Key Points
-
Migraine is a chronic and disabling brain disorder that typically manifests as attacks of one-sided, often throbbing head pain that is worsened by movement and is associated with nausea and sensitivity to light (photophobia) and sound (phonophobia).
-
Migraine is thought to involve activation of the trigeminovascular system, which includes the efferent projections to the pain-producing dura mater and large intracranial vessels, and the afferent projection to the central trigeminal nucleus caudalis (TNC). It is a pivotal relay centre that passes nociceptive information from the cranial vasculature to the brainstem and higher processing centres.
-
Several studies have demonstrated that structures within the brainstem, midbrain and forebrain — areas that are known to be involved in the modulation of the trigeminovascular system — are active during spontaneous migraine. This suggests that dysfunction within these regions may be responsible for a migrainous phenotype.
-
In the pons, the superior salivatory nucleus (SuS) has a reflex connection with the TNC and provides the cells of origin of the parasymapathetic outflow to the cranial vasculature. Activation contributes to the autonomic symptoms in primary headache and has now been shown to also activate and exacerbate neuronal firing in the TNC.
-
In the midbrain, the ventrolateral periaqueductal grey and rostral ventromedial medulla provide descending control of trigeminovascular nociceptive responses, controlled by 'on'- and 'off'-cell activation. Additionally, connections with hypothalamic, thalamic and limbic nuclei, which are involved in homeostatic processes, suggest that 'on'–'off' cell activation, or the dysregulation of these cells, may be involved in triggering migraine and may contribute to migrainous symptoms.
-
In the forebrain, the hypothalamus is involved in the control of the sleep–wake cycle, feeding, thirst, urination and arousal — behaviours that are altered during premonitory symptoms. Disruption to the regular functioning of these behaviours can also serve as triggers for migraine. Bidirectional connections with the SuS may provide a link between the potential site of origin of migraine triggers, premonitory symptoms and other migraine symptoms, and descending modulation of trigeminovascular nociceptive traffic.
-
The thalamus is a major centre for processing nociceptive information. Sensitization of third-order trigeminovascular nociceptive neurons in thalamic nuclei is likely to contribute to the cutaneous allodynia that is experienced by patients. Sensitized neurons of the posterior thalamus that receive projections from areas of the visual cortex respond to bright light with exacerbated firing. This may provide a neural explanation for the photophobia that is exhibited by patients who suffer from migraine.
-
We believe that the explanation that best accounts for the multifaceted migrainous symptomology is a dysfunction of the brainstem or diencenphalic nuclei that process nociceptive inputs of the craniovascular afferents. The bidirectional connections of the many brainstem and diencephalic nuclei mean that dysfunction can create a brain state that produces many simultaneous symptoms. The next best theory involves a sequential sensitization of trigeminovascular synapses up to the thalamus that requires an initial peripheral nociceptive event. This cannot explain many centrally mediated migraine triggers or the premonitory symptoms that precede any pain.
Abstract
Migraine is a common and complex brain disorder. Although it is clear that head pain is a key manifestation of the disorder for most patients, what drives the activation of neuronal pain pathways in susceptible patients is less obvious. There is growing evidence that migraine pathophysiology may, in part, include dysfunction of subcortical structures. These include diencephalic and brainstem nuclei that can modulate the perception of activation of the trigeminovascular system, which carries sensory information from the cranial vasculature to the brain. Dysfunction of these nuclei, and their connections to other key brain centres, may contribute to the cascade of events that results in other symptoms of migraine — such as light and sound sensitivity — thus providing a comprehensive explanation of the neurobiology of the disorder.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Goadsby, P. J., Lipton, R. B. & Ferrari, M. D. Migraine — current understanding and treatment. N. Engl. J. Med. 346, 257–270 (2002).
Lipton, R. B. et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 68, 343–349 (2007).
Lipton, R. B., Stewart, W. F., Diamond, S., Diamond, M. L. & Reed, M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 41, 646–657 (2001).
Stewart, W. F., Ricci, J. A., Chee, E. & Morganstein, D. Lost productive work time costs from health conditions in the United States: results from the American Productivity Audit. J. Occup. Environ. Med. 45, 1234–1246 (2003).
Andlin-Sobocki, P., Jonsson, B., Wittchen, H. U. & Olesen, J. Cost of disorders of the brain in Europe. Eur. J. Neurol. 12, 1–27 (2005).
Headache Classification Committee of the International Headache Society. The international classification of headache disorders. 2nd ed. Cephalalgia Suppl. 24, 9–160 (2004).
Ferrari, M. D. Treatment of migraine attacks with sumatriptan. The Subcutaneous Sumatriptan International Study Group. N. Engl. J. Med. 325, 316–321 (1991).
Humphrey, P. P. A. et al. Preclinical studies on the anti-migraine drug, sumatriptan. Eur. Neurol. 31, 282–290 (1991).
May, A. & Goadsby, P. J. The trigeminovascular system in humans: pathophysiologic implications for primary headache syndromes of the neural influences on the cerebral circulation. J. Cereb. Blood Flow Metab. 19, 115–127 (1999).
Goadsby, P. J. Pathophysiology of migraine. Neurologic Clinics 27, 335–360 (2009).
Goadsby, P. J., Charbit, A. R., Andreou, A. P., Akerman, S. & Holland, P. R. Neurobiology of migraine. Neuroscience 161, 327–341 (2009).
Dalkara, T., Nozari, A. & Moskowitz, M. A. Migraine aura pathophysiology: the role of blood vessels and microembolisation. Lancet Neurol. 9, 309–317 (2010).
Eikermann-Haerter, K. & Moskowitz, M. A. Animal models of migraine headache and aura. Curr. Opin. Neurol. 21, 294–300 (2008).
Eikermann-Haerter, K. & Ayata, C. Cortical spreading depression and migraine. Curr. Neurol. Neurosci. Rep. 10, 167–173 (2010).
Wolthausen, J., Sternberg, S., Gerloff, C. & May, A. Are cortical spreading depression and headache in migraine causally linked? Cephalalgia 29, 244–249 (2009).
Goadsby, P. J. Migraine, aura and cortical spreading depression: why are we still talking about it? Ann. Neurol. 49, 4–6 (2001).
Ayata, C. Cortical spreading depression triggers migraine attack: pro. Headache 50, 725–730 (2010).
Charles, A. Does cortical spreading depression initiate a migraine attack? Maybe not. Headache 50, 731–733 (2010).
McNaughton, F. L. & Feindel, W. in Physiological Aspects Of Clinical Neurology (ed. Rose, F. C.) 279–293 (Blackwell Scientific, Oxford, 1977).
Penfield, W. & F., M. Dural headache and innervation of the dura mater. Arch. Neurol. Psychiatry 44, 43–75 (1940).
Ray, B. S. & Wolff, H. G. Experimental studies on headache. Pain sensitive structures of the head and their significance in headache. Arch. Surg. 41, 813–856 (1940).
Goadsby, P. J. & Zagami, A. S. Stimulation of the superior sagittal sinus increases metabolic activity and blood flow in certain regions of the brainstem and upper cervical spinal cord of the cat. Brain 114, 1001–1011 (1991).
Kaube, H., Keay, K. A., Hoskin, K. L., Bandler, R. & Goadsby, P. J. Expression of c-Fos-like immunoreactivity in the caudal medulla and upper cervical spinal cord following stimulation of the superior sagittal sinus in the cat. Brain Res. 629, 95–102 (1993).
Hoskin, K. L., Zagami, A. S. & Goadsby, P. J. Stimulation of the middle meningeal artery leads to Fos expression in the trigeminocervical nucleus: a comparative study of monkey and cat. J. Anat. 194, 579–588 (1999).
Burstein, R., Yamamura, H., Malick, A. & Strassman, A. M. Chemical stimulation of the intracranial dura induces enhanced responses to facial stimulation in brain stem trigeminal neurons. J. Neurophysiol. 79, 964–982 (1998).
Knight, Y. E. et al. Patterns of fos expression in the rostral medulla and caudal pons evoked by noxious craniovascular stimulation and periaqueductal gray stimulation in the cat. Brain Res. 1045, 1–11 (2005).
Bartsch, T. & Goadsby, P. J. Stimulation of the greater occipital nerve induces increased central excitability of dural afferent input. Brain 125, 1496–1509 (2002).
Bartsch, T. & Goadsby, P. J. Increased responses in trigeminocervical nociceptive neurons to cervical input after stimulation of the dura mater. Brain 126, 1801–1813 (2003).
Bartsch, T. & Goadsby, P. J. Anatomy and physiology of pain referral in primary and cervicogenic headache disorders. Headache Curr. 2, 42–48 (2005).
Liu, Y., Broman, J., Zhang, M. & Edvinsson, L. Brainstem and thalamic projections from a craniovascular sensory nervous centre in the rostral cervical spinal dorsal horn of rats. Cephalalgia 29, 935–948 (2009).
Hoskin, K. L., Bulmer, D. C. E., Lasalandra, M., Jonkman, A. & Goadsby, P. J. Fos expression in the midbrain periaqueductal grey after trigeminovascular stimulation. J. Anat. 198, 29–35 (2001).
Lambert, G. A., Hoskin, K. L. & Zagami, A. S. Cortico-NRM influences on trigeminal neuronal sensation. Cephalalgia 28, 640–652 (2008).
Edelmayer, R. M. et al. Medullary pain facilitating neurons mediate allodynia in headache-related pain. Ann. Neurol. 65, 184–193 (2009).
Burstein, R. & Jakubowski, M. Unitary hypothesis for multiple triggers of the pain and strain of migraine. J. Comp. Neurol. 493, 9–14 (2005).
Malick, A. & Burstein, R. Cells of origin of the trigeminohypothalamic tract in the rat. J. Comp. Neurol. 400, 125–144 (1998).
Malick, A., Strassman, R. M. & Burstein, R. Trigeminohypothalamic and reticulohypothalamic tract neurons in the upper cervical spinal cord and caudal medulla of the rat. J. Neurophysiol. 84, 2078–2112 (2000).
Burstein, R., Cliffer, K. D. & Giesler, G. J. Jr. Direct somatosensory projections from the spinal cord to the hypothalamus and telencephalon. J. Neurosci. 7, 4159–4164 (1987).
Burstein, R., Cliffer, K. D. & Giesler, G. J. Jr. Cells of origin of the spinohypothalamic tract in the rat. J. Comp. Neurol. 291, 329–344 (1990).
Benjamin, L. et al. Hypothalamic activation after stimulation of the superior sagittal sinus in the cat: a Fos study. Neurobiol. Dis. 16, 500–505 (2004).
Malick, A., Jakubowski, M., Elmquist, J. K., Saper, C. B. & Burstein, R. A neurohistochemical blueprint for pain-induced loss of appetite. Proc. Natl Acad. Sci. USA 98, 9930–9935 (2001). This study shows that sensitization of trigeminovascular neurons disrupts feeding in rodents, possibly through activation of hypothalamic neurons. It demonstrates a mechanism by which migraine in patients may alter food intake.
Matsushita, M., Ikeda, M. & Okado, N. The cells of origin of the trigeminothalamic, trigeminospinal and trigeminocerebellar projections in the cat. Neuroscience 7, 1439–1454 (1982).
Shigenaga, Y. et al. The cells of origin of cat trigeminothalamic projections: especially in the caudal medulla. Brain Res. 277, 201–222 (1983).
Williams, M. N., Zahm, D. S. & Jacquin, M. F. Differential foci and synaptic organization of the principal and spinal trigeminal projections to the thalamus in the rat. Eur. J. Neurosci. 6, 429–453 (1994).
Veinante, P., Jacquin, M. F. & Deschenes, M. Thalamic projections from the whisker-sensitive regions of the spinal trigeminal complex in the rat. J. Comp. Neurol. 420, 233–243 (2000).
Zagami, A. S. & Lambert, G. A. Stimulation of cranial vessels excites nociceptive neurones in several thalamic nuclei of the cat. Exp. Brain Res. 81, 552–566 (1990).
Zagami, A. S. & Lambert, G. A. Craniovascular application of capsaicin activates nociceptive thalamic neurones in the cat. Neurosci. Lett. 121, 187–190 (1991).
Burstein, R. et al. Thalamic sensitization transforms localized pain into widespread allodynia. Ann. Neurol. 68, 81–91 (2010).
Jasmin, L., Burkey, A. R., Card, J. P. & Basbaum, A. I. Transneuronal labeling of a nociceptive pathway, the spino-(trigemino-)parabrachio-amygdaloid, in the rat. J. Neurosci. 17, 3751–3765 (1997).
Kunkler, P. E. & Kraig, R. P. Hippocampal spreading depression bilaterally activates the caudal trigeminal nucleus in rodents. Hippocampus 13, 835–844 (2003).
Tracey, I. Imaging pain. Br. J. Anaesth. 101, 32–39 (2008).
Derbyshire, S. W. et al. Pain processing during three levels of noxious stimulation produces differential patterns of central activity. Pain 73, 431–445 (1997).
Burstein, R. & Jakubowski, M. Neural substrate of depression during migraine. Neurol. Sci. 30, S27–S31 (2009).
Afridi, S. K. et al. A PET study exploring the laterality of brainstem activation in migraine using glyceryl trinitrate. Brain 128, 932–939 (2005).
Bahra, A., Matharu, M. S., Buchel, C., Frackowiak, R. S. & Goadsby, P. J. Brainstem activation specific to migraine headache. Lancet 357, 1016–1017 (2001).
May, A., Bahra, A., Buchel, C., Frackowiak, R. S. & Goadsby, P. J. Hypothalamic activation in cluster headache attacks. Lancet 352, 275–278 (1998).
Weiller, C. et al. Brain stem activation in spontaneous human migraine attacks. Nature Med. 1, 658–660 (1995). This was the first demonstration of brainstem activation during a spontaneous migraine attack, and led to the hypothesis of brainstem dysfunction in migraine.
Sprenger, T. & Goadsby, P. J. What has functional neuroimaging done for primary headache.and for the clinical neurologist? J. Clin. Neurosci. 17, 547–553 (2010).
Stephan, K. E. & Friston, K. J. Analyzing effective connectivity with fMRI. Wiley Interdiscip. Rev. Cogn. Sci. 1, 446–459 (2010).
Sprenger, T. et al. Abnormal interictal large-scale brain network connectivity in episodic migraine. Headache 50, 71 (2010).
Mainero, C., Boshyan, J. & Hadjikhani, N. Altered functional MRI resting-state connectivity in periaqueductal gray networks in migraine. Ann. Neurol. 11 Jul 2011 (doi:10.1002/ana.22537).
Percheron, G. Thalamus. in The Human Nervous System (eds Paxinos, G. & May, J.) 592–675 (Elsevier, Amsterdam, 2003).
Denuelle, M., Fabre, N., Payoux, P., Chollet, F. & Geraud, G. Hypothalamic activation in spontaneous migraine attacks. Headache 47, 1418–1426 (2007). Together with reference 55, this was the first demonstration of hypothalamic activation during cluster headache and migraine, respectively. The studies put forward the argument that central changes may be responsible for the pain, vascular and autonomic symptoms that occur in cluster headache and migraine, and emphasize the importance of the brain in these headache disorders
Afridi, S. K. et al. A positron emission tomographic study in spontaneous migraine. Arch. Neurol. 62, 1270–1275 (2005).
Fields, H. L. Is there is a facilitating component to central modulation of pain? J. Pain 1, 71–78 (1992).
Young, R. F. & Brechner, T. Electrical stimulation of the brain for relief of intractable pain due to cancer. Cancer 57, 1266–1272 (1986).
Mayer, D. J. Analgesia produced by electrical stimulation of the brain. Prog. Neuropsychopharmacol. Biol. Psychiatry 8, 557–564 (1984).
Sandkuhler, J. & Gebhart, G. F. Relative contributions of the nucleus raphe magnus and adjacent medullary reticular formation to the inhibition by stimulation in the periaqueductal gray of a spinal nociceptive reflex in the pentobarbital-anesthetized rat. Brain Res. 305, 77–87 (1984).
Fields, H. L., Basbaum, A. I., Clanton, C. H. & Anderson, S. D. Nucleus raphe magnus inhibition of spinal cord dorsal horn neurons. Brain Res. 126, 441–453 (1977).
Porreca, F., Ossipov, M. H. & Gebhart, G. F. Chronic pain and medullary descending facilitation. Trends Neurosci. 25, 319–325 (2002).
Bartsch, T., Knight, Y. E. & Goadsby, P. J. Activation of 5-HT(1B/1D) receptor in the periaqueductal gray inhibits nociception. Ann. Neurol. 56, 371–381 (2004). The authors showed that triptans that are targeted to the vlPAG can attenuate dural-evoked nociceptive trigeminovascular neurons — the first clear indication that triptans can act in areas other than the TNC to exert their therapeutic affects.
Spencer, S. E., Sawyer, W. B., Wada, H., Platt, K. B. & Loewy, A. D. CNS projections to the pterygopalatine parasympathetic preganglionic neurons in the rat: a retrograde transneuronal viral cell body labeling study. Brain Res. 534, 149–169 (1990).
Lai, T.-H., Fuh, J.-L. & Wang, S.-J. Cranial autonomic symptoms in migraine: characteristics and comparison with cluster headache. J. Neurol. Neurosurg. Psychiatry 80, 1116–1119 (2009).
Goadsby, P. J. Pathophysiology of cluster headache: a trigeminal autonomic cephalalgia. Lancet Neurol. 1, 251–257 (2002).
Akerman, S., Holland, P. R., Lasalandra, M. P. & Goadsby, P. J. Oxygen inhibits neuronal activation in the trigeminocervical complex after stimulation of trigeminal autonomic reflex, but not during direct dural activation of trigeminal afferents. Headache 49, 1131–1143 (2009). This is the first study to show a mechanism of action for the therapeutic effects of oxygen in cluster headache, and a lack of therapeutic effect in migraine. There is also a clear demonstration that SuS stimulation can cause activation in the medullary and cervical dorsal horn.
Okamoto, K., Tashiro, A., Chang, Z. & Bereiter, D. A. Bright light activates a trigeminal nociceptive pathway. Pain 149, 235–242 (2010).
Goadsby, P. J. Sphenopalatine ganglion stimulation increases regional cerebral blood flow independent of glucose utilization in the cat. Brain Res. 506, 145–148 (1990).
Goadsby, P. J. Effect of stimulation of facial nerve on regional cerebral blood flow and glucose utilization in cats. Am. J. Physiol. 257, R517–R521 (1989).
Goadsby, P. J. & MacDonald, G. J. Extracranial vasodilation mediated by vasoactive intestinal polypeptide (VIP). Brain Res. 329, 285–288 (1985).
Goadsby, P. J. & Edvinsson, L. Human in vivo evidence for trigeminovascular activation in cluster headache. Neuropeptide changes and effects of acute attacks therapies. Brain 117, 427–434 (1994).
Goadsby, P. J. & Edvinsson, L. Neuropeptide changes in a case of chronic paroxysmal hemicrania-evidence for trigemino-parasympathetic activation. Cephalalgia 16, 448–450 (1996).
Hosoya, Y., Matsushita, M. & Sugiura, Y. A direct hypothalamic projection to the superior salivatory nucleus neurons in the rat. A study using anterograde autoradiographic and retrograde HRP methods. Brain Res. 266, 329–333 (1983).
Hosoya, Y., Sugiura, Y., Ito, R. & Kohno, K. Descending projections from the hypothalamic paraventricular nucleus to the A5 area, including the superior salivatory nucleus, in the rat. Exp. Brain Res. 82, 513–518 (1990).
Knight, Y. E. & Goadsby, P. J. The periaqueductal grey matter modulates trigeminovascular input: a role in migraine? Neuroscience 106, 793–800 (2001).
Knight, Y. E., Bartsch, T. & Goadsby, P. J. Trigeminal antinociception induced by bicuculline in the periaqueductal gray (PAG) is not affected by PAG P/Q-type calcium channel blockade in rat. Neurosci. Lett. 336, 113–116 (2003).
Knight, Y. E., Bartsch, T., Kaube, H. & Goadsby, P. J. P/Q-type calcium-channel blockade in the periaqueductal gray facilitates trigeminal nociception: a functional genetic link for migraine? J. Neurosci. 22, RC213 (2002). References 83–85 were the first studies to demonstrate that manipulation of P/Q-type calcium channels in the vlPAG have a descending modulatory effect on dural-evoked nociceptive trigeminovascular neurons — with implications for brainstem involvement in pathophysiology of migraine and familial hemiplegic migraine.
Ophoff, R. A. et al. Familial hemiplegic migraine and episodic ataxia type-2 are caused by mutations in the Ca2+ channel gene CACNL1A4. Cell 87, 543–552 (1996).
Basbaum, A. I., Clanton, C. H. & Fields, H. L. Three bulbospinal pathways from the rostral medulla of the cat: an autoradiographic study of pain modulating systems. J. Comp. Neurol. 178, 209–224 (1978).
Holstege, G. & Kuypers, H. G. The anatomy of brain stem pathways to the spinal cord in cat. A labeled amino acid tracing study. Prog. Brain Res. 57, 145–175 (1982).
Fields, H. L., Vanegas, H., Hentall, I. D. & Zorman, G. Evidence that disinhibition of brain stem neurones contributes to morphine analgesia. Nature 306, 684–686 (1983).
Mason, P. Deconstructing endogenous pain modulations. J. Neurophysiol. 94, 1659–1663 (2005).
Fields, H. L., Bry, J., Hentall, I. & Zorman, G. The activity of neurons in the rostral medulla of the rat during withdrawal from noxious heat. J. Neurosci. 3, 2545–2552 (1983).
Gao, K. & Mason, P. Physiological and anatomic evidence for functional subclasses of serotonergic raphe magnus cells. J. Comp. Neurol. 439, 426–439 (2001).
Gao, K. & Mason, P. Serotonergic Raphe magnus cells that respond to noxious tail heat are not ON or OFF cells. J. Neurophysiol. 84, 1719–1725 (2000).
Mason, P. Physiological identification of pontomedullary serotonergic neurons in the rat. J. Neurophysiol. 77, 1087–1098 (1997).
Fields, H. L., Heinricher, M. M. & Mason, P. Neurotransmitters in nociceptive modulatory circuits. Annu. Rev. Neurosci. 14, 219–245 (1991).
Fields, H. L. & Heinricher, M. M. Anatomy and physiology of a nociceptive modulatory system. Philos. Trans. R. Soc. Lond. B 308, 361–374 (1985).
Ellrich, J., Ulucan, C. & Schnell, C. Are 'neutral cells' in the rostral ventro-medial medulla subtypes of on- and off-cells? Neurosci. Res. 38, 419–423 (2000).
Mason, P. Ventromedial medulla: pain modulation and beyond. J. Comp. Neurol. 493, 2–8 (2005).
Leung, C. G. & Mason, P. Physiological properties of raphe magnus neurons during sleep and waking. J. Neurophysiol. 81, 584–595 (1999).
Foo, H. & Mason, P. Movement-related discharge of ventromedial medullary neurons. J. Neurophysiol. 93, 873–883 (2005).
Foo, H. & Mason, P. Discharge of raphe magnus ON and OFF cells is predictive of the motor facilitation evoked by repeated laser stimulation. J. Neurosci. 23, 1933–1940 (2003).
Foo, H. & Mason, P. Sensory suppression during feeding. Proc. Natl Acad. Sci. USA 102, 16865–16869 (2005).
Baez, M. A., Brink, T. S. & Mason, P. Roles for pain modulatory cells during micturition and continence. J. Neurosci. 25, 384–394 (2005).
Foo, H. & Mason, P. Brainstem modulation of pain during sleep and waking. Sleep Med. Rev. 7, 145–154 (2003).
Foo, H., Crabtree, K. & Mason, P. The modulatory effects of rostral ventromedial medulla on air-puff evoked microarousals in rats. Behav. Brain Res. 215, 156–159 (2010).
Vera-Portocarrero, L. P., Ossipov, M. H., King, T. & Porreca, F. Reversal of inflammatory and noninflammatory visceral pain by central or peripheral actions of sumatriptan. Gastroenterology 135, 1369–1378 (2008).
Holland, P. R., Akerman, S., Lasalandra, M. P. & Goadsby, P. J. Antinociceptive effects of orexin A in the vlPAG are blocked by 5-HT1B/1D receptor antagonism. Headache 48, S1–S67 (2008).
Akerman, S., Holland, P. R., Lasalandra, M. P. & Goadsby, P. J. Activation of the CB1 receptor in the vlPAG inhibits nociceptive dural inputs in the TCC via neurons that are modulated by the 5-HT1B/1D receptor. Headache 48, S1–S67 (2008).
Bigal, M. E. et al. Acute migraine medications and evolution from episodic to chronic migraine: a longitudinal population-based study. Headache 48, 1157–1168 (2008).
Hilairet, S., Bouaboula, M., Carriere, D., Le Fur, G. & Casellas, P. Hypersensitization of the Orexin 1 receptor by the CB1 receptor: evidence for cross-talk blocked by the specific CB1 antagonist, SR141716. J. Biol. Chem. 278, 23731–23737 (2003).
Ellis, J., Pediani, J. D., Canals, M., Milasta, S. & Milligan, G. Orexin-1 receptor-cannabinoid CB1 receptor heterodimerization results in both ligand-dependent and -independent coordinated alterations of receptor localization and function. J. Biol. Chem. 281, 38812–38824 (2006).
Finn, D. P. et al. Effects of direct periaqueductal grey administration of a cannabinoid receptor agonist on nociceptive and aversive responses in rats. Neuropharmacology 45, 594–604 (2003).
Martin, W. J., Tsou, K. & Walker, J. M. Cannabinoid receptor-mediated inhibition of the rat tail-flick reflex after microinjection into the rostral ventromedial medulla. Neurosci. Lett. 242, 33–36 (1998).
Meng, I. D., Manning, B. H., Martin, W. J. & Fields, H. L. An analgesia circuit activated by cannabinoids. Nature 395, 381–383 (1998).
Meng, I. D. & Johansen, J. P. Antinociception and modulation of rostral ventromedial medulla neuronal activity by local microinfusion of a cannabinoid receptor agonist. Neuroscience 124, 685–693 (2004).
Vaughan, C. W., Connor, M., Bagley, E. E. & Christie, M. J. Actions of cannabinoids on membrane properties and synaptic transmission in rat periaqueductal gray neurons in vitro. Mol. Pharmacol. 57, 288–295 (2000).
Moreau, J. L. & Fields, H. L. Evidence for GABA involvement in midbrain control of medullary neurons that modulate nociceptive transmission. Brain Res. 397, 37–46 (1986).
Goadsby, P. J., Cittadini, E. & Cohen, A. S. Trigeminal autonomic cephalalgias: paroxysmal hemicrania, SUNCT/SUNA and hemicrania continua. Semin. Neurol. 30, 186–191 (2010).
Panda, S. & Hogenesch, J. B. It's all in the timing: many clocks, many outputs. J. Biol. Rhythms 19, 374–387 (2004).
Settle, M. The hypothalamus. Neonatal Netw. 19, 9–14 (2000).
Goder, R. et al. Polysomnographic findings in nights preceding a migraine attack. Cephalalgia 21, 31–37 (2001).
Dalkvist, J., Ekbom, K. & Waldenlind, E. Headache and mood: a time-series analysis of self-ratings. Cephalalgia 4, 45–52 (1984).
Giffin, N. J. et al. Premonitory symptoms in migraine: an electronic diary study. Neurology 60, 935–940 (2003).
Fleetwood-Walker, S. M., Hope, P. J. & Mitchell, R. Antinociceptive actions of descending dopaminergic tracts on cat and rat dorsal horn somatosensory neurones. J. Physiol. 399, 335–348 (1988).
Holland, P. & Goadsby, P. J. The hypothalamic orexinergic system: pain and primary headaches. Headache 47, 951–962 (2007).
Bartsch, T., Levy, M. J., Knight, Y. E. & Goadsby, P. J. Differential modulation of nociceptive dural input to [hypocretin] orexin A and B receptor activation in the posterior hypothalamic area. Pain 109, 367–378 (2004).
Bartsch, T., Levy, M. J., Knight, Y. E. & Goadsby, P. J. Inhibition of nociceptive dural input in the trigeminal nucleus caudalis by somatostatin receptor blockade in the posterior hypothalamus. Pain 117, 30–39 (2005).
Matharu, M. S., Levy, M. J., Meeran, K. & Goadsby, P. J. Subcutaneous octreotide in cluster headache: randomized placebo-controlled double-blind crossover study. Ann. Neurol. 56, 488–494 (2004).
Levy, M. J., Matharu, M. S., Bhola, R., Meeran, K. & Goadsby, P. J. Octreotide is not effective in the acute treatment of migraine. Cephalalgia 25, 48–55 (2005).
Strassman, A. M., Raymond, S. A. & Burstein, R. Sensitization of meningeal sensory neurons and the origin of headaches. Nature 384, 560–564 (1996).
Dahlstrom, A. & Fuxe, K. Evidence for existence of monoamine-containing neurons in central nervous system. I. Demonstration of monoamines in cell bodies of brain stem neurons. Acta Physiol.Scand, Suppl. 232, 1–55 (1964).
Skagerberg, G., Bjorklund, A., Lindvall, O. & Schmidt, R. H. Origin and termination of the diencephalo-spinal dopamine system in the rat. Brain Res. Bull. 9, 237–244 (1982).
Holstege, J. C. et al. Distribution of dopamine immunoreactivity in the rat, cat and monkey spinal cord. J. Comp. Neurol. 376, 631–652 (1996).
Bergerot, A., Storer, R. J. & Goadsby, P. J. Dopamine inhibits trigeminovascular transmission in the rat. Ann. Neurol. 61, 251–262 (2007).
Charbit, A. R., Akerman, S., Holland, P. R. & Goadsby, P. J. Neurons of the dopaminergic/calcitonin gene-related peptide A11 cell group modulate neuronal firing in the trigeminocervical complex: an electrophysiological and immunohistochemical study. J. Neurosci. 29, 12532–12541 (2009). This was that first study to introduce the A11 dopaminergic nucleus into migraine pathophysiology. Stimulation of the A11 can inhibit dural-evoked nociceptive trigeminovascular neurons, whereas lesioning the nucleus facilitates the dural and facial nociceptive responses. It implicates the A11 in the hypothesis that diencephalic dysfunction could contribute to migraine pathophysiology.
Clemens, S., Rye, D. & Hochman, S. Restless legs syndrome: revisiting the dopamine hypothesis from the spinal cord perspective. Neurology 67, 125–130 (2006).
Ondo, W. G., He, Y., Rajasekaran, S. & Le, W. D. Clinical correlates of 6-hydroxydopamine injections into A11 dopaminergic neurons in rats: a possible model for restless legs syndrome. Mov. Disord. 15, 154–158 (2000).
Burstein, R., Yarnitsky, D., Goor-Aryeh, I., Ransil, B. J. & Bajwa, Z. H. An association between migraine and cutaneous allodynia. Ann. Neurol. 47, 614–624 (2000). In references 138 and 47, the authors show that nearly 80% of patients experience cutaneous allodynia during migraine attack. By studying patients during migraine attack and animal models of central sensitization, the authors show that allodynia probably occurs through sensitization of third-order trigeminovascular neurons at the level of the thalamus.
Shields, K. G. & Goadsby, P. J. Propranolol modulates trigeminovascular responses in thalamic ventroposteromedial nucleus: a role in migraine? Brain 128, 86–97 (2005).
Andreou, A. P., Shields, K. G. & Goadsby, P. J. GABA and valproate modulate trigeminovascular nociceptive transmission in the thalamus. Neurobiol. Dis. 37, 314–323 (2010).
Summ, O., Charbit, A. R., Andreou, A. P. & Goadsby, P. J. Modulation of nocioceptive transmission with calcitonin gene-related peptide receptor antagonists in the thalamus. Brain 133, 2540–2548 (2010).
Shields, K. G. & Goadsby, P. J. Serotonin receptors modulate trigeminovascular responses in ventroposteromedial nucleus of thalamus: a migraine target? Neurobiol. Dis. 23, 491–501 (2006).
Andreou, A. P. & Goadsby, P. J. Therapeutic potential of novel glutamate receptor antagonists in migraine. Expert Opin. Investig. Drugs 18, 789–803 (2009).
Noseda, R. et al. A neural mechanism for exacerbation of headache by light. Nature Neurosci. 13, 239–245 (2010). References 75 and 144 show a neural mechanism for the photophobia that is experienced during migraine. Reference 75 provides a direct link between light intensity and activation of the TNC. Reference 144 shows that dura-sensitive nociceptive trigeminovascular neuronal responses in the posterior thalamus are exacerbated by increasing light intensity, and that they project to the sensory and visual cortices.
Neugebauer, V. & Li, W. Processing of nociceptive mechanical and thermal information in central amygdala neurons with knee-joint input. J. Neurophysiol. 87, 103–112 (2002).
Hotopf, M., Mayou, R., Wadsworth, M. & Wessely, S. Temporal relationships between physical symptoms and psychiatric disorder. Results from a national birth cohort. Br. J. Psychiatry 173, 255–261 (1998).
Lazarov, N. E. et al. Amygdalotrigeminal projection in the rat: an anterograde tracing study. Ann. Anat. 193, 118–126 (2011).
Dehbandi, S., Speckmann, E. J., Pape, H. C. & Gorji, A. Cortical spreading depression modulates synaptic transmission of the rat lateral amygdala. Eur. J. Neurosci. 27, 2057–2065 (2008).
Sink, K. S., Walker, D. L., Yang, Y. & Davis, M. Calcitonin gene-related peptide in the bed nucleus of the stria terminalis produces an anxiety-like pattern of behavior and increases neural activation in anxiety-related structures. J. Neurosci. 31, 1802–1810 (2011).
Calandre, E. P., Bembibre, J., Arnedo, M. L. & Becerra, D. Cognitive disturbances and regional cerebral blood flow abnormalities in migraine patients: their relationship with the clinical manifestations of the illness. Cephalalgia 22, 291–302 (2002).
Valfre, W., Rainero, I., Bergui, M. & Pinessi, L. Voxel-based morphometry reveals gray matter abnormalities in migraine. Headache 48, 109–117 (2008).
Kim, J. H. et al. Regional grey matter changes in patients with migraine: a voxel-based morphometry study. Cephalalgia 28, 598–604 (2008).
Tessitore, A. et al. Interictal cortical reorganization in episodic migraine without aura: an event-related fMRI study during parametric trigeminal nociceptive stimulation. Neurol. Sci. 32, S165–S167 (2011).
Peroutka, S. J. Neurogenic inflammation and migraine: implications for the therapeutics. Mol. Interv. 5, 304–311 (2005).
Moulton, E. A. et al. Interictal dysfunction of a brainstem descending modulatory center in migraine patients. PLoS ONE 3, e3799 (2008).
Stankewitz, A., Aderjan, D., Eippert, F. & May, A. Trigeminal nociceptive transmission in migraineurs predicts migraine attacks. J. Neurosci. 31, 1937–1943 (2011).
Stankewitz, A. & May, A. The phenomenon of changes in cortical excitability in migraine is not migraine-specific—a unifying thesis. Pain 145, 14–17 (2009).
Uddman, R. & Edvinsson, L. Neuropeptides in the cerebral circulation. Cerebrovasc. Brain Metab. Rev. 1, 230–252 (1989).
Goadsby, P. J., Edvinsson, L. & Ekman, R. Release of vasoactive peptides in the extracerebral circulation of humans and the cat during activation of the trigeminovascular system. Ann. Neurol. 23, 193–196 (1988).
Goadsby, P. J. & Duckworth, J. W. Effect of stimulation of trigeminal ganglion on regional cerebral blood flow in cats. Am. J. Physiol. 253, R270–R274 (1987).
Tran-Dinh, Y. R., Thurel, C., Cunin, G., Serrie, A. & Seylaz, J. Cerebral vasodilation after the thermocoagulation of the trigeminal ganglion in humans. Neurosurgery 31, 658–662 (1992).
Goadsby, P. J., Knight, Y. E., Hoskin, K. L. & Butler, P. Stimulation of an intracranial trigeminally-innervated structure selectively increases cerebral blood flow. Brain Res. 751, 247–252 (1997).
Zagami, A. S., Goadsby, P. J. & Edvinsson, L. Stimulation of the superior sagittal sinus in the cat causes release of vasoactive peptides. Neuropeptides 16, 69–75 (1990).
Goadsby, P. J., Edvinsson, L. & Ekman, R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann. Neurol. 28, 183–187 (1990).
Gallai, V. et al. Vasoactive peptide levels in the plasma of young migraine patients with and without aura assessed both interictally and ictally. Cephalalgia 15, 384–390 (1995).
Fanciullacci, M., Alessandri, M., Figini, M., Geppetti, P. & Michelacci, S. Increase in plasma calcitonin gene-related peptide from the extracerebral circulation during nitroglycerin-induced cluster headache attack. Pain 60, 119–123 (1995).
Knight, Y. E., Edvinsson, L. & Goadsby, P. J. Blockade of calcitonin gene-related peptide release after superior sagittal sinus stimulation in cat: a comparison of avitriptan and CP122,288. Neuropeptides 33, 41–46 (1999).
Knight, Y. E., Edvinsson, L. & Goadsby, P. J. 4991W93 inhibits release of calcitonin gene-related peptide in the cat but only at doses with 5HT(1B/1D) receptor agonist activity? Neuropharmacology 40, 520–525 (2001).
Roon, K. I. et al. No acute antimigraine efficacy of CP-122288, a highly potent inhibitor of neurogenic inflammation: results of two randomized, double-blind, placebo-controlled clinical trials. Ann. Neurol. 47, 238–241 (2000).
Earl, N. L., McDonald, S. A. & Lowry, M. T. Efficacy and tolerability of the neurogenic inflammation inhibitor, 4991W93 in the acute treatment of migraine. Cephalalgia 19, 357 (1999).
Doods, H. et al. Pharmacological profile of BIBN4096BS, the first selective small molecule CGRP antagonist. Br. J. Pharmacol. 129, 420–423 (2000).
Olesen, J. et al. Calcitonin gene-related peptide receptor antagonist BIBN 4096 BS for the acute treatment of migraine. N. Engl. J. Med. 350, 1104–1110 (2004). This proof of concept clinical study demonstrated that CGRP receptor antagonists were efficacious in the acute treatment of migraine without cardiovascular implication, and may represent a new class of compound for patients who suffer from migraine.
Ho, T. W. et al. Randomized controlled trial of an oral CGRP receptor antagonist, MK-0974, in acute treatment of migraine. Neurology 70, 1304–1312 (2008).
Connor, K. M. et al. Randomized, controlled trial of telcagepant for the acute treatment of migraine. Neurology 73, 970–977 (2009).
Hewitt, D. J. et al. Randomized controlled trial of the CGRP receptor antagonist, MK-3207, in the acute treatment of migraine. Cephalalgia 31, 712–722 (2011).
Diener, H.-C. et al. BI 44370 TA, an oral CGRP antagonist for the acute treatment of migraine attacks: results from a phase II study. Cephalalgia 31, 573–584 (2011).
Rasmussen, B. K. & Olesen, J. Migraine with aura and migraine without aura: an epidemiological study. Cephalalgia 12, 221–228 (1992).
Olesen, J. Cerebral and extracranial circulatory disturbances in migraine: pathophysiological implications. Cerebrovasc. Brain Metab. Rev. 3, 1–28 (1991).
Cutrer, F. M. et al. Perfusion-weighted imaging defects during spontaneous migrainous aura. Ann. Neurol. 43, 25–31 (1998).
Hadjikhani, N. et al. Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proc. Natl Acad. Sci. USA 98, 4687–4692 (2001). The clearest demonstration so far of cortical signal changes that are consistent with CSD during migraine aura.
Sanchez del Rio, M. et al. Perfusion weighted imaging during migraine: spontaneous visual aura and headache. Cephalalgia 19, 701–707 (1999).
Lauritzen, M. Pathophysiology of the migraine aura. The spreading depression theory. Brain 117, 199–210 (1994).
Leao, A. A. P. Spreading depression of activity in cerebral cortex. J. Neurophysiol. 7, 359–390 (1944).
Brennan, K. C. et al. Distinct vascular conduction with cortical spreading depression. J. Neurophysiol. 97, 4143–4151 (2007).
Bolay, H. et al. Intrinsic brain activity triggers trigeminal meningeal afferents in a migraine model. Nature Med. 8, 136–142 (2002).
Zhang, X. et al. Activation of meningeal nociceptors by cortical spreading depression: implications for migraine with aura. J. Neurosci. 30, 8807–8814 (2010).
Zhang, X. et al. Activation of central trigeminovascular neurons by cortical spreading depression. Ann. Neurol. 69, 855–865 (2011).
Moskowitz, M. A., Bolay, H. & Dalkara, T. Deciphering migraine mechanisms: clues from familial hemiplegic migraine genotypes. Ann. Neurol. 55, 276–280 (2004).
Haerter, K., Ayata, C. & Moskowitz, M. A. Cortical spreading depression: a model for understanding migraine biology and future drug targets. Headache Curr. 2, 97–103 (2005).
Ebersberger, A., Schaible, H.-G., Averbeck, B. & Richter, F. Is there a correlation between spreading depression, neurogenic inflammation, and nociception that might cause migraine headache? Ann. Neurol. 41, 7–13 (2001).
Lambert, G. A., Michalicek, J., Storer, R. J. & Zagami, A. S. Effect of cortical spreading depression on activity of trigeminovascular sensory neurons. Cephalalgia 19, 631–638 (1999).
Piper, R. D., Lambert, G. A. & Duckworth, J. W. Cortical blood flow changes during spreading depression in cats. Am. J. Physiol. 261, H96–H102 (1991).
Goadsby, P. J., Seylaz, J. & Mraovitch, S. in Migraine and other headaches: the vascular mechanisms (ed. Olesen, J.) 181–6 (Raven Press, New York, 1991)
Yokota, C. et al. Unique profile of spreading depression in a primate model. J. Cereb. Blood Flow Metab. 22, 835–842 (2002).
Mayevsky, A. et al. Cortical spreading depression recorded from the human brain using a multiparametric monitoring system. Brain Res. 740, 268–274 (1996).
Strong, A. J. et al. Spreading and synchronous depressions of cortical activity in acutely injured human brain. Stroke 33, 2738–2743 (2002).
Fabricius, M. et al. Cortical spreading depression and peri-infarct depolarization in acutely injured human cerebral cortex. Brain 129, 778–790 (2006).
Moncada, S., Palmer, R. M. & Higgs, E. A. Nitric oxide: physiology, pathophysiology, and pharmacology. Pharmacol. Rev. 43, 109–142 (1991).
Lassen, L. H. et al. CGRP may play a causative role in migraine. Cephalalgia 22, 54–61 (2002).
Schytz, H. W. et al. PACAP38 induces migraine-like attacks in patients with migraine without aura. Brain 132, 16–25 (2009).
Wienecke, T., Olesen, J. & Ashina, M. Prostaglandin I2 (epoprostenol) triggers migraine-like attacks in migraineurs. Cephalalgia 30, 179–190 (2010).
Iversen, H. K., Olesen, J. & Tfelt-hansen, P. Intravenous nitroglycerin as an experimental-model of vascular headache — basic characteristics. Pain 38, 17–24 (1989).
Olesen, J., Iversen, H. K. & Thomsen, L. L. Nitric oxide supersensitivity: a possible molecular mechanism of migraine pain. Neuroreport 4, 1027–1030 (1993).
Olesen, J., Thomsen, L. L. & Iversen, H. Nitric oxide is a key molecule in migraine and other vascular headaches. Trends Pharmacol. Sci. 15, 149–153 (1994).
Olesen, J., Thomsen, L. L., Lassen, L. H. & Olesen, I. J. The nitric oxide hypothesis of migraine and other vascular headaches. Cephalalgia 15, 94–100 (1995).
Asghar, M. S. et al. Dilation by CGRP of middle meningeal artery and reversal by sumatriptan in normal volunteers. Neurology 75, 1520–1526 (2010).
Iversen, H. K. & Olesen, J. Headache induced by a nitric oxide donor (nitroglycerin) responds to sumatriptan. A human model for development of migraine drugs. Cephalalgia 16, 412–418 (1996).
Akerman, S., Williamson, D. J., Kaube, H. & Goadsby, P. J. The effect of anti-migraine compounds on nitric oxide-induced dilation of dural meningeal vessels. Eur. J. Pharmacol. 452, 223–228 (2002).
Humphrey, P. P., Feniuk, W. Mode of action of the anti-migraine drug sumatriptan. Trends Pharmacol. Sci. 12, 444–446 (1991).
Schoonman, G. G. et al. Migraine headache is not associated with cerebral or meningeal vasodilatation-a 3T magnetic resonance angiography study. Brain 131, 2192–2200 (2008). References 206 and 210 are two studies that show the complexity of the arguments over whether vascular changes are a necessary factor in the pain in migraine. Reference 210 was able to demonstrate migraine headache without meningeal or cerebral changes, whereas reference 206 shows migraine headache with substantial meningeal and cerebral vessel dilation.
Asghar, M. S. et al. Evidence for a vascular factor in migraine. Ann. Neurol. 69, 635–645 (2011).
Hoskin, K. L., Kaube, H. & Goadsby, P. J. Sumatriptan can inhibit trigeminal afferents by an exclusively neural mechanism. Brain 119, 1419–1428 (1996). This study showed that sumatriptan can have an action that is exclusively neural and not at the level of the vasculature, and was the first indication that drugs without actions at the vasculature may be therapeutic in migraine.
Rahmann, A. et al. Vasoactive intestinal peptide causes marked cephalic vasodilation, but does not induce migraine. Cephalalgia 28, 226–236 (2008).
Tassorelli, C. & Joseph, S. A. Systemic nitroglycerin induces fos immunoreactivity in brain-stem and forebrain structures of the rat. Brain Res. 682, 167–181 (1995).
Lambert, G. A., Donaldson, C., Boers, P. M. & Zagami, A. S. Activation of trigeminovascular neurons by glyceryl trinitrate. Brain Res. 887, 203–210 (2000).
Petersen, K. A., Nilsson, E., Olesen, J. & Edvinsson, L. Presence and function of the calcitonin gene-related peptide receptor on rat pial arteries investigated in vitro and in vivo. Cephalalgia 25, 424–432 (2005).
Storer, R. J., Akerman, S. & Goadsby, P. J. Calcitonin gene-related peptide (CGRP) modulates nociceptive trigeminovascular transmission in the cat. Br. J. Pharmacol. 142, 1171–1181 (2004).
Cumberbatch, M. J., Williamson, D. J., Mason, G. S., Hill, R. G. & Hargreaves, R. J. Dural vasodilation causes a sensitization of rat caudal trigeminal neurones in vivo that is blocked by a 5-HT1B/1D agonist. Br. J. Pharmacol. 126, 1478–1486 (1999).
Paxinos, G. & Watson, C. The Rat Brain In Stereotaxic Coordinates (Elsevier Academic Press, London, 2005).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
P.J.G. is a paid member of the boards of the following companies: Allergan, Colucid, MAP Pharmaceuticals, Merck Sharpe and Dohme (MSD), Neuralieve, Neuraxon, ATI (Autonomic Technologies Incorporated), Boston Scientific, Coherex, Eli-Lilly, Medtronic, Linde gases and Bristol Myers Squibb (BMS). In addition, he is a paid consultant for Pfizer and Air Products and has provided paid expert testimony for MedicoLegal advice. The institution at which P.J.G. works receives grant funding from GlaxoSmithKline, MAP, MSD, Neuralieve, Boston Scientific and Amgen. P.J.G. has also received payment for lectures from MSD, Pfizer, Allergan and Mennarini, and has been paid to provide educational slides to the American Headache Society.
Glossary
- Aura
-
Fully reversible neurological symptoms that typically occur before a migraine and that move from one part of a limb, or of the body, to another. These symptoms can include homonymous visual symptoms (that is, flickering lights, spots or lines, or complete loss of vision), sensory symptoms (that is, pins and needles, or numbness) and dysphasic speech.
- Brainstem
-
The most posterior (stem-like) part of the brain, adjoining the cerebral hemispheres. The brainstem is structurally continuous with the spinal cord and comprises the pons, medulla oblongata and midbrain.
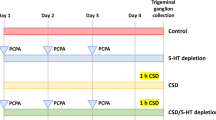
- Cortical spreading depression
-
(CSD). A slowly propagating wave (2–6 mm min−1) of sustained strong neuronal depolarization that generates transient and intense spike activity, followed by neural suppression that can last for several minutes.
- Trigeminocervical complex
-
(TCC). A group of spinal cord regions that include the trigeminal nucleus caudalis in the cervicomedullary junction and the superficial layers of the high cervical region dorsal horn at the C1 and C2 level of the spinal cord.
- Quintothalamic tract
-
Also known as the trigeminothalamic tract. The tract that carries sensory information from the head and face to the thalamus through the trigeminal nucleus.
- Positron emission tomography
-
(PET). A nuclear imaging technique that produces three-dimensional images of the brain by detecting photons that are emitted by a positron-emitting radionuclide tracer.
- Midbrain
-
Also known as the mesencephalon. The region that is situated between the pons and the diencephalon, and that includes the periaqueductal grey (PAG).
- Hyperaemia
-
Also known as hyperperfusion. An increase in blood flow.
- Oligaemia
-
Also known as hypoperfusion. A decrease in blood flow.
- Diencephalic structures
-
Structures of the diencephalon, which is the posterior part of the brain. The diencephalon is anterior to the brainstem and includes the hypothalamus, thalamus, metathalamus and epithalamus.
- Trigeminal autonomic cephalalgias
-
(TACs). Primary headache disorders that are characterized by unilateral head pain occurring in association with ipsilateral cranial autonomic features. There are three major pathophysiological features: trigeminal distribution of pain, cranial autonomic features and an episodic pattern of attacks.
- Central sensitization
-
An enhanced response of central neurons by activation of peripheral nociceptors.
- Allodynia
-
The perception of pain from a stimulus that is normally considered innocuous or a stimulus that does not normally produce pain.
- Referred pain
-
In the context of headache, referred pain is the area of the head where spontaneous pain is felt; in a literal sense it is pain in a location other than the site of stimulus. In the case of migraine, the stimulus is likely to be either central or at the very least intracranial, whereas the pain is perceived in the extracranial region.
Rights and permissions
About this article
Cite this article
Akerman, S., Holland, P. & Goadsby, P. Diencephalic and brainstem mechanisms in migraine. Nat Rev Neurosci 12, 570–584 (2011). https://doi.org/10.1038/nrn3057
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrn3057
This article is cited by
-
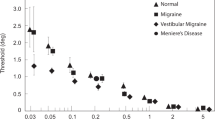
Subjective and objective responses to caloric stimulation help separate vestibular migraine from other vestibular disorders
Journal of Neurology (2024)
-
Imaging the brain and vascular reactions to headache treatments: a systematic review
The Journal of Headache and Pain (2023)
-
Genetics of migraine: where are we now?
The Journal of Headache and Pain (2023)
-
Activation of CB1R alleviates central sensitization by regulating HCN2-pNR2B signaling in a chronic migraine rat model
The Journal of Headache and Pain (2023)
-
Increased iron deposition in nucleus accumbens associated with disease progression and chronicity in migraine
BMC Medicine (2023)