
Robot-assisted laparoscopic surgery (RALS) has been proven to be safe and effective for various urological procedures in children, including pyeloplasty, orchiopexy, nephrectomy, and bladder augmentation. The robot system enables delicate and precise movements, which are ideal for the types of reconstructive surgeries that children with urological issues often require, overcoming many of the impediments associated with the conventional laparoscopic approach. RALS helps the relative novice to perform fine surgical techniques and is thought to reduce the learning curve associated with some surgical techniques, such as intracorporeal suturing, owing to the improved freedom of movement of the surgical instruments, the ergonomic positioning of the surgeon, and the 3D vision provided by the robotic system. Given the favourable safety profile and associated benefits of the robot system, including reductions in mean postoperative hospital stay compared with conventional procedures, RALS is becoming more widely adopted by paediatric urologists.
Key Points
-
Robot-assisted laparoscopic surgery (RALS) is safe and effective in the surgical management of various paediatric urological conditions
-
The advantages of RALS include shorter hospitalization times, quicker recovery, and ease of surgery; the disadvantages include longer operative time and increased material cost
-
Special anaesthesia considerations—for example, CO2 absorption and the effect of the pneumoperitoneum on ventilation—should be made when performing RALS in young or small children
-
Modifications to robotic positioning and port placement should be considered when performing RALS in the paediatric population owing to limitations in body surface area and intra-abdominal space
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Lee, R. S., Retik, A. B., Borer, J. G. & Peters, C. A. Paediatric robot assisted laparoscopic dismembered pyeloplasty: comparison with a cohort of open surgery. J. Urol. 175, 683–687 (2006).
Barbosa, J. A. B. A. et al. Patient and parent perceptions of robotic compared to open surgical scars in paediatric urologic surgery. J. Urol. http://dx.doi.org/10.1016/j.juro.2012.12.060.
Gobet, R. in Paediatric robotic and reconstructive urology: a comprehensive guide (ed. Gundeti, M. S.) 120 (Wiley-Blackwell, West Sussex, 2012).
Minnillo, B. J. et al. Long-term experience and outcomes of robotic assisted laparoscopic pyeloplasty in children and young adults. J. Urol. 185, 1455–1460 (2011).
Sorensen, M. D., Delostrinos, C., Johnson, M. H., Grady, R. W. & Lendvay, T. S. Comparison of the learning curve and outcomes of robotic assisted paediatric pyeloplasty. J. Urol. 185, 2517–2522 (2011).
Freilich, D. A. et al. Parental satisfaction after open versus robot assisted laparoscopic pyeloplasty: results from modified Glasgow Children's Benefit Inventory Survey. J. Urol. 183, 704–708 (2010).
Lee, R. S. et al. Early results of robot assisted laparoscopic lithotomy in adolescents. J. Urol. 177, 2306–2310 (2007).
Casale, P., Muchsavage, P., Resnick, M. & Kim, S. S. Robotic ureterocalicostomy in the paediatric population. J. Urol. 180, 2643–2648 (2008).
Badalato, G. M., Haemal, A. K., Menon, M. & Badani, K. K. Current role of robot-assisted pyelolithotomy for the management of large renal calculi: a contemporary analysis. J. Endourol. 23, 1719–1722 (2009).
Elder, J. S. Guidelines for consideration for surgical repair of vesicoureteral reflux. Curr. Opin. Urol. 10, 579 (2000).
Jodal, U. et al. Ten-year results of randomized treatment of children with severe vesicoureteral reflux. Final report of the International Reflux Study in Children. Paediatr. Nephrol. 21, 785 (2006).
Ehrlich, R. M., Gershman, A. & Fuchs, G. Laparoscopic vesicoureteroplasty in children: initial case reports. Urology 43, 255–261 (1994).
Marchini, L. et al. Robotic assisted laparoscopic ureteral reimplantation in children: case matched comparative study with open surgical approach. J. Urol. 185, 1870–1875 (2011).
Casale, P., Patel, R. P. & Kolon, T. F. Nerve sparing extravesical ureteral reimplantation. J. Urol. 179, 1987–1990 (2008).
Lendvay, T. Robotic-assisted laparoscopic management of vesicoureteral reflux. Adv. Urol. 732, 942 (2008).
Smith, R. P., Oliver, J. L. & Peters, C. A., Paediatric robotic extravesical ureteral reimplantation: comparison with open surgery. J. Urol. 185, 1876–1881 (2011).
Gill, I. S., Ponsky, L. E., Desai, M., Kay, R. & Ross, J. H. Laparoscopic cross-trigonal Cohen ureteroneocystostomy: novel technique. J. Urol. 166, 1811–1814 (2001).
Thakre, A. A. & Yeung, C. K. Techinique of intravesical laparoscopy for ureteric reimplantation to treat VUR. Adv. Urol. 937, 231 (2008).
Kutikov, A. et al. Laparoscopic and robotic complex upper-tract reconstruction in children with a duplex collecting system. J. Endourol. 21, 621–624 (2007).
Lee, R. S., Sethi, A. S., Passerotti, A. C. & Peters, C. A. Robot-assisted laparoscopic nephrectomy and contralateral ureteral reimplantation in children. J. Endourol. 24, 123–128 (2010).
Anderberg, M., Kockum, C. C. & Arnbjornsson, E. Paediatric computer-assisted retroperitoneoscopic nephrectomy compared with open surgery. Paediatr. Surg. Int. 27, 761–767 (2011).
Oslen, L. H. & Jorgensen, T. M. Robotically assisted retroperitoneoscopic hemi-nephrectomy in children: initial clinical results. J. Paediatr. Urol. 1, 101–104 (2005).
Lee, R. S., Sethi, A. S. & Passerotti, C. C. Robot assisted laparoscopic partial nephrectomy: a viable and safe option in children. J. Urol. 181, 823–828 (2009).
Nguyen, H. T., Passerotti, C. C., Penna, F. J., Retik, A. B. & Peters, C. A. Robotic assisted laparoscopic Mitrofanoff appendicovesicostomy: preliminary experience in a paediatric population. J. Urol. 182, 1528–1534 (2009).
Thakre, A. A., Yeung, C. K. & Peters, C. Robot-assisted Mitrofanoff and Malone antegrade continence enema reconstruction using divided appendix. J. Endourol. 22, 2393–2396 (2008).
Famakinwa, O. & Gundeti, M. S. Robotic assisted laparoscopic Mitrofanoff appendicovesicostomy (RALMA). Curr. Urol. Rep. 14, 41–45 (2013).
Passerotti, C. C. et al. Robot-assisted laparoscopic ileal bladder augmentation: defining techniques and potential pitfalls. J. Endourol. 22, 355–360 (2008).
Gundeti, M. S., Acharya, S. S., Zagaja, G. P. & Shalhav, A. L. Paediatric robotic-assisted laparoscopic augmentation ileocystoplasty and Mitrofanoff appendicovesicostomy (RALIMA): feasibility of and initial experience with the University of Chicago technique. BJU Int. 107, 962–969 (2011).
Law, G. S., Pérez, L. M. & Joseph, D. B. Two-stage Fowler-Stephens orchiopexy with laparoscopic clipping of the spermatic vessels. J. Urol. 158, 1205–1207 (1997).
Volfson, I. A. et al. Robot-assisted urologic surgery: safety and feasibility in the paediatric population. J. Endourol. 21, 1315–1318 (2007).
Kutikov, A. et al. Incidence of benign pathologic findings at partial nephrectomy for solitary renal mass presumed to be renal cell carcinoma on preoperative imaging. Urology 68, 737–740 (2006).
Tomaszewski, J. J., Casella, D. P., Turner, R. M., Casale, P. & Ost, M. C. Paediatric laparoscopic and robot-assisted laparoscopic surgery: technical considerations. J. Urol. 26, 602–613 (2012).
Joris, J. L. et al. Haemodynamic changes during laparoscopic cholecystectomy. Anesth. Analg. 76, 1067–1071 (1993).
Halachmi, S. et al. Haemodynamic and respiratory effect of paediatric urological laparoscopic surgery: A retrospective study. J. Urol. 170, 1651–1654 (2003).
Rawashdeh, Y. F., Olsen, L. H. & Jorgensen, T. M. in Paediatric Robotic Urology. (ed. Palmer, J. S.) 24 (Humana Press, Cleveland, 2009).
Colodny, A. H. Laparoscopy in paediatric urology: too much of a good thing? Semin. Paediatr. Surg. 5, 23–29 (1996).
Moore, R. G., Kavoussi, L. R. & Bloom, D. A. Postoperative adhesion formation after urological laparoscopy in the paediatric population. J. Urol. 153, 792–795 (1995).
Penna, F. J. & Elder, J. S. in Paediatric robotic and reconstructive urology: a comprehensive guide (ed. Gundeti, M. S.) 32 (Wiley-Blackwell, West Sussex, 2012).
Chiu, A. et al. Effects of intra-abdominal pressure on renal tissue perfusion during laparoscopy. J. Endourol. 8, 99–103 (1994).
McDougall, E. et al. The effect of prolonged pneumoperitoneum on renal function in an animal model. J. Am. Coll. Surg. 182, 317–328 (1996).
Abassi, Z. et al. Adverse effects of pneumoperitoneum on renal function: involvement of the endothelin and nitric oxide systems. Am. J. Physiol. Regul. Integr. Comp. Physiol. 294, R842–R850 (2008).
Uzzo, R. G., Bilsky, M., Mininberg, D. T. & Poppas, D. P. Laparoscopic surgery in children with ventriculoperitoneal shunts: Effect of pneumoperitoneum on intracranial pressure—preliminary experience. Urology 49, 753–757 (1997).
Marchetti, P., Razmaria, A., Zagaja, G. P. & Gundeti, M. S. Management of the ventriculo-peritoneal shunt in paediatric patients during robot-assisted laparoscopic urologic procedures. J. Endourol. 25, 2225–2229 (2011).
Fraser, J. D. et al. The safety of laparoscopy in paediatric patients with ventriculoperitoneal shunts. J. Laparoendoscop. Advan. Surg. Techniques 19, 676–678 (2009).
Chen, C. et al. Malfunction of the da Vinci robotic system in urology. Int. J. Urol. 19, 736–740 (2012).
Zorn, K. C. et al. Da Vinci robot error and failure rates: single institution experience on a single three-arm robot unit of more than 700 consecutive robot-assisted laparoscopic radical prostatectomies. J. Endourol. 21, 1341–1344 (2007).
Lavery, H. J. et al. Robotic equipment malfunction during robotic prostatectomy: a multi-institutional study. J. Endourol. 22, 2165–2168 (2008).
Author information
Authors and Affiliations
Contributions
L. F. Sávio researched the literature for this Review. Both authors contributed towards writing the article. H. T. Nguyen discussed the content with colleagues and reviewed the article prior to submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Sávio, L., Nguyen, H. Robot-assisted laparoscopic urological surgery in children. Nat Rev Urol 10, 632–639 (2013). https://doi.org/10.1038/nrurol.2013.220
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2013.220
This article is cited by
-
Robotic Ureteral Reimplant—the Current Role
Current Urology Reports (2017)