Abstract
Immunological memory is considered to be one of the cardinal features of the adaptive immune system. Despite being a recognized phenomenon since the time of the ancient Greeks, immunologists are yet to fully appreciate the mechanisms that control memory responses in the immune system. Furthermore, our definition of immunological memory itself continues to evolve, with recent suggestions that innate immune cells also show memory-like behaviour. In this Viewpoint article, Nature Reviews Immunology invites five leading immunologists to share their thoughts on our current understanding of the nature of immunological memory. Our experts highlight some of the seminal studies that have shaped the immune memory field and offer contrasting views on the key questions that remain to be addressed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Zinkernagel, R. M. On differences between immunity and immunological memory. Curr. Opin. Immunol. 14, 523–536 (2002).
Ahmed, R. & Gray, D. Immunological memory and protective immunity: understanding their relation. Science 272, 54–60 (1996).
Rajewsky, K. Clonal selection and learning in the antibody system. Nature 381, 751–758 (1996).
Roost, H. P. et al. Early high-affinity neutralizing anti-viral IgG responses without further overall improvements of affinity. Proc. Natl Acad. Sci. USA 92, 1257–1261 (1995).
Gupta, S. C., Hengartner, H. & Zinkernagel, R. M. Primary antibody responses to a well-defined and unique hapten are not enhanced by preimmunization with carrier: analysis in a viral model. Proc. Natl Acad. Sci. USA 83, 2604–2608 (1986).
Ochsenbein, A. F. et al. Protective long-term antibody memory by antigen-driven and T help-dependent differentiation of long-lived memory B cells to short-lived plasma cells independent of secondary lymphoid organs. Proc. Natl Acad. Sci. USA 97, 13263–13268 (2000).
Plotkin, S. A. Correlates of protection induced by vaccination. Clin. Vaccine Immunol. 17, 1055–1065 (2010).
Bachmann, M. F. et al. The role of antibody concentration and avidity in antiviral protection. Science 276, 2024–2027 (1997).
Ochsenbein, A. F. et al. Control of early viral and bacterial distribution and disease by natural antibodies. Science 286, 2156–2159 (1999).
Zinkernagel, R. M. On natural and artificial vaccinations. Ann. Rev. Immunol. 21, 515–546 (2003).
Kundig, T. M. et al. On the role of antigen in maintaining cytotoxic T-cell memory. Proc. Natl Acad. Sci. USA 93, 9716–9723 (1996).
Bachmann, M. F. et al. Protection against immunopathological consequences of a viral infection by activated but not resting cytotoxic T cells: T cell memory without “memory T cells”? Proc. Natl Acad. Sci. USA 94, 640–645 (1997).
Bachmann, M. F. et al. Induction of long-lived germinal centers associated with persisting antigen after viral infection. J. Exp. Med. 183, 2259–2269 (1996).
Navarini, A. A. et al. Long-lasting immunity by early infection of maternal-antibody-protected infants. Eur. J. Immunol. 40, 113–116 (2010).
Griffiths, G. M. et al. Somatic mutation and the maturation of immune response to 2-phenyl oxazolone. Nature 312, 271–275 (1984).
Cherry, J. D. Epidemic pertussis in 2012—the resurgence of a vaccine-preventable disease. N. Engl. J. Med. 367, 785–787 (2012).
Sonnenberg, G. F. & Artis, D. Innate lymphoid cells in the initiation, regulation and resolution of inflammation. Nat. Med. 21, 698–708 (2015).
O'Sullivan, T. E., Sun, J. C. & Lanier, L. L. Natural killer cell memory. Immunity 43, 634–645 (2015).
Conrath, U., Beckers, G. J., Langenbach, C. J. & Jaskiewicz, M. R. Priming for enhanced defense. Annu. Rev. Phytopathol. 53, 97–119 (2015).
Kurtz, J. Specific memory within innate immune systems. Trends Immunol. 26, 186–192 (2005).
Quintin, J. et al. Candida albicans infection affords protection against reinfection via functional reprogramming of monocytes. Cell Host Microbe 16, 223–232 (2012).
Saeed, S. et al. Epigenetic programming of monocyte-to-macrophage differentiation and trained innate immunity. Science 345, 1251086 (2014).
Schlums, H. et al. Cytomegalovirus infection drives adaptive epigenetic diversification of NK cells with altered signaling and effector function. Immunity 42, 443–456 (2015).
Lee, J. et al. Epigenetic modification and antibody-dependent expansion of memory-like NK cells in human cytomegalovirus-infected individuals. Immunity 42, 431–442 (2015).
Mackaness, G. B. Resistance to intracellular infection. J. Infect. Dis. 123, 439–445 (1971).
Zinkernagel, R. & Blanden, R. Macrophage activation in mice lacking thymus-derived (T) cells. Experientia 31, 591–593 (1975).
Sallusto, F. et al. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature 401, 708–712 (1999).
Usherwood, E. J. et al. Functionally heterogeneous CD8+ T-cell memory is induced by Sendai virus infection of mice. J. Virol. 73, 7278–7286 (1999).
Ahmadzadeh, M., Hussain, S. F. & Farber, D. L. Heterogeneity of the memory CD4 T cell response: persisting effectors and resting memory T cells. J. Immunol. 166, 926–935 (2001).
Masopust, D. et al. Preferential localization of effector memory cells in nonlymphoid tissue. Science 291, 2413–2417 (2001).
Masopust, D. & Picker, L. J. Hidden memories: frontline memory T cells and early pathogen interception. J. Immunol. 188, 5811–5817 (2012).
Teijaro, J. R. et al. Cutting edge: tissue-retentive lung memory CD4 T cells mediate optimal protection to respiratory virus infection. J. Immunol. 187, 5510–5514 (2011).
Gebhardt, T. et al. Memory T cells in nonlymphoid tissue that provide enhanced local immunity during infection with herpes simplex virus. Nat. Immunol. 10, 524–530 (2009).
Shin, H. & Iwasaki, A. A vaccine strategy that protects against genital herpes by establishing local memory T cells. Nature 491, 463–467 (2012).
Stary, G. et al. A mucosal vaccine against Chlamydia trachomatis generates two waves of protective memory T cells. Science 348, aaa8205 (2015).
Wang, C., Collins, M. & Kuchroo, V. K. Effector T cell differentiation: are master regulators of effector T cells still the masters? Curr. Opin. Immunol. 37, 6–10 (2015).
Mills, C. D. M1 and M2 macrophages: oracles of health and disease. Crit. Rev. Immunol. 32, 463–488 (2012).
Murali-Krishna, K. et al. Counting antigen-specific CD8 T cells: a reevaluation of bystander activation during viral infection. Immunity 8, 177–187 (1998).
Wherry, E. J. et al. Lineage relationship and protective immunity of memory CD8 T cell subsets. Nat. Immunol. 4, 225–234 (2003).
Kaech, S. M. et al. Selective expression of the interleukin 7 receptor identifies effector CD8 T cells that give rise to long-lived memory cells. Nat. Immunol. 4, 1191–1198 (2003).
Tan, J. T. et al. Interleukin (IL)-15 and IL-7 jointly regulate homeostatic proliferation of memory phenotype CD8+ cells but are not required for memory phenotype CD4+ cells. J. Exp. Med. 195, 1523–1532 (2002).
Slifka, M. K., Antia, R., Whitmire, J. K. & Ahmed, R. Humoral immunity due to long-lived plasma cells. Immunity 8, 363–372 (1998).
Halliley, J. L. et al. Long-lived plasma cells are contained within the CD19−CD38hiCD138+ subset in human bone marrow. Immunity 43, 132–145 (2015).
Ochsenbein, A. F. et al. Roles of tumour localization, second signals and cross priming in cytotoxic T-cell induction. Nature 411, 1058–1064 (2001).
Johansen, P. et al. Antigen kinetics determines immune reactivity. Proc. Natl Acad. Sci. USA 105, 5189–5194 (2008).
McGregor, D. D. & Gowans, J. L. The antibody response of rats depleted of lymphocytes by chronic drainage from the thoracic duct. J. Exp. Med. 117, 303–320 (1963).
Sercan Alp, Ö. et al. Memory CD8+ T cells colocalize with IL-7+ stromal cells in bone marrow and rest in terms of proliferation and transcription. Eur. J. Immunol. 45, 975–987 (2015).
Ludewig, B. et al. Immunotherapy with dendritic cells directed against tumor antigens shared with normal host cells results in severe autoimmune disease. J. Exp. Med. 191, 795–804 (2000).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
- Germinal centre
-
A transient, highly organized multicellular structure present within B cell follicles that is a site for the generation of memory B cells and long-lived plasma cells, as well as for affinity maturation of antibodies.
- Hapten
-
A molecule that can be bound by an antibody but cannot elicit an immune response by itself. Antibodies that are specific for a hapten can be generated when the hapten is chemically linked to a protein carrier that can elicit a T cell response. Haptens have no biological significance, as all relevant determinants of immunity (antigens) involve complex tertiary structures with antibody contact areas of approximately 8–15 amino acids or T cell peptide epitopes of 9–11 amino acids presented by MHC molecules.
- Heterologous immunity
-
Also known as 'infection immunity'. Immunity that develops against a pathogen after the host has been exposed to a non-identical pathogen.
- Somatic hypermutation
-
A programmed process of mutation targeting the variable regions of immunoglobulin genes that allows the selection of B cells that express immunoglobulin receptors with the highest affinity for antigens.
- Systemic acquired resistance
-
(SAR). A state of enhanced immunity to infection in plants that occurs throughout the whole plant after it has been subjected to an initial, localized injury.
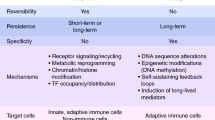
- Trained immunity
-
Also referred to as 'innate memory'. The long-term improvement of the function of innate immune cells after infection or vaccination, owing to epigenetic rewiring of cellular functional programmes.
Rights and permissions
About this article
Cite this article
Farber, D., Netea, M., Radbruch, A. et al. Immunological memory: lessons from the past and a look to the future. Nat Rev Immunol 16, 124–128 (2016). https://doi.org/10.1038/nri.2016.13
Published:
Issue Date:
DOI: https://doi.org/10.1038/nri.2016.13
This article is cited by
-
Innate lymphoid cells and innate-like T cells in cancer — at the crossroads of innate and adaptive immunity
Nature Reviews Cancer (2023)
-
A subpopulation of lipogenic brown adipocytes drives thermogenic memory
Nature Metabolism (2023)
-
The interaction between nanoparticles and immune system: application in the treatment of inflammatory diseases
Journal of Nanobiotechnology (2022)
-
Inflammatory memory and tissue adaptation in sickness and in health
Nature (2022)
-
Innate immune memory and its application to artificial immune systems
The Journal of Supercomputing (2022)