Abstract
Failed hypospadias refers to any hypospadias repair that leads to complications or causes patient dissatisfaction. The complication rate after hypospadias repairs ranges from 5–70%, but the actual incidence of failed hypospadias is unknown as complications can become apparent many years after surgery and series with lifelong follow-up data do not exist. Moreover, little is known about uncomplicated repairs that fail in terms of patient satisfaction. Risk factors for complications include factors related to the hypospadias (severity of the condition and characteristics of the urethral plate), the patient (age at surgery, endocrine environment, and wound healing impairment), the surgeon (technique selection and surgeon expertise), and the procedure (technical details and postoperative management). The most important factors for preventing complications are surgeon expertise (number of cases treated per year), interposition of a barrier layer between the urethroplasty and the skin, and postoperative urinary drainage. Major complications associated with failed hypospadias include residual curvature, healing complications (preputial dehiscence, glans dehiscence, fistula formation, and urethral breakdown), urethral obstruction (meatal stenosis, urethral stricture, and functional obstruction), urethral diverticula, hairy urethra, and penile skin deficiency.
Key Points
-
Hypospadias failure is any repair that leads to complications or causes patient dissatisfaction; the latter is very subjective and difficult to assess
-
Surgeon expertise, interposition of barrier layers between the urethroplasty and the skin, and urinary drainage are the most important factors for preventing hypospadias failure
-
The most common complications associated with hypospadias failure include residual curvature, fistula formation, urethral breakdown, meatal stenosis, and urethral stricture
-
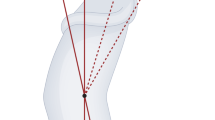
Residual curvature can be addressed by dorsal shortening of the penis; however, urethral substitution should be performed if curvature is caused by a contraction of the ventral neourethra
-
Reurethroplasty technique should be selected according to residual curvature secondary to contracture of the neourethra, quality of the residual urethral plate, and suitability of genital skin for elevating flaps
-
Urethral dilatation and direct vision internal urethrotomy are much less effective than reurethroplasty for treating urethral strictures after hypospadias repair
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Baskin, L. S. & Ebber, M. B. Hypospadias: anatomy, etiology, and technique. J. Pediatr. Surg. 41, 463–472 (2006).
Castagnetti, M. & El-Ghoneimi, A. Surgical management of primary severe hypospadias in children: systematic 20-year review. J. Urol. 184, 1469–1474 (2010).
Smith, E. D. The history of hypospadias. Pediatr. Surg. Int. 12, 81–85 (1997).
Rynja, S. P., de Jong, T. P., Bosch, J. L. & de Kort, L. M. Functional, cosmetic and psychosexual results in adult men who underwent hypospadias correction in childhood. J. Pediatr. Urol. 7, 504–515 (2011).
Braga, L. H. et al. Ventral penile lengthening versus dorsal plication for severe ventral curvature in children with proximal hypospadias. J. Urol. 180, 1743–1747 (2008).
Mureau, M. A., Slijper, F. M., Slob, A. K., Verhulst, F. C. & Nijman, R. J. Satisfaction with penile appearance after hypospadias surgery: the patient and surgeon view. J. Urol. 155, 703–706 (1996).
Barbagli, G., Perovic, S., Djinovic, R., Sansalone, S. & Lazzeri, M. Retrospective descriptive analysis of 1,176 patients with failed hypospadias repair. J. Urol. 183, 207–211 (2010).
Myers, J. B., McAninch, J. W., Erickson, B. A. & Breyer, B. N. Treatment of adults with complications from previous hypospadias surgery. J. Urol. 188, 459–463 (2012).
Prasad, M. M., Marks, A., Vasquez, E., Yerkes, E. B. & Cheng, E. Y. Published surgical success rates in pediatric urology—fact or fiction? J. Urol. 188, 1643–1648 (2012).
Snodgrass, W. T., Bush, N. & Cost, N. Tubularized incised plate hypospadias repair for distal hypospadias. J. Pediatr. Urol. 6, 408–413 (2010).
Shukla, A. R., Patel, R. P. & Canning, D. A. The 2-stage hypospadias repair. Is it a misnomer? J. Urol. 172, 1714–1716 (2004).
Hinder, U. T., Duran, F. R. & Caravaca, M. P. in Long term results in plastic and reconstructive surgery 1st edn Vol. 1 (ed. Goldwyn, R. M.; Boston Little Brown & Co., USA, 1980).
Spinoit, A. F., Poelaert, F., Groen, L. A., Van Laecke, E. & Hoebeke, P. Hypospadias repair in a single reference centre: Long term follow-up is mandatory to detect the real complication rate! J. Urol. http://dx.doi.org/10.1016/j.juro.2012.12.100.
Wood, H. M., Kay, R., Angermeier, K. W. & Ross, J. H. Timing of the presentation of urethrocutaneous fistulas after hypospadias repair in pediatric patients. J. Urol. 180, 1753–1756 (2008).
Nuininga, J. E., De Gier, R. P. E., Verschuren, R. & Feitz, W. F. J. Long-term outcome of different types of 1-stage hypospadias repair. J. Urol. 174, 1544–1548 (2005).
Vandersteen, D. R. & Husmann, D. A. Late onset recurrent penile chordee after successful correction at hypospadias repair. J. Urol. 160, 1131–1133 (1998).
Sarhan, O. M. et al. Factors affecting outcome of tubularized incised plate (TIP) urethroplasty: single center experience with 500 cases. J. Pediatr. Urol. 5, 378–382 (2009).
Holland, A. J. & Smith, G. H. Effect of the depth and width of the urethral plate on tubularized incised plate urethroplasty. J. Urol. 164, 489–491 (2000).
Nguyen, M. T., Snodgrass, W. T. & Zaontz, M. R. Effect of urethral plate characteristics on tubularized incised plate urethroplasty. J. Urol. 171, 1260–1262 (2004).
Sarhan, O., Saad, M., Helmy, T. & Hafez, A. Effect of suturing technique and urethral plate characteristics on complication rate following hypospadias repair: a prospective randomized study. J. Urol. 182, 682–685 (2009).
El-Hout, Y. et al. Assessment of urethral plate appearance through digital photography: do pediatric urologists agree in their visual impressions of the urethral plate in children with hypospadias? J. Pediatr. Urol. 6, 294–300 (2010).
Snodgrass, W., Macedo, A., Hoebeke, P. & Mouriquand, P. D. Hypospadias dilemmas: a round table. J. Pediatr. Urol. 7, 145–157 (2011).
Castagnetti, M. & El-Ghoneimi, A. The influence of perioperative factors on primary severe hypospadias repair. Nat. Rev. Urol. 8, 198–206 (2011).
American Academy of Pediatrics. Section on Urology. Action committee for determining timing of elective surgery on the genitalia of male children. Timing of elective surgery on the genitalia of male children with particular reference to the risks, benefits and psychological effects of surgery and anesthesia. American Academy of Pediatrics. Pediatrics 97, 590–594 (1996).
Jones, B. C., O'Brien, M., Chase, J., Southwell, B. R. & Hutson, J. M. Early hypospadias surgery may lead to better psychosexual outcome. J. Urol. 182, 1744–1750 (2009).
Weber, D. M., Schonbucher, V. B., Gobet, R., Gerber, A. & Landot, M. A. Is there an ideal age for hypospadias repair? A pilot study. J. Pediatr. Urol. 5, 345–350 (2009).
Marrocco, G., Vallasciani, S., Fiocca, G. & Calisti, A. Hypospadias surgery: a 10-year review. Pediatr. Surg. Int. 20, 200–203 (2004).
Ziada, A. et al. Outcomes of hypospadias repair in older children: a prospective study. J. Urol. 185, 2483–2486 (2011).
Dodson, J. L., Baird, A. D., Baker, L. A., Docimo, S. G. & Mathews, R. I. Outcomes of delayed hypospadias repair: implications for decision making. J. Urol. 178, 278–281 (2007).
Kocherov, S. et al. Outcome of hypospadias repair in toilet-trained children and adolescents. Pediatr. Surg. Int. 28, 429–433 (2012).
Eassa, W., Jednak, R., Capolicchio, J. P., Brzezinski, A. & El-Sherbiny, M. Risk factors for re-operation following tubularized incised plate urethroplasty: a comprehensive analysis. Urology 77, 716–720 (2011).
Bush, N. C., Holzer, M., Zhang, S. & Snodgrass, W. Age does not impact risk for urethroplasty complications after tubularized incised plate repair of hypospadias in prepubertal boys. J. Pediatr. Urol. 9, 252–256 (2013).
Koff, S. A. & Jayanthi, V. R. Preoperative treatment with human chorionic gonadotropin in infancy decreases the severity of proximal hypospadias and chordee. J. Urol. 162, 1435–1439 (1999).
Gorduza, D. B. et al. Does androgen stimulation prior to hypospadias surgery increase the rate of healing complications? A preliminary report. J. Pediatr. Urol. 7, 158–161 (2011).
Gilliver, S. C. et al. 5α-dihydrotestosterone (DHT) retards wound closure by inhibiting re-epithelialization. J. Pathol. 217, 73–82 (2009).
Gilliver, S. C. et al. The hormonal regulation of cutaneous wound healing. Clin. Dermatol. 25, 56–62 (2007).
Gilliver, S. C. et al. Sex steroids and cutaneous wound healing: the contrasting influences of estrogens and androgens. Climacteric 10, 276–288 (2007).
de Mattos e Silva, E. et al. Outcome of severe hypospadias repair using three different techniques. J. Pediatr. Urol. 5, 205–211 (2009).
Morera, A. M. et al. Is hypospadias due to metalloproteinase overactivity? Presented at the European Society for Paediatric Urology (ESPU) 2004 meeting.
Cook, A. et al. A multicenter evaluation of technical preferences for primary hypospadias repair. J. Urol. 174, 2354–2357 (2005).
Springer, A., Krois, W. & Horcher, E. Trends in hypospadias surgery: results of a worldwide survey. Eur. Urol. 60, 1184–1189 (2011).
Koyle, M. A. Hypospadias: a 30-year personal journey. Scand. J. Surg. 100, 250–255 (2011).
Castagnetti, M., Zhapa, E. & Rigamonti, W. Primary severe hypospadias: comparison of reoperation rates and parental perception of urinary symptoms and cosmetic outcomes among 4 repairs. J. Urol. 189, 1508–1513 (2013).
Vallasciani, S., Berrettini, A., Manzoni, G. & Marrocco, G. Observational retrospective study on acquired megalourethra after primary proximal hypospadias repair and its recurrence after tapering. J. Pediatr. Urol. 9, 364–367 (2013).
Chrzan, R., Dik, P., Klijn, A. J. & de Jong, T. P. Quality assessment of hypospadias repair with emphasis on techniques used and experience of pediatric urologic surgeons. Urology 70, 148–152 (2007).
Marrocco, G., Calisti, A., Materia, E., Baglio, G. & Tancioni, V. The efficacy of surgical treatment of hypospadias: analysis of hospital data from Lazio region during the three year period (1996–1998). Pediatr. Med. Chir. 24, 223–227 (2002).
Chuang, J. H. & Shieh, C. S. Two-layer versus one-layer closure in transverse island flap repair of posterior hypospadias. J. Pediatr. Surg. 30, 739–742 (1995).
Savanelli, A., Esposito, C. & Settimi, A. A prospective randomized comparative study on the use of ventral subcutaneous flap to prevent fistulas in the Snodgrass repair for distal hypospadias. World J. Urol. 25, 641–645 (2007).
Cimador, M., Pensabene, M., Sergio, M., Catalano, P. & de Grazia, E. Coverage of urethroplasty in pediatric hypospadias: randomized comparison between different flaps. Int. J. Urol. http://dx.doi.org/10.1111/iju.12092.
Gipson, M. Hypospadias repair using polyglycolic acid sutures. Br. J. Plast. Surg. 28, 135–138 (1975).
Bartone, F., Shore, N., Newland, J., King, L. & DuPlessis, D. The best suture for hypospadias? Urology 29, 517–522 (1987).
Cimador, M. et al. Suture materials: do they affect fistula and stricture rates in flap urethroplasties? Urol. Int. 73, 320–324 (2004).
Guarino, N., Vallasciani, S. A. & Marrocco, G. A new suture material for hypospadias surgery: a comparative study. J. Urol. 181, 1318–1323 (2009).
Grobbelaar, A. O., Laing, J. H., Harrison, D. H. & Sanders, R. Hypospadias repair: the influence of postoperative care and a patient factor on surgical morbidity. Ann. Plast. Surg. 37, 612–617 (1996).
Chuang, J. H. & Shieh, C. S. Two-layer versus one-layer closure in transverse island flap repair of posterior hypospadias. J. Pediatr. Surg. 30, 739–742 (1995).
Ben Meir, D. & Livne, P. M. Is prophylactic antimicrobial treatment necessary after hypospadias repair? J. Urol. 171, 2621–2622 (2004).
McLorie, G. et al. Prospective randomized clinical trial to evaluate methods of postoperative care of hypospadias. J. Urol. 165, 1669–1672 (2001).
Van Savage, J. G., Palanca, L. G. & Slaughenhoupt, B. L. A prospective randomized trial of dressings versus no dressings for hypospadias repair. J. Urol. 164, 981–983 (2000).
Braga, L. H., Lorenzo, A. J., Suoub, M. & Bägli, D. J. Is statistical significance sufficient? Importance of interaction and confounding in hypospadias analysis. J. Urol. 184, 2510–2515 (2010).
Perovic, S. et al. Surgical challenge in patients who underwent failed hypospadias repair: is it time to change? Urol. Int. 85, 427–435 (2010).
Horton, C. E. & Devine, C. J. A one-stage repair for hypospadias cripples. Plast. Reconstr. Surg. 45, 425–430 (1970).
Taylor, J. R., Lockwood, A. P. & Taylor, A. J. The prepuce: specialized mucosa of the penis and its loss to circumcision. Br. J. Urol. 77, 291–295 (1996).
Winkelmann, R. K. The erogenous zones: their nerve supply and its significance. Proc. Staff Meet Mayo Clin. 34, 39–47 (1959).
Cold, C. J. & Taylor, J. R. The prepuce. BJU Int. 83 (Suppl. 1), 34–44 (1999).
Leclair, M. D., Benyoucef, N. & Héloury, Y. [Morbidity of foreskin reconstruction in distal hypospadias repair surgery]. Prog. Urol. 18, 475–479 (2008).
Cimador, M., Castagnetti, M. & De Grazia, E. Risks and relevance of preputial reconstruction in hypospadia repair. Pediatr. Med. Chir. 25, 269–272 (2003).
Castagnetti, M., Cimador, M. & De Grazia, E. Re: reconstruction of the hypospadiac hooded prepuce. J. Urol. 171, 2385 (2004).
Castagnetti, M. Commentary to 'Foreskin retractility following hypospadias repair with preputioplasty—Medium term outcomes'. J. Pediatr. Urol. http://dx.doi.org/10.1016/j.jpurol.2013.03.019.
Snodgrass, W., Cost, N., Nakonezny, P. A. & Bush, N. Analysis of risk factors for glans dehiscence after tubularized incised plate hypospadias repair. J. Urol. 185, 1845–1851 (2011).
Zaontz, M. R. & Dean, G. E. Glandular hypospadias repair. Urol. Clin. North Am. 29, 291–298 (2002).
Emir, L. & Erol, D. Mathieu urethroplasty as a salvage procedure: 20-year experience. J. Urol. 169, 2325–2326 (2003).
Muruganandham, K. et al. Urethrocutaneous fistula after hypospadias repair: outcome of three types of closure techniques. Pediatr. Surg. Int. 26, 305–308 (2010).
Elbakry, A. Management of urethrocutaneous fistula after hypospadias repair: 10 years' experience. BJU Int. 88, 590–595 (2001).
Cimador, M., Castagnetti, M. & De Grazia, E. Urethrocutaneous fistula repair after hypospadias surgery. BJU Int. 92, 621–623 (2003).
Karamürsel, S. & Celebiog˘lu, S. Urethral advancement for recurrent distal hypospadias fistula treatment. Ann. Plast. Surg. 56, 423–426 (2006).
Snodgrass, W. T., Bush, N. & Cost, N. Algorithm for comprehensive approach to hypospadias reoperation using 3 techniques. J. Urol. 182, 2885–2891 (2009).
Eliçevik, M., Tireli, G., Demirali, O., Unal, M. & Sander, S. Tubularized incised plate urethroplasty for hypospadias reoperations in 100 patients. Int. Urol. Nephrol. 39, 823–827 (2007).
Jayanthi, V. R. et al. Can previously relocated penile skin be successfully used for salvage hypospadias repair? J. Urol. 152, 740–743 (1994).
Snodgrass, W. & Elmore, J. Initial experience with staged buccal graft (Bracka) hypospadias reoperations. J. Urol. 172, 1720–1724 (2004).
Castagnetti, M. & Rigamonti, W. Aptness and complications of labial mucosa grafts for the repair of anterior urethral defects in children and adults: single centre experience with 115 cases. World J. Urol. 27, 799–803 (2009).
Leslie, B. et al. Critical outcome analysis of staged buccal mucosa graft urethroplasty for prior failed hypospadias repair in children. J. Urol. 185, 1077–1082 (2011).
Nitkunan, T., Johal, N., O'Malley, K. & Cuckow, P. Secondary hypospadias repair in two stages. J. Pediatr. Urol. 2, 559–563 (2006).
Simonato, A. et al. Lingual mucosal graft urethroplasty for anterior urethral reconstruction. Eur. Urol. 54, 79–85 (2008).
Castagnetti, M., Ghirardo, V., Capizzi, A., Andretta, M. & Rigamonti, W. Donor site outcome after oral mucosa harvest for urethroplasty in children and adults. J. Urol. 180, 2624–2628 (2008).
Maarouf, A. M. et al. Buccal versus lingual mucosal graft urethroplasty for complex hypospadias repair. J. Pediatr. Urol. http://dx.doi.org/10.1016/j.jpurol.2012.08.013.
Haxhirexha, K. N., Castagnetti, M., Rigamonti, W. & Manzoni, G. A. Two-stage repair in hypospadias. Indian J. Urol. 24, 226–232 (2008).
Lorenzo, A. J. & Snodgrass, W. T. Regular dilatation is unnecessary after tubularized incised-plate hypospadias repair. BJU Int. 89, 94–97 (2002).
Gargollo, P. C., Cai, A. W., Borer, J. G. & Retik, A. B. Management of recurrent urethral strictures after hypospadias repair: is there a role for repeat dilation or endoscopic incision? J. Pediatr. Urol. 7, 34–38 (2011).
Lumen, N. et al. Etiology of urethral stricture disease in the 21st century. J. Urol. 182, 983–987 (2009).
Andersson, M., Doroszkiewicz, M., Arfwidsson, C., Abrahamsson, K. & Holmdahl, G. Hypospadias repair with tubularized incised plate: does the obstructive flow pattern resolve spontaneously? J. Pediatr. Urol. 7, 441–445 (2011).
Husmann, D. A. & Rathbun, S. R. Long-term followup of visual internal urethrotomy for management of short (less than 1 cm) penile urethral strictures following hypospadias repair. J. Urol. 176, 1738–1741 (2006).
Scherz, H. C., Kaplan, G. W., Packer, M. G. & Brock, W. A. Post-hypospadias repair urethral strictures: a review of 30 cases. J. Urol. 140, 1253–1255 (1988).
Ferro, F., Vallasciani, S., Borsellino, A., Atzori, P. & Martini, L. Snodgrass urethroplasty: grafting the incised plate--10 years later. J. Urol. 182, 1730–1734 (2009).
Djordjevic, M. L. et al. “Hanging” of the buccal mucosal graft for urethral stricture repair after failed hypospadias. J. Urol. 185, 2479–2482 (2011).
Meeks, J. J., Erickson, B. A. & Gonzalez, C. M. Staged reconstruction of long segment urethral strictures in men with previous pediatric hypospadias repair. J. Urol. 181, 685–689 (2009).
Uemura, S., Hutson, J. M., Woodward, A. A., Kelly, J. H. & Chow, C. W. Balanitis xerotica obliterans with urethral stricture after hypospadias repair. Pediatr. Surg. Int. 16, 144–145 (2000).
Mattioli, G. et al. Lichen sclerosus et atrophicus in children with phimosis and hypospadias. Pediatr. Surg. Int. 18, 273–275 (2002).
Depasquale, I., Park, A. J. & Bracka, A. The treatment of balanitis xerotica obliterans. BJU Int. 86, 459–465 (2000).
Kumar, M. V. & Harris, D. L. Balanitis xerotica obliterans complicating hypospadias repair. Br. J. Plast. Surg. 52, 69–71 (1999).
Aigen, A. B., Khawand, N., Skoog, S. T. & Belman, A. B. Acquired megalourethra: an uncommon complication of the transverse preputial island flap urethroplasty. J. Urol. 137, 712–713 (1987).
Elbakry, A. Complications of the preputial island flap-tube urethroplasty. BJU Int. 84, 89–94 (1999).
Singh, I. & Hemal, A. K. Recurrent urethral hairball and stone in a hypospadiac: management prevention. J. Endourol. 15, 645–647 (2001).
Crain, D. S., Miller, O. F., Smith, L. J., Roberts, J. L. & Ross, E. V. Transcutaneous laser hair ablation for management of intraurethral hair after hypospadias repair: initial experience. J. Urol. 170, 1948–1949 (2003).
Cohen, S., Livne, P. M., Ad-El, D. & Lapidoth, M. CO2 laser desiccation urethral hair post-penoscrotal hypospadias repair. J. Cosmet. Laser Ther. 9, 241–243 (2007).
Beiko, D., Pierre, S. A. & Leonard, M. P. Urethroscopic holmium:YAG laser epilation of urethral diverticular hair follicles following hypospadias repair. J. Pediatr. Urol. 7, 231–232 (2011).
Hayashi, Y. et al. Management of urethral calculi associated with hairballs after urethroplasty for severe hypospadias. Int. J. Urol. 14, 161–163 (2007).
Mir, T., Simpson, R. L. & Hanna, M. K. The use of tissue expanders for resurfacing of the penis for hypospadias cripples. Urology 78, 1424–1429 (2011).
Thompson, J. H., Zmaj, P., Cummings, J. M. & Steinhardt, G. F. An approach for using full thickness skin grafts for complex penile surgeries in children. J. Urol. 175, 1869–1871 (2006).
Author information
Authors and Affiliations
Contributions
M. Cimador wrote, edited, and discussed this Review with colleagues. S. Vallasciani and M. Castagnetti researched data and contributed towards writing the article. In addition, M. Castagnetti made substantial contributions towards discussions of content. G. Manzoni, W. Rigamonti, and E. De Grazia reviewed and edited the manuscript prior to submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Cimador, M., Vallasciani, S., Manzoni, G. et al. Failed hypospadias in paediatric patients. Nat Rev Urol 10, 657–666 (2013). https://doi.org/10.1038/nrurol.2013.164
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2013.164
This article is cited by
-
The long-term consequences of the hypospadias salvage repair issue
BMC Pediatrics (2024)
-
Lateral incision 1-stage urethroplasty with oral mucosal graft for patients with penile urethral stricture after hypospadias repair—a preliminary report
BMC Urology (2023)
-
Glans dehiscence after severe hypospadias repair. Is it a real complication? Clues from a study in post-pubertal patients
Pediatric Surgery International (2023)
-
Surgical management of primary severe hypospadias in children: an update focusing on penile curvature
Nature Reviews Urology (2022)
-
Hypospadias repair can be associated with a hairy urethra. Reply to a letter to the Editor concerning the publication “Postoperative outcomes in distal hypospadias: a meta-analysis of Mathieu and tubularized incised plate repair methods for the development of urethrocutaneous fistula and urethral stricture”
Pediatric Surgery International (2022)