Abstract
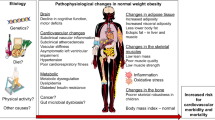
Excessive fat deposition in obesity has a multifactorial aetiology, but is widely considered the result of disequilibrium between energy intake and expenditure. Despite specific public health policies and individual treatment efforts to combat the obesity epidemic, >2 billion people worldwide are overweight or obese. The central nervous system circuitry, fuel turnover and metabolism as well as adipose tissue homeostasis are important to comprehend excessive weight gain and associated comorbidities. Obesity has a profound impact on quality of life, even in seemingly healthy individuals. Diet, physical activity or exercise and lifestyle changes are the cornerstones of obesity treatment, but medical treatment and bariatric surgery are becoming important. Family history, food environment, cultural preferences, adverse reactions to food, perinatal nutrition, previous or current diseases and physical activity patterns are relevant aspects for the health care professional to consider when treating the individual with obesity. Clinicians and other health care professionals are often ill-equipped to address the important environmental and socioeconomic drivers of the current obesity epidemic. Finally, understanding the epigenetic and genetic factors as well as metabolic pathways that take advantage of ‘omics’ technologies could play a very relevant part in combating obesity within a precision approach.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
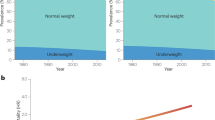
NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 387, 1377–1396 (2016). This article discusses that obesity prevalence could reach 20% of the population by 2025.
Williams, E. P., Mesidor, M., Winters, K., Dubbert, P. M. & Wyatt, S. B. Overweight and obesity: prevalence, consequences, and causes of a growing public health problem. Curr. Obes. Rep. 4, 363–370 (2015).
Alberti, K. G. et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120, 1640–1645 (2009).
Sellayah, D., Cagampang, F. R. & Cox, R. D. On the evolutionary origins of obesity: a new hypothesis. Endocrinology 155, 1573–1588 (2014).
Bhupathiraju, S. N. & Hu, F. B. Epidemiology of obesity and diabetes and their cardiovascular complications. Circ. Res. 118, 1723–1735 (2016).
Martinez, J. A. Body-weight regulation: causes of obesity. Proc. Nutr. Soc. 59, 337–345 (2000).
McAllister, E. J. et al. Ten putative contributors to the obesity epidemic. Crit. Rev. Food Sci. Nutr. 49, 868–913 (2009). This review discusses the putative causes for obesity, which are not generally considered.
Heymsfield, S. B. et al. Multi-component molecular-level body composition reference methods: evolving concepts and future directions. Obes. Rev. 16, 282–294 (2015). This paper suggests that the methods traditionally used to diagnose obesity have been underestimating the problem, but more precise tools are under study and in development.
Seabolt, L. A., Welch, E. B. & Silver, H. J. Imaging methods for analyzing body composition in human obesity and cardiometabolic disease. Ann. NY Acad. Sci. 1353, 41–59 (2015).
Fosbol, M. O. & Zerahn, B. Contemporary methods of body composition measurement. Clin. Physiol. Funct. Imaging 35, 81–97 (2015).
Javed, A. et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity in children and adolescents: a systematic review and meta-analysis. Pediatr. Obes. 10, 234–244 (2015).
Despres, J. P. Body fat distribution and risk of cardiovascular disease: an update. Circulation 126, 1301–1313 (2012). This paper shows that visceral fat accumulation increases the risk of developing obesity-related comorbidities.
Cerhan, J. R. et al. A pooled analysis of waist circumference and mortality in 650,000 adults. Mayo Clin. Proc. 89, 335–345 (2014).
Sahakyan, K. R. et al. Normal-weight central obesity: implications for total and cardiovascular mortality. Ann. Intern. Med. 163, 827–835 (2015).
Urdampilleta, A., Gonzalez-Muniesa, P., Portillo, M. P. & Martinez, J. A. Usefulness of combining intermittent hypoxia and physical exercise in the treatment of obesity. J. Physiol. Biochem. 68, 289–304 (2012).
World Health Organization. Obesity and overweight. WHOhttp://www.who.int/mediacentre/factsheets/fs311/en/ (2015).
Dobbs, R. et al. How the world could better fight obesity (McKinsey Global Institute, 2014).
Cornelsen, L., Green, R., Dangour, A. & Smith, R. Why fat taxes won’t make us thin. J. Public Health (Oxf.) 37, 18–23 (2015).
Malik, V. S., Willett, W. C. & Hu, F. B. Global obesity: trends, risk factors and policy implications. Nat. Rev. Endocrinol. 9, 13–27 (2013).
Lauby-Secretan, B. et al. Body fatness and cancer — viewpoint of the IARC Working Group. N. Engl. J. Med. 375, 794–798 (2016). These data indicate a causal cancer-preventive effect of intentional weight loss.
Ng, M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 766–781 (2014).
Yang, L. & Colditz, G. A. Prevalence of overweight and obesity in the United States, 2007–2012. JAMA Intern. Med. 175, 1412–1413 (2015).
Nazare, J. A. et al. Ethnic influences on the relations between abdominal subcutaneous and visceral adiposity, liver fat, and cardiometabolic risk profile: the International Study of Prediction of Intra-Abdominal Adiposity and Its Relationship With Cardiometabolic Risk/Intra-Abdominal Adiposity. Am. J. Clin. Nutr. 96, 714–726 (2012).
Finucane, M. M. et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 377, 557–567 (2011).
Finkelstein, E. A. et al. Obesity and severe obesity forecasts through 2030. Am. J. Prev. Med. 42, 563–570 (2012).
Kelly, T., Yang, W., Chen, C. S., Reynolds, K. & He, J. Global burden of obesity in 2005 and projections to 2030. Int. J. Obes. (Lond.) 32, 1431–1437 (2008).
Ahmad, O. B. et al. Age standardization of rates: a new WHO standard (WHO, 2001).
Ahluwalia, N. et al. Trends in overweight prevalence among 11-, 13- and 15-year-olds in 25 countries in Europe, Canada and USA from 2002 to 2010. Eur. J. Public Health 25 (Suppl. 2), 28–32 (2015).
Koletzko, B., Symonds, M. E. & Olsen, S. F. Programming research: where are we and where do we go from here? Am. J. Clin. Nutr. 94, 2036S–2043S (2011).
Hanley, B. et al. Metabolic imprinting, programming and epigenetics — a review of present priorities and future opportunities. Br. J. Nutr. 104, S1–S25 (2010).
Eriksson, J. G. Developmental origins of health and disease — from a small body size at birth to epigenetics. Ann. Med. 48, 456–467 (2016).
Dearden, L. & Ozanne, S. E. Early life origins of metabolic disease: developmental programming of hypothalamic pathways controlling energy homeostasis. Front. Neuroendocrinol. 39, 3–16 (2015).
Lin, X. et al. Developmental pathways to adiposity begin before birth and are influenced by genotype, prenatal environment and epigenome. BMC Med. 15, 50 (2017).
Yu, Z. B. et al. Birth weight and subsequent risk of obesity: a systematic review and meta-analysis. Obes. Rev. 12, 525–542 (2011).
Labayen, I. et al. Early life programming of abdominal adiposity in adolescents: the HELENA study. Diabetes Care 32, 2120–2122 (2009).
Druet, C. et al. Prediction of childhood obesity by infancy weight gain: an individual-level meta-analysis. Paediatr. Perinat. Epidemiol. 26, 19–26 (2012).
Chen, L. W. et al. Associations of maternal macronutrient intake during pregnancy with infant BMI peak characteristics and childhood BMI. Am. J. Clin. Nutr. 105, 705–713 (2017).
Arenz, S., Ruckerl, R., Koletzko, B. & von Kries, R. Breast-feeding and childhood obesity — a systematic review. Int. J. Obes. Relat. Metab. Disord. 28, 1247–1256 (2004).
Weber, M. et al. Lower protein content in infant formula reduces BMI and obesity risk at school age: follow-up of a randomized trial. Am. J. Clin. Nutr. 99, 1041–1051 (2014).
Ohlsson, C., Lorentzon, M., Norjavaara, E. & Kindblom, J. M. Age at adiposity rebound is associated with fat mass in young adult males — the GOOD study. PLoS ONE 7, e49404 (2012).
Peneau, S. et al. Age at adiposity rebound: determinants and association with nutritional status and the metabolic syndrome at adulthood. Int. J. Obes. (Lond.) 40, 1150–1156 (2016). This paper suggests that monitoring childhood growth will help to identify children at risk of developing an adverse cardiometabolic profile in adulthood.
Prentice, P. & Viner, R. M. Pubertal timing and adult obesity and cardiometabolic risk in women and men: a systematic review and meta-analysis. Int. J. Obes. (Lond.) 37, 1036–1043 (2013).
Hu, F. B. Obesity Epidemiology (Oxford Univ. Press, 2008).
Hall, K. D. et al. Quantification of the effect of energy imbalance on bodyweight. Lancet 378, 826–837 (2011).
Vague, J. The degree of masculine differentiation of obesities: a factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease. Am. J. Clin. Nutr. 4, 20–34 (1956).
Saeed, S. et al. Genetic variants in LEP, LEPR, and MC4R explain 30% of severe obesity in children from a consanguineous population. Obesity (Silver Spring) 23, 1687–1695 (2015).
Flier, J. S. Obesity wars: molecular progress confronts an expanding epidemic. Cell 116, 337–350 (2004).
Ferguson, L. R. et al. Guide and position of the International Society of Nutrigenetics/Nutrigenomics on personalised nutrition: part 1 — fields of precision nutrition. J. Nutrigenet. Nutrigenomics 9, 12–27 (2016).
Ludwig, D. S. & Nestle, M. Can the food industry play a constructive role in the obesity epidemic? JAMA 300, 1808–1811 (2008).
Bes-Rastrollo, M. et al. A prospective study of eating away-from-home meals and weight gain in a Mediterranean population: the SUN (Seguimiento Universidad de Navarra) cohort. Public Health Nutr. 13, 1356–1363 (2010).
Vandevijvere, S., Chow, C. C., Hall, K. D., Umali, E. & Swinburn, B. A. Increased food energy supply as a major driver of the obesity epidemic: a global analysis. Bull. World Health Organ. 93, 446–456 (2015).
Sayon-Orea, C. et al. Association between sleeping hours and siesta and the risk of obesity: the SUN Mediterranean cohort. Obes. Facts 6, 337–347 (2013).
Ludwig, D. S. Lifespan weighed down by diet. JAMA 315, 2269–2270 (2016).
Jensen, M. D. et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and The Obesity Society. J. Am. Coll. Cardiol. 63, 2985–3023 (2014).
Martinez, J. A., Navas-Carretero, S., Saris, W. H. & Astrup, A. Personalized weight loss strategies-the role of macronutrient distribution. Nat. Rev. Endocrinol. 10, 749–760 (2014). This paper shows that the role of macronutrient distribution has to be considered for individualized dietary approaches.
Razquin, C. et al. A 3 years follow-up of a Mediterranean diet rich in virgin olive oil is associated with high plasma antioxidant capacity and reduced body weight gain. Eur. J. Clin. Nutr. 63, 1387–1393 (2009).
Estruch, R. et al. Effect of a high-fat Mediterranean diet on bodyweight and waist circumference: a prespecified secondary outcomes analysis of the PREDIMED randomised controlled trial. Lancet Diabetes Endocrinol. 4, 666–676 (2016). This paper shows that the Mediterranean diet (without calorie restriction) was associated with body weight loss and less gain in central adiposity.
Mozaffarian, D., Hao, T., Rimm, E. B., Willett, W. C. & Hu, F. B. Changes in diet and lifestyle and long-term weight gain in women and men. N. Engl. J. Med. 364, 2392–2404 (2011).
Schwingshackl, L. et al. Fruit and vegetable consumption and changes in anthropometric variables in adult populations: a systematic review and meta-analysis of prospective cohort studies. PLoS ONE 10, e0140846 (2015).
Smith, J. D. et al. Changes in intake of protein foods, carbohydrate amount and quality, and long-term weight change: results from 3 prospective cohorts. Am. J. Clin. Nutr. 101, 1216–1224 (2015).
Mozaffarian, D. Food and weight gain: time to end our fear of fat. Lancet Diabetes Endocrinol. 4, 633–635 (2016).
Tobias, D. K. et al. Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 3, 968–979 (2015).
Cornier, M. A., Marshall, J. A., Hill, J. O., Maahs, D. M. & Eckel, R. H. Prevention of overweight/obesity as a strategy to optimize cardiovascular health. Circulation 124, 840–850 (2011).
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation (WHO Technical Report Series 894) (WHO, 2000).
Nordestgaard, B. G. et al. The effect of elevated body mass index on ischemic heart disease risk: causal estimates from a Mendelian randomisation approach. PLoS Med. 9, e1001212 (2012).
Park, M. H., Sovio, U., Viner, R. M., Hardy, R. J. & Kinra, S. Overweight in childhood, adolescence and adulthood and cardiovascular risk in later life: pooled analysis of three British birth cohorts. PLoS ONE 8, e70684 (2013).
Renehan, A. G. et al. Incident cancer burden attributable to excess body mass index in 30 European countries. Int. J. Cancer 126, 692–702 (2010).
Wang, Y. C., McPherson, K., Marsh, T., Gortmaker, S. L. & Brown, M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 378, 815–825 (2011).
Jauch-Chara, K. & Oltmanns, K. M. Obesity — a neuropsychological disease? Systematic review and neuropsychological model. Prog. Neurobiol. 114, 84–101 (2014).
Global BMI Mortality Collaboration. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 388, 776–786 (2016). This article reports that overweight and obesity consistently increase all-cause mortality worldwide.
Flegal, K. M., Kit, B. K., Orpana, H. & Graubard, B. I. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 309, 71–82 (2013).
de Onis, M. & Lobstein, T. Defining obesity risk status in the general childhood population: which cut-offs should we use? Int. J. Pediatr. Obes. 5, 458–460 (2010).
Stokes, A. Using maximum weight to redefine body mass index categories in studies of the mortality risks of obesity. Popul. Health Metr. 12, 6 (2014).
Despres, J. P. & Lemieux, I. Abdominal obesity and metabolic syndrome. Nature 444, 881–887 (2006).
Elks, C. E. et al. Variability in the heritability of body mass index: a systematic review and meta-regression. Front. Endocrinol. (Lausanne) 3, 29 (2012).
Meyers, M. G. Jr & Leibel, R. L. Lessons from rodent models of obesity. Endotexthttps://www.ncbi.nlm.nih.gov/books/NBK279123/ (updated 6 Sept 2015).
van der Klaauw, A. A. & Farooqi, I. S. The hunger genes: pathways to obesity. Cell 161, 119–132 (2015).
Frayling, T. M. et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science 316, 889–894 (2007).
Scuteri, A. et al. Genome-wide association scan shows genetic variants in the FTO gene are associated with obesity-related traits. PLoS Genet. 3, e115 (2007).
Yang, J. et al. FTO genotype is associated with phenotypic variability of body mass index. Nature 490, 267–272 (2012).
Milagro, F. I., Moreno-Aliaga, M. J. & Martinez, J. A. FTO obesity variant and adipocyte browning in humans. N. Engl. J. Med. 374, 190–191 (2016).
Locke, A. E. et al. Genetic studies of body mass index yield new insights for obesity biology. Nature 518, 197–206 (2015).
Shungin, D. et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature 518, 187–196 (2015).
Winkler, T. W. et al. The influence of age and sex on genetic associations with adult body size and shape: a large-scale genome-wide interaction study. PLoS Genet. 11, e1005378 (2015).
Loche, E. & Ozanne, S. E. Early nutrition, epigenetics, and cardiovascular disease. Curr. Opin. Lipidol. 27, 449–458 (2016).
Ravelli, G. P., Stein, Z. A. & Susser, M. Obesity in young men after famine exposure in utero and early infancy. N. Engl. J. Med. 295, 349–353 (1976).
Heijmans, B. T. et al. Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proc. Natl Acad. Sci. USA 105, 17046–17049 (2008).
Dick, K. J. et al. DNA methylation and body-mass index: a genome-wide analysis. Lancet 383, 1990–1998 (2014).
Jiang, C. et al. Disruption of hypoxia-inducible factor 1 in adipocytes improves insulin sensitivity and decreases adiposity in high-fat diet-fed mice. Diabetes 60, 2484–2495 (2011).
Wahl, S. et al. Epigenome-wide association study of body mass index, and the adverse outcomes of adiposity. Nature 541, 81–86 (2017).
Mendelson, M. M. et al. Association of body mass index with DNA methylation and gene expression in blood cells and relations to cardiometabolic disease: a Mendelian randomization approach. PLoS Med. 14, e1002215 (2017).
van Dijk, S. J. et al. Epigenetics and human obesity. Int. J. Obes. (Lond.) 39, 85–97 (2015). This paper reports that unfavourable epigenomic profiles could be modified with appropriate lifestyle programmes.
Giralt, M. & Villarroya, F. White, brown, beige/brite: different adipose cells for different functions? Endocrinology 154, 2992–3000 (2013). This paper suggests that understanding brown adipocyte activity and differentiation could be a useful tool to increase energy expenditure and the fight against obesity.
Sacks, H. & Symonds, M. E. Anatomical locations of human brown adipose tissue functional relevance and implications in obesity and type 2 diabetes. Diabetes 62, 1783–1790 (2013).
Santhanam, P., Solnes, L., Hannukainen, J. C. & Taieb, D. Adiposity-related cancer and functional imaging of brown adipose tissue. Endocr. Pract. 21, 1282–1290 (2015).
Prodhomme, H. et al. Imaging and identification of brown adipose tissue on CT scan. Clin. Physiol. Funct. Imaginghttp://dx.doi.org/10.1111/cpf.12373 (2016).
Matsuzawa, Y. The metabolic syndrome and adipocytokines. FEBS Lett. 580, 2917–2921 (2006).
Kotani, K. et al. Sexual dimorphism of age-related changes in whole-body fat distribution in the obese. Int. J. Obes. Relat. Metab. Disord. 18, 207–202 (1994).
Rosen, E. D. & Spiegelman, B. M. What we talk about when we talk about fat. Cell 156, 20–44 (2014).
Shulman, G. I. Ectopic fat in insulin resistance, dyslipidemia, and cardiometabolic disease. N. Engl. J. Med. 371, 1131–1141 (2014).
Gonzalez-Muniesa, P. et al. Effects of hyperoxia on oxygen-related inflammation with a focus on obesity. Oxid. Med. Cell. Longev. 2015, 8957827 (2015).
Karpe, F. & Pinnick, K. E. Biology of upper-body and lower-body adipose tissue — link to whole-body phenotypes. Nat. Rev. Endocrinol. 11, 90–100 (2015).
Rosito, G. A. et al. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study. Circulation 117, 605–613 (2008).
Thanassoulis, G. et al. Prevalence, distribution, and risk factor correlates of high pericardial and intrathoracic fat depots in the Framingham Heart Study. Circ. Cardiovasc. Imaging 3, 559–566 (2010).
Thomas, E. L. et al. The missing risk: MRI and MRS phenotyping of abdominal adiposity and ectopic fat. Obesity (Silver Spring) 20, 76–87 (2012). This article defines a new subphenotype, called thin-on-the-outside fat-on-the-inside (TOFI), for individuals at increased metabolic risk.
Ross, R. et al. Does the relationship between waist circumference, morbidity and mortality depend on measurement protocol for waist circumference? Obes. Rev. 9, 312–325 (2008).
Fabbrini, E. et al. Intrahepatic fat, not visceral fat, is linked with metabolic complications of obesity. Proc. Natl Acad. Sci. USA 106, 15430–15435 (2009).
Neeland, I. J. et al. Body fat distribution and incident cardiovascular disease in obese adults. J. Am. Coll. Cardiol. 65, 2150–2151 (2015).
Monajemi, H., Stroes, E., Hegele, R. A. & Fliers, E. Inherited lipodystrophies and the metabolic syndrome. Clin. Endocrinol. (Oxf.) 67, 479–484 (2007).
Patni, N. & Garg, A. Congenital generalized lipodystrophies — new insights into metabolic dysfunction. Nat. Rev. Endocrinol. 11, 522–534 (2015).
Iannucci, C. V., Capoccia, D., Calabria, M. & Leonetti, F. Metabolic syndrome and adipose tissue: new clinical aspects and therapeutic targets. Curr. Pharm. Des. 13, 2148–2168 (2007).
Camilleri, M. Peripheral mechanisms in appetite regulation. Gastroenterology 148, 1219–1233 (2015).
Ridaura, V. K. et al. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science 341, 1241214 (2013).
Santacruz, A. et al. Interplay between weight loss and gut microbiota composition in overweight adolescents. Obesity (Silver Spring) 17, 1906–1915 (2009).
Stenholm, S. et al. Sarcopenic obesity: definition, cause and consequences. Curr. Opin. Clin. Nutr. Metab. Care 11, 693–700 (2008).
Prado, C. M. et al. A population-based approach to define body-composition phenotypes. Am. J. Clin. Nutr. 99, 1369–1377 (2014).
Stefan, N., Haring, H. U., Hu, F. B. & Schulze, M. B. Metabolically healthy obesity: epidemiology, mechanisms, and clinical implications. Lancet Diabetes Endocrinol. 1, 152–162 (2013).
Teixeira, T. F., Alves, R. D., Moreira, A. P. & Peluzio Mdo, C. Main characteristics of metabolically obese normal weight and metabolically healthy obese phenotypes. Nutr. Rev. 73, 175–190 (2015).
Hwang, Y. C. et al. Visceral abdominal fat accumulation predicts the conversion of metabolically healthy obese subjects to an unhealthy phenotype. Int. J. Obes. (Lond.) 39, 1365–1370 (2015). This paper provides data to differentiate between metabolically healthy obese and metabolically unhealthy obese, and the conversion from the former to the latter.
Franco, L. P., Morais, C. C. & Cominetti, C. Normal-weight obesity syndrome: diagnosis, prevalence, and clinical implications. Nutr. Rev. 74, 558–570 (2016).
Chan, J. C. et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 301, 2129–2140 (2009).
Zheng, W. et al. Association between body-mass index and risk of death in more than 1 million Asians. N. Engl. J. Med. 364, 719–729 (2011).
Ortega, F. B., Sui, X., Lavie, C. J. & Blair, S. N. Body mass index, the most widely used but also widely criticized index: would a criterion standard measure of total body fat be a better predictor of cardiovascular disease mortality? Mayo Clin. Proc. 91, 443–455 (2016).
Savva, S. C., Lamnisos, D. & Kafatos, A. G. Predicting cardiometabolic risk: waist-to-height ratio or BMI. A meta-analysis. Diabetes Metab. Syndr. Obes. 6, 403–419 (2013).
Marques, M. et al. Design of the nutritional therapy for overweight and obese Spanish adolescents conducted by registered dieticians: the EVASYON study. Nutr. Hosp. 27, 165–176 (2012).
Dong, B., Wang, Z., Wang, H. J. & Ma, J. Associations between adiposity indicators and elevated blood pressure among Chinese children and adolescents. J. Hum. Hypertens. 29, 236–240 (2015).
Guo, F., Moellering, D. R. & Garvey, W. T. The progression of cardiometabolic disease: validation of a new cardiometabolic disease staging system applicable to obesity. Obesity (Silver Spring) 22, 110–118 (2014).
Sharma, A. M. & Kushner, R. F. A proposed clinical staging system for obesity. Int. J. Obes. (Lond.) 33, 289–295 (2009).
Heo, M., Faith, M. S., Pietrobelli, A. & Heymsfield, S. B. Percentage of body fat cutoffs by sex, age, and race-ethnicity in the US adult population from NHANES 1999–2004. Am. J. Clin. Nutr. 95, 594–602 (2012).
Lobstein, T. et al. Child and adolescent obesity: part of a bigger picture. Lancet 385, 2510–2520 (2015).
Swinburn, B. A. et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet 378, 804–814 (2011).
Blake-Lamb, T. L. et al. Interventions for childhood obesity in the first 1,000 days a systematic review. Am. J. Prev. Med. 50, 780–789 (2016).
Tanvig, M. et al. Anthropometrics and body composition by dual energy X-ray in children of obese women: a follow-up of a randomized controlled trial (the Lifestyle in Pregnancy and Offspring [LiPO] study). PLoS ONE 9, e89590 (2014).
Gillman, M. W. et al. Effect of treatment of gestational diabetes mellitus on obesity in the next generation. Diabetes Care 33, 964–968 (2010).
Wen, L. M. et al. Effectiveness of home based early intervention on children's BMI at age 2: randomised controlled trial. BMJ 344, e3732 (2012).
Navarro, J. I., Sigulem, D. M., Ferraro, A. A., Polanco, J. J. & Barros, A. J. The double task of preventing malnutrition and overweight: a quasi-experimental community-based trial. BMC Public Health 13, 212 (2013).
Ciampa, P. J. et al. Interventions aimed at decreasing obesity in children younger than 2 years: a systematic review. Arch. Pediatr. Adolesc. Med. 164, 1098–1104 (2010).
Summerbell, C. D. et al. Evidence-based recommendations for the development of obesity prevention programs targeted at preschool children. Obes. Rev. 13 (Suppl. 1), 129–132 (2012).
Waters, E. et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 12, CD001871 (2011).
Shah, R., Kennedy, S., Clark, M. D., Bauer, S. C. & Schwartz, A. Primary care-based interventions to promote positive parenting behaviors: a meta-analysis. Pediatrics 137, e20153393 (2016).
Ewart-Pierce, E., Mejia Ruiz, M. J. & Gittelsohn, J. “Whole-of-community” obesity prevention: a review of challenges and opportunities in multilevel, multicomponent interventions. Curr. Obes. Rep. 5, 361–374 (2016).
Gluckman, P., Nishtar, S. & Armstrong, T. Ending childhood obesity: a multidimensional challenge. Lancet 385, 1048–1050 (2015).
Moreno, L. A. et al. Nutrition and lifestyle in European adolescents: the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) study. Adv. Nutr. 5, 615S–623S (2014).
Burke, L. E., Wang, J. & Sevick, M. A. Self-monitoring in weight loss: a systematic review of the literature. J. Am. Diet. Assoc. 111, 92–102 (2011).
Apovian, C. M. et al. Pharmacological management of obesity: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 100, 342–362 (2015).
Eckel, R. H. et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J. Am. Coll. Cardiol. 63, 2960–2984 (2014).
Garvey, W. T. et al. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity: executive summary: complete guidelines available at https://www.aace.com/publications/guidelines. Endocr. Pract. 22, 842–884 (2016).
National Clinical Guideline Centre. Obesity: identification, assessment and management of overweight and obesity in children, young people and adults: partial update of CG43 (National Clinical Guideline Centre, 2014).
Jensen, M. D. et al. Executive summary: guidelines (2013) for the management of overweight and obesity in adults. Obesity 22, S5–S39 (2014).
Yumuk, V., Fruhbeck, G., Oppert, J. M., Woodward, E. & Toplak, H. An EASO position statement on multidisciplinary obesity management in adults. Obes. Facts 7, 96–101 (2014).
Bray, G. A. & Siri-Tarino, P. W. The role of macronutrient content in the diet for weight management. Endocrinol. Metab. Clin. North Am. 45, 581–604 (2016).
Bray, G. A., Fruhbeck, G., Ryan, D. H. & Wilding, J. P. Management of obesity. Lancet 387, 1947–1956 (2016). This review explains the latest lifestyle programmes, pharmacological treatments and surgical procedures to manage obesity.
Wadden, T. A., Webb, V. L., Moran, C. H. & Bailer, B. A. Lifestyle modification for obesity: new developments in diet, physical activity, and behavior therapy. Circulation 125, 1157–1170 (2012).
Leblanc, E. S., O’Connor, E., Whitlock, E. P., Patnode, C. D. & Kapka, T. Effectiveness of primary care-relevant treatments for obesity in adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann. Intern. Med. 155, 434–447 (2011).
Robinson, E. et al. A systematic review and meta-analysis examining the effect of eating rate on energy intake and hunger. Am. J. Clin. Nutr. 100, 123–151 (2014).
Tate, D. F. A series of studies examining Internet treatment of obesity to inform Internet interventions for substance use and misuse. Subst. Use Misuse 46, 57–65 (2011).
Mozaffarian, D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation 133, 187–225 (2016).
Johnston, B. C. et al. Comparison of weight loss among named diet programs in overweight and obese adults: a meta-analysis. JAMA 312, 923–933 (2014).
Abete, I., Astrup, A., Martínez, J. A., Thorsdottir, I. & Zulet, M. A. Obesity and the metabolic syndrome: role of different dietary macronutrient distribution patterns and specific nutritional components on weight loss and maintenance. Nutr. Rev. 68, 214–231 (2010).
Larsen, T. M. et al. Diets with high or low protein content and glycemic index for weight-loss maintenance. N. Engl. J. Med. 363, 2102–2113 (2010).
de la Iglesia, R. et al. Dietary strategies implicated in the prevention and treatment of metabolic syndrome. Int. J. Mol. Sci. 17, E1877 (2016).
Donnelly, J. E. et al. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med. Sci. Sports Exerc. 41, 459–471 (2009).
World Health Organization. Global recommendations on physical activity for health (WHO, 2010).
Wu, T., Gao, X., Chen, M. & van Dam, R. M. Long-term effectiveness of diet-plus-exercise interventions versus diet-only interventions for weight loss: a meta-analysis. Obes. Rev. 10, 313–323 (2009).
Jakicic, J. M., Marcus, B. H., Lang, W. & Janney, C. Effect of exercise on 24-month weight loss maintenance in overweight women. Arch. Intern. Med. 168, 1550–1559 (2008).
Look AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity (Silver Spring) 22, 5–13 (2014).
Ross, R., Hudson, R., Stotz, P. J. & Lam, M. Effects of exercise amount and intensity on abdominal obesity and glucose tolerance in obese adults: a randomized trial. Ann. Intern. Med. 162, 325–334 (2015).
Solas, M., Milagro, F. I., Martinez-Urbistondo, D., Ramirez, M. J. & Martinez, J. A. Precision obesity treatments including pharmacogenetic and nutrigenetic approaches. Trends Pharmacol. Sci. 37, 575–593 (2016).
Schauer, P. R. et al. Bariatric surgery versus intensive medical therapy for diabetes — 3-year outcomes. N. Engl. J. Med. 370, 2002–2013 (2014).
Rubino, F. et al. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by International Diabetes Organizations. Diabetes Care 39, 861–877 (2016).
Courcoulas, A. P. et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA 310, 2416–2425 (2013).
Inge, T. H. et al. Weight loss and health status 3 years after bariatric surgery in adolescents. N. Engl. J. Med. 374, 113–123 (2016).
Sjostrom, L. Review of the key results from the Swedish Obese Subjects (SOS) trial — a prospective controlled intervention study of bariatric surgery. J. Intern. Med. 273, 219–234 (2013).
Ikramuddin, S. et al. Roux-en-Y gastric bypass versus intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA 309, 2240–2249 (2013).
Sjostrom, L. et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA 311, 2297–2304 (2014).
Nguyen, K. T. & Korner, J. The sum of many parts: potential mechanisms for improvement in glucose homeostasis after bariatric surgery. Curr. Diab. Rep. 14, 481 (2014).
Colquitt, J. L., Pickett, K., Loveman, E. & Frampton, G. K. Surgery for weight loss in adults. Cochrane Database Syst. Rev. 8, CD003641 (2014).
Chang, S. H. et al. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003–2012. JAMA Surg. 149, 275–287 (2014).
Kroes, M., Osei-Assibey, G., Baker-Searle, R. & Huang, J. Impact of weight change on quality of life in adults with overweight/obesity in the United States: a systematic review. Curr. Med. Res. Opin. 32, 485–508 (2016). This paper reports that weight loss should improve quality of life in people who are overweight and obese.
Perez-Cornago, A. et al. A decline in inflammation is associated with less depressive symptoms after a dietary intervention in metabolic syndrome patients: a longitudinal study. Nutr. J. 13, 36 (2014).
Vallis, M. Quality of life and psychological well-being in obesity management: improving the odds of success by managing distress. Int. J. Clin. Pract. 70, 196–205 (2016).
Groessl, E. J., Kaplan, R. M., Barrett-Connor, E. & Ganiats, T. G. Body mass index and quality of well-being in a community of older adults. Am. J. Prev. Med. 26, 126–129 (2004).
Brazier, J., Jones, N. & Kind, P. Testing the validity of the Euroqol and comparing it with the SF-36 health survey questionnaire. Qual. Life Res. 2, 169–180 (1993).
Muennig, P., Lubetkin, E., Jia, H. & Franks, P. Gender and the burden of disease attributable to obesity. Am. J. Public Health 96, 1662–1668 (2006).
Cameron, A. J. et al. A bi-directional relationship between obesity and health-related quality of life: evidence from the longitudinal AusDiab study. Int. J. Obes. (Lond.) 36, 295–303 (2012).
Kolotkin, R. L., Crosby, R. D., Williams, G. R., Hartley, G. G. & Nicol, S. The relationship between health-related quality of life and weight loss. Obes. Res. 9, 564–571 (2001).
Pan, A. et al. Changes in body weight and health-related quality of life: 2 cohorts of US women. Am. J. Epidemiol. 180, 254–262 (2014).
Warkentin, L. M. et al. Weight loss required by the severely obese to achieve clinically important differences in health-related quality of life: two-year prospective cohort study. BMC Med. 12, 175 (2014).
de Beer, M. et al. Health-related-quality-of-life in obese adolescents is decreased and inversely related to BMI. Acta Paediatr. 96, 710–714 (2007).
Helseth, S., Haraldstad, K. & Christophersen, K. A. A cross-sectional study of health related quality of life and body mass index in a Norwegian school sample (8–18 years): a comparison of child and parent perspectives. Health Qual. Life Outcomes 13, 47 (2015).
Tsiros, M. D. et al. Health-related quality of life in obese children and adolescents. Int. J. Obes. (Lond.) 33, 387–400 (2009).
Wille, N., Erhart, M., Petersen, C. & Ravens-Sieberer, U. The impact of overweight and obesity on health-related quality of life in childhood — results from an intervention study. BMC Public Health 8, 421 (2008).
Wu, J., Cohen, P. & Spiegelman, B. M. Adaptive thermogenesis in adipocytes: is beige the new brown? Genes Dev. 27, 234–250 (2013).
Goni, L., Cuervo, M., Milagro, F. I. & Martinez, J. A. Future perspectives of personalized weight loss interventions based on nutrigenetic, epigenetic, and metagenomic data. J. Nutr. 146, 905S–912S (2016). This paper suggests that personalized dietary treatments could benefit from the integration of nutrigenetic, epigenetic and metagenomic data.
Giles-Corti, B. et al. City planning and population health: a global challenge. Lancet 388, 2912–2924 (2016).
Taheri, S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Arch. Dis. Child. 91, 881–884 (2006).
Diaz-Gutierrez, J. et al. Living at higher altitude and incidence of overweight/obesity: prospective analysis of the SUN cohort. PLoS ONE 11, e0164483 (2016).
Lopez-Pascual, A. et al. Living at a geographically higher elevation is associated with lower risk of metabolic syndrome: prospective analysis of the SUN cohort. Front. Physiol. 7, 658 (2016).
Kelley, C. P., Sbrocco, G. & Sbrocco, T. Behavioral modification for the management of obesity. Prim. Care 43, 159–175 (2016).
Enright, G. et al. Evaluating factors influencing the delivery and outcomes of an incentive-based behaviour change strategy targeting child obesity: protocol for a qualitative process and impact evaluation. BMJ Open 6, e012536 (2016).
Kahn, R., Buse, J., Ferrannini, E. & Stern, M. The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 28, 2289–2304 (2005).
Zulet, M. A. et al. The reduction of the metabolyc syndrome in Navarra-Spain (RESMENA-S) study: a multidisciplinary strategy based on chrononutrition and nutritional education, together with dietetic and psychological control. Nutr. Hosp. 26, 16–26 (2011).
Brazier, J. E. et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 305, 160–164 (1992).
Kolotkin, R. L., Crosby, R. D., Kosloski, K. D. & Williams, G. R. Development of a brief measure to assess quality of life in obesity. Obes. Res. 9, 102–111 (2001).
McHorney, C. A., Ware, J. E. Jr & Raczek, A. E. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med. Care 31, 247–263 (1993).
Kolotkin, R. L. & Crosby, R. D. Psychometric evaluation of the impact of weight on quality of life-lite questionnaire (IWQOL-lite) in a community sample. Qual. Life Res. 11, 157–171 (2002).
Crosby, R. D., Kolotkin, R. L. & Williams, G. R. An integrated method to determine meaningful changes in health-related quality of life. J. Clin. Epidemiol. 57, 1153–1160 (2004).
Wyrwich, K. W., Tierney, W. M., Babu, A. N., Kroenke, K. & Wolinsky, F. D. A comparison of clinically important differences in health-related quality of life for patients with chronic lung disease, asthma, or heart disease. Health Serv. Res. 40, 577–591 (2005).
Janicke, D. M. et al. Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity. J. Pediatr. Psychol. 39, 809–825 (2014).
Modi, A. C. & Zeller, M. H. The IWQOL-Kids©: establishing minimal clinically important difference scores and test-retest reliability. Int. J. Pediatr. Obes. 6, e94–e96 (2011).
Lai, C. S., Wu, J. C., Ho, C. T. & Pan, M. H. Chemoprevention of obesity by dietary natural compounds targeting mitochondrial regulation. Mol. Nutr. Food Res. 61, 1600721 (2017).
De Fanti, B. A., Milagro, F. I., Lamas, O., Martinez-Anso, E. & Martinez, J. A. Immunomanipulation of appetite and body temperature through the functional mimicry of leptin. Obes. Res. 10, 833–837 (2002).
De Fanti, B. A., Lamas, O., Milagro, F. I., Martinez-Anso, E. & Martinez, J. A. Immunoneutralization and anti-idiotype production: two-sided applications of leptin. Trends Immunol. 23, 180–181 (2002). This article reports on immunotherapy as an obesity treatment.
Martinez-Fernandez, L., Laiglesia, L. M., Huerta, A. E., Martinez, J. A. & Moreno-Aliaga, M. J. Omega-3 fatty acids and adipose tissue function in obesity and metabolic syndrome. Prostaglandins Other Lipid Mediat. 121, 24–41 (2015).
Arias, N. et al. A combination of resveratrol and quercetin induces browning in white adipose tissue of rats fed an obesogenic diet. Obesity (Silver Spring) 25, 111–121 (2017).
Gonzalez-Muniesa, P. et al. Impact of intermittent hypoxia and exercise on blood pressure and metabolic features from obese subjects suffering sleep apnea-hypopnea syndrome. J. Physiol. Biochem. 71, 589–599 (2015).
Quintero, P., Milagro, F., Campion, J. & Martinez, J. Impact of oxygen availability on body weight management. Med. Hypotheses 74, 901–907 (2010).
Gonzalez-Muniesa, P., Milagro, F. I., Campion, J. & Martinez, J. A. Reduction in energy efficiency induced by expression of the uncoupling protein, UCP1, in mouse liver mitochondria. Int. J. Mol. Med. 17, 591–597 (2006).
Marti, A., Larrarte, E., Novo, F. J., Garcia, M. & Martinez, J. A. UCP2 muscle gene transfer modifies mitochondrial membrane potential. Int. J. Obes. Relat. Metab. Disord. 25, 68–74 (2001).
Cordero, P., Campion, J., Milagro, F. I., Marzo, F. & Martinez, J. A. Fat-to-glucose interconversion by hydrodynamic transfer of two glyoxylate cycle enzyme genes. Lipids Health Dis. 7, 49 (2008).
Rolland-Cachera, M. F., Deheeger, M., Maillot, M. & Bellisle, F. Early adiposity rebound: causes and consequences for obesity in children and adults. Int. J. Obes. (Lond.) 30, S11–S17 (2006).
Jensen, S. M., Ritz, C., Ejlerskov, K. T., Molgaard, C. & Michaelsen, K. F. Infant BMI peak, breastfeeding, and body composition at age 3y. Am. J. Clin. Nutr. 101, 319–325 (2015).
Hiuge-Shimizu, A. et al. Absolute value of visceral fat area measured on computed tomography scans and obesity-related cardiovascular risk factors in large-scale Japanese general population (the VACATION-J study). Ann. Med. 44, 82–92 (2012).
de Heredia, F. P., Gomez-Martinez, S. & Marcos, A. Obesity, inflammation and the immune system. Proc. Nutr. Soc. 71, 332–338 (2012).
Ouchi, N., Parker, J. L., Lugus, J. J. & Walsh, K. Adipokines in inflammation and metabolic disease. Nat. Rev. Immunol. 11, 85–97 (2011).
Naik, R. D., Choksi, Y. A. & Vaezi, M. F. Consequences of bariatric surgery on oesophageal function in health and disease. Nat. Rev. Gastroenterol. Hepatol. 13, 111–119 (2016).
Torgerson, J. S., Hauptman, J., Boldrin, M. N. & Sjostrom, L. XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care 27, 155–161 (2004).
Smith, S. R. et al. Multicenter, placebo-controlled trial of lorcaserin for weight management. N. Engl. J. Med. 363, 245–256 (2010).
Pi-Sunyer, X. et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N. Engl. J. Med. 373, 11–22 (2015).
Marso, S. P. et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 375, 311–322 (2016).
Aronne, L. J. et al. Evaluation of phentermine and topiramate versus phentermine/topiramate extended-release in obese adults. Obesity (Silver Spring) 21, 2163–2171 (2013).
Nissen, S. E. et al. Effect of naltrexone-bupropion on major adverse cardiovascular events in overweight and obese patients with cardiovascular risk factors: a randomized clinical trial. JAMA 315, 990–1004 (2016).
Cefalu, W. T. et al. Advances in the science, treatment, and prevention of the disease of obesity: reflections from a Diabetes Care Editors’ Expert Forum. Diabetes Care 38, 1567–1582 (2015).
Acknowledgements
The authors thank the Spanish Government Carlos III Health Institute Centre of Biomedical Research Network (CIBERobn Physiopathology of Obesity and Nutrition) for support and funding.
Author information
Authors and Affiliations
Contributions
Introduction (P.G.-M. and J.A.M.); Epidemiology (F.B.H. and M.-A.M.-G.); Mechanisms/pathophysiology (J.-P.D., Y.M. and R.J.F.L.); Diagnosis, screening and prevention (L.A.M.); Management (G.A.B.); Quality of life (M.-A.M.-G.); Outlook (P.G.-M. and J.A.M.); Overview of the Primer (J.A.M.).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
González-Muniesa, P., Mártinez-González, MA., Hu, F. et al. Obesity. Nat Rev Dis Primers 3, 17034 (2017). https://doi.org/10.1038/nrdp.2017.34
Published:
DOI: https://doi.org/10.1038/nrdp.2017.34
This article is cited by
-
Association of anthropometric measures with all-cause and cause-specific mortality in US adults: revisiting the obesity paradox
BMC Public Health (2024)
-
An RNA-seq atlas of mouse brain areas during fasting and diet-induced obesity
Scientific Data (2024)
-
Patients with Obesity Should be Recognised as a Special Patient Population During Drug Development of Antibacterial and Antifungal Agents; A Call to Action
Clinical Pharmacokinetics (2024)
-
Whole genome sequencing of mouse lines divergently selected for fatness (FLI) and leanness (FHI) revealed several genetic variants as candidates for novel obesity genes
Genes & Genomics (2024)
-
Current progress and limitations of research regarding the therapeutic use of adipose-derived stem cells: literature review
Journal of Umm Al-Qura University for Applied Sciences (2024)