Abstract
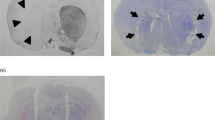
Recent clinical and preclinical studies have shown that hyperkinetic disorders such as Huntington's disease, dystonia and l-DOPA-induced dyskinesia in Parkinson's disease are all characterized by loss of the ability to reverse synaptic plasticity and an associated increase in the excitability of excitatory neuronal inputs to a range of cortical and subcortical brain areas. Moreover, these changes have been detected in humans with hyperkinetic disorders either via direct recordings from implanted deep brain electrodes or noninvasively using transcranial magnetic stimulation. Here we discuss the mechanisms underlying the loss of bidirectional plasticity and the possibility that future interventions could be devised to reverse these changes in patients with hyperkinetic movement disorders.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Kim Caesar/Nature Publishing Group



Kim Caesar/Nature Publishing Group
Similar content being viewed by others
References
Calabresi, P., Picconi, B., Tozzi, A., Ghiglieri, V. & Di Filippo, M. Direct and indirect pathways of basal ganglia: a critical reappraisal. Nat. Neurosci. 17, 1022–1030 (2014).
Malenka, R.C. & Bear, M.F. LTP and LTD: an embarrassment of riches. Neuron 44, 5–21 (2004).
Marras, C. et al. Nomenclature of genetic movement disorders: recommendations of the International Parkinson and Movement Disorder Society Task Force. Mov. Disord. 31, 436–457 (2016).
Plotkin, J.L. & Surmeier, D.J. Corticostriatal synaptic adaptations in Huntington’s disease. Curr. Opin. Neurobiol. 33, 53–62 (2015).
Zuccato, C. & Cattaneo, E. Huntington’s disease. Handb. Exp. Pharmacol. 220, 357–409 (2014).
Quartarone, A. & Pisani, A. Abnormal plasticity in dystonia: disruption of synaptic homeostasis. Neurobiol. Dis. 42, 162–170 (2011).
Standaert, D.G. Update on the pathology of dystonia. Neurobiol. Dis. 42, 148–151 (2011).
Calabresi, P., Di Filippo, M., Ghiglieri, V., Tambasco, N. & Picconi, B. Levodopa-induced dyskinesias in patients with Parkinson’s disease: filling the bench-to-bedside gap. Lancet Neurol. 9, 1106–1117 (2010).
Cenci, M.A. Presynaptic mechanisms of l-DOPA-Induced Dyskinesia: the findings, the debate, and the therapeutic implications. Front. Neurol. 5, 242 (2014).
Day, M. et al. Selective elimination of glutamatergic synapses on striatopallidal neurons in Parkinson disease models. Nat. Neurosci. 9, 251–259 (2006).An elegant paper showing that dopamine depletion leads to rapid and selective loss of spines and glutamatergic synapses on striatopallidal spiny neurons.
Ueno, T. et al. Morphological and electrophysiological changes in intratelencephalic-type pyramidal neurons in the motor cortex of a rat model of levodopa-induced dyskinesia. Neurobiol. Dis. 64, 142–149 (2014).
Raymond, L.A. et al. Pathophysiology of Huntington’s disease: time-dependent alterations in synaptic and receptor function. Neuroscience 198, 252–273 (2011).
Galvan, L., André, V.M., Wang, E.A., Cepeda, C. & Levine, M.S. Functional differences between direct and indirect striatal output pathways in Huntington’s disease. J. Huntingtons Dis. 1, 17–25 (2012).
Picconi, B. et al. Plastic and behavioral abnormalities in experimental Huntington’s disease: a crucial role for cholinergic interneurons. Neurobiol. Dis. 22, 143–152 (2006).An important study showing early loss of depotentiation in striatal spiny neurons in a genetic model of Huntington’s disease.
Plotkin, J.L. et al. Impaired TrkB receptor signaling underlies corticostriatal dysfunction in Huntington’s disease. Neuron 83, 178–188 (2014).
Milnerwood, A.J. & Raymond, L.A. Corticostriatal synaptic function in mouse models of Huntington’s disease: early effects of huntingtin repeat length and protein load. J. Physiol. (Lond.) 585, 817–831 (2007).
Tang, T.S., Chen, X., Liu, J. & Bezprozvanny, I. Dopaminergic signaling and striatal neurodegeneration in Huntington’s disease. J. Neurosci. 27, 7899–7910 (2007).
Ariano, M.A. et al. Striatal neurochemical changes in transgenic models of Huntington’s disease. J. Neurosci. Res. 68, 716–729 (2002).
Tarditi, A. et al. Early and transient alteration of adenosine A2A receptor signaling in a mouse model of Huntington disease. Neurobiol. Dis. 23, 44–53 (2006).
Giralt, A. et al. Increased PKA signaling disrupts recognition memory and spatial memory: role in Huntington’s disease. Hum. Mol. Genet. 20, 4232–4247 (2011).
Varani, K. et al. Biological abnormalities of peripheral A(2A) receptors in a large representation of polyglutamine disorders and Huntington’s disease stages. Neurobiol. Dis. 27, 36–43 (2007).
Varani, K. et al. Aberrant amplification of A(2A) receptor signaling in striatal cells expressing mutant huntingtin. FASEB J. 15, 1245–1247 (2001).
Li, W. et al. Inactivation of adenosine A2A receptors reverses working memory deficits at early stages of Huntington’s disease models. Neurobiol. Dis. 79, 70–80 (2015).
Chen, J.Y., Wang, E.A., Cepeda, C. & Levine, M.S. Dopamine imbalance in Huntington’s disease: a mechanism for the lack of behavioral flexibility. Front. Neurosci. 7, 114 (2013).
Cummings, D.M. et al. Aberrant cortical synaptic plasticity and dopaminergic dysfunction in a mouse model of Huntington’s disease. Hum. Mol. Genet. 15, 2856–2868 (2006).An interesting study suggesting that alterations in dopaminergic signaling underlie early cortical dysfunction in synaptic plasticity in a genetic model of HD.
Murmu, R.P., Li, W., Holtmaat, A. & Li, J.Y. Dendritic spine instability leads to progressive neocortical spine loss in a mouse model of Huntington’s disease. J. Neurosci. 33, 12997–13009 (2013).
Mazzocchi-Jones, D., Döbrössy, M. & Dunnett, S.B. Embryonic striatal grafts restore bi-directional synaptic plasticity in a rodent model of Huntington’s disease. Eur. J. Neurosci. 30, 2134–2142 (2009).This study demonstrates that embryonic striatal grafts form functional connections with the host striatal circuitry that are capable of restoring bidirectional synaptic plasticity, similar to that in the normal corticostriatal circuit, in an excitotoxic lesion model of Huntington’s disease.
Albanese, A. et al. Phenomenology and classification of dystonia: a consensus update. Mov. Disord. 28, 863–873 (2013).
Goodchild, R.E., Grundmann, K. & Pisani, A. New genetic insights highlight 'old' ideas on motor dysfunction in dystonia. Trends Neurosci. 36, 717–725 (2013).
Ozelius, L.J. et al. The early-onset torsion dystonia gene (DYT1) encodes an ATP-binding protein. Nat. Genet. 17, 40–48 (1997).
Martella, G. et al. Impairment of bidirectional synaptic plasticity in the striatum of a mouse model of DYT1 dystonia: role of endogenous acetylcholine. Brain 132, 2336–2349 (2009).This study demonstrates the loss of LTD and of synaptic depotentiation in a genetic model of DYT1 dystonia.
Grundmann, K. et al. Generation of a novel rodent model for DYT1 dystonia. Neurobiol. Dis. 47, 61–74 (2012).
Martella, G. et al. Regional specificity of synaptic plasticity deficits in a knock-in mouse model of DYT1 dystonia. Neurobiol. Dis. 65, 124–132 (2014).
Breakefield, X.O. et al. The pathophysiological basis of dystonias. Nat. Rev. Neurosci. 9, 222–234 (2008).
Pisani, A., Bernardi, G., Ding, J. & Surmeier, D.J. Re-emergence of striatal cholinergic interneurons in movement disorders. Trends Neurosci. 30, 545–553 (2007).
Sciamanna, G. et al. Cholinergic dysfunction alters synaptic integration between thalamostriatal and corticostriatal inputs in DYT1 dystonia. J. Neurosci. 32, 11991–12004 (2012).
Sciamanna, G. et al. Developmental profile of the aberrant dopamine D2 receptor response in striatal cholinergic interneurons in DYT1 dystonia. PLoS One 6, e24261 (2011).
Napolitano, F. et al. Dopamine D2 receptor dysfunction is rescued by adenosine A2A receptor antagonism in a model of DYT1 dystonia. Neurobiol. Dis. 38, 434–445 (2010).
Dang, M.T. et al. An anticholinergic reverses motor control and corticostriatal LTD deficits in Dyt1 ΔGAG knock-in mice. Behav. Brain Res. 226, 465–472 (2012).
Pappas, S.S. et al. Forebrain deletion of the dystonia protein torsinA causes dystonic-like movements and loss of striatal cholinergic neurons. eLife 4, e08352 (2015).
Eskow Jaunarajs, K.L., Bonsi, P., Chesselet, M.F., Standaert, D.G. & Pisani, A. Striatal cholinergic dysfunction as a unifying theme in the pathophysiology of dystonia. Prog. Neurobiol. 127-128, 91–107 (2015).
Fahn, S. The medical treatment of Parkinson disease from James Parkinson to George Cotzias. Mov. Disord. 30, 4–18 (2015).
Picconi, B. et al. Loss of bidirectional striatal synaptic plasticity in l-DOPA-induced dyskinesia. Nat. Neurosci. 6, 501–506 (2003).This study demonstrates that striatal LTP induced by high frequency stimulation of glutamatergic inputs in parkinsonian dyskinetic rats is not reversed by a depotentiation protocol, suggesting that abnormal information storage in corticostriatal synapses is linked with the development of l-DOPA-induced dyskinesia.
Cerovic, M. et al. Derangement of Ras-guanine nucleotide-releasing factor 1 (Ras-GRF1) and extracellular signal-regulated kinase (ERK) dependent striatal plasticity in l-DOPA-induced dyskinesia. Biol. Psychiatry 77, 106–115 (2015).
Picconi, B. et al. Inhibition of phosphodiesterases rescues striatal long-term depression and reduces levodopa-induced dyskinesia. Brain 134, 375–387 (2011).
Ghiglieri, V. et al. Modulation of serotonergic transmission by eltoprazine in l-DOPA-induced dyskinesia: Behavioral, molecular, and synaptic mechanisms. Neurobiol. Dis. 86, 140–153 (2016).
Thiele, S.L. et al. Selective loss of bi-directional synaptic plasticity in the direct and indirect striatal output pathways accompanies generation of parkinsonism and l-DOPA induced dyskinesia in mouse models. Neurobiol. Dis. 71, 334–344 (2014).
Fieblinger, T. et al. Cell type-specific plasticity of striatal projection neurons in parkinsonism and l-DOPA-induced dyskinesia. Nat. Commun. 5, 5316 (2014).
Dumas, E.M. et al. Early changes in white matter pathways of the sensorimotor cortex in premanifest Huntington’s disease. Hum. Brain Mapp. 33, 203–212 (2012).
Rioult-Pedotti, M.S., Pekanovic, A., Atiemo, C.O., Marshall, J. & Luft, A.R. Dopamine promotes motor cortex plasticity and motor skill learning via PLC activation. PLoS One 10, e0124986 (2015).
Ziemann, U. et al. Consensus: motor cortex plasticity protocols. Brain Stimul. 1, 164–182 (2008).This important article critically analyzes the properties of the various stimulation protocols used in clinical neurophysiology and their particular strengths and weaknesses.
Abbruzzese, G. et al. Intracortical inhibition and facilitation are abnormal in Huntington’s disease: a paired magnetic stimulation study. Neurosci. Lett. 228, 87–90 (1997).
Priori, A., Berardelli, A., Inghilleri, M., Polidori, L. & Manfredi, M. Electromyographic silent period after transcranial brain stimulation in Huntington’s disease. Mov. Disord. 9, 178–182 (1994).
Tegenthoff, M., Vorgerd, M., Juskowiak, F., Roos, V. & Malin, J.P. Postexcitatory inhibition after transcranial magnetic single and double brain stimulation in Huntington’s disease. Electroencephalogr. Clin. Neurophysiol. 101, 298–303 (1996).
Schippling, S. et al. Abnormal motor cortex excitability in preclinical and very early Huntington’s disease. Biol. Psychiatry 65, 959–965 (2009).
Crupi, D. et al. Cortical and brainstem LTP-like plasticity in Huntington’s disease. Brain Res. Bull. 75, 107–114 (2008).
Lorenzano, C. et al. Motor cortical excitability studied with repetitive transcranial magnetic stimulation in patients with Huntington’s disease. Clin. Neurophysiol. 117, 1677–1681 (2006).
Orth, M. et al. Abnormal motor cortex plasticity in premanifest and very early manifest Huntington disease. J. Neurol. Neurosurg. Psychiatry 81, 267–270 (2010).
Espay, A.J. et al. Cortical and spinal abnormalities in psychogenic dystonia. Ann. Neurol. 59, 825–834 (2006).
Huang, Y.Z., Rothwell, J.C., Lu, C.S., Wang, J. & Chen, R.S. Restoration of motor inhibition through an abnormal premotor-motor connection in dystonia. Mov. Disord. 25, 696–703 (2010).
Ridding, M.C., Sheean, G., Rothwell, J.C., Inzelberg, R. & Kujirai, T. Changes in the balance between motor cortical excitation and inhibition in focal, task specific dystonia. J. Neurol. Neurosurg. Psychiatry 59, 493–498 (1995).
Brighina, F. et al. Effects of cerebellar TMS on motor cortex of patients with focal dystonia: a preliminary report. Exp. Brain Res. 192, 651–656 (2009).
Stinear, C.M. & Byblow, W.D. Impaired inhibition of a pre-planned response in focal hand dystonia. Exp. Brain Res. 158, 207–212 (2004).
Chen, R. & Hallett, M. Focal dystonia and repetitive motion disorders. Clin. Orthop. Relat. Res. (351): 102–106 (1998).
Kimberley, T.J. et al. Establishing the definition and inter-rater reliability of cortical silent period calculation in subjects with focal hand dystonia and healthy controls. Neurosci. Lett. 464, 84–87 (2009).
Kojovic, M. et al. Secondary and primary dystonia: pathophysiological differences. Brain 136, 2038–2049 (2013).
Sohn, Y.H. & Hallett, M. Disturbed surround inhibition in focal hand dystonia. Ann. Neurol. 56, 595–599 (2004).
Koch, G. et al. Altered dorsal premotor-motor interhemispheric pathway activity in focal arm dystonia. Mov. Disord. 23, 660–668 (2008).
Quartarone, A. et al. Abnormal associative plasticity of the human motor cortex in writer’s cramp. Brain 126, 2586–2596 (2003).
Weise, D. et al. The two sides of associative plasticity in writer’s cramp. Brain 129, 2709–2721 (2006).
Edwards, M.J., Huang, Y.Z., Mir, P., Rothwell, J.C. & Bhatia, K.P. Abnormalities in motor cortical plasticity differentiate manifesting and nonmanifesting DYT1 carriers. Mov. Disord. 21, 2181–2186 (2006).
Tamura, Y. et al. Disordered plasticity in the primary somatosensory cortex in focal hand dystonia. Brain 132, 749–755 (2009).
Tisch, S. et al. Pallidal stimulation modifies after-effects of paired associative stimulation on motor cortex excitability in primary generalised dystonia. Exp. Neurol. 206, 80–85 (2007).
Ruge, D. et al. Shaping reversibility? Long-term deep brain stimulation in dystonia: the relationship between effects on electrophysiology and clinical symptoms. Brain 134, 2106–2115 (2011).
Sadnicka, A., Hamada, M., Bhatia, K.P., Rothwell, J.C. & Edwards, M.J. A reflection on plasticity research in writing dystonia. Mov. Disord. 29, 980–987 (2014).
Quartarone, A. et al. Abnormal sensorimotor plasticity in organic but not in psychogenic dystonia. Brain 132, 2871–2877 (2009).This seminal work shows that abnormal plasticity is a hallmark of organic dystonia while dystonia of psychogenic origin is characterized by normal plasticity.
Kang, J.S., Terranova, C., Hilker, R., Quartarone, A. & Ziemann, U. Deficient homeostatic regulation of practice-dependent plasticity in writer’s cramp. Cereb. Cortex 21, 1203–1212 (2011).
Quartarone, A. et al. Homeostatic-like plasticity of the primary motor hand area is impaired in focal hand dystonia. Brain 128, 1943–1950 (2005).
Morgante, F., Espay, A.J., Gunraj, C., Lang, A.E. & Chen, R. Motor cortex plasticity in Parkinson’s disease and levodopa-induced dyskinesias. Brain 129, 1059–1069 (2006).
Huang, Y.Z., Rothwell, J.C., Lu, C.S., Chuang, W.L. & Chen, R.S. Abnormal bidirectional plasticity-like effects in Parkinson’s disease. Brain 134, 2312–2320 (2011).This study, using a clinical neurophysiological approach, demonstrates that depotentiation is abnormal in the motor cortex of people with Parkinson’s disease with levodopa-induced dyskinesias.
Fasano, A. & Lozano, A.M. Deep brain stimulation for movement disorders: 2015 and beyond. Curr. Opin. Neurol. 28, 423–436 (2015).
Prescott, I.A. et al. Levodopa enhances synaptic plasticity in the substantia nigra pars reticulata of Parkinson’s disease patients. Brain 132, 309–318 (2009).
Prescott, I.A. et al. Lack of depotentiation at basal ganglia output neurons in PD patients with levodopa-induced dyskinesia. Neurobiol. Dis. 71, 24–33 (2014).This study, performed in people with dyskinesia implanted with electrodes for DBS, demonstrates impaired depotentiation in basal ganglia output nuclei. It is an important validation of the animal models of levodopa-induced dyskinesia.
Fox, M.D. & Alterman, R.L. Brain stimulation for torsion dystonia. JAMA Neurol. 72, 713–719 (2015).
Barow, E. et al. Deep brain stimulation suppresses pallidal low frequency activity in patients with phasic dystonic movements. Brain 137, 3012–3024 (2014).
Ruge, D. et al. Deep brain stimulation effects in dystonia: time course of electrophysiological changes in early treatment. Mov. Disord. 26, 1913–1921 (2011).
Prescott, I.A. et al. Reduced paired pulse depression in the basal ganglia of dystonia patients. Neurobiol. Dis. 51, 214–221 (2013).
Sharma, M. & Deogaonkar, M. Deep brain stimulation in Huntington’s disease: assessment of potential targets. J. Clin. Neurosci. 22, 812–817 (2015).
Chou, Y.H., Hickey, P.T., Sundman, M., Song, A.W. & Chen, N.K. Effects of repetitive transcranial magnetic stimulation on motor symptoms in Parkinson disease: a systematic review and meta-analysis. JAMA Neurol. 72, 432–440 (2015).
Udupa, K. & Chen, R. Motor cortical plasticity in Parkinson’s disease. Front. Neurol. 4, 128 (2013).
Lefaucheur, J.P. et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin. Neurophysiol. 125, 2150–2206 (2014).
Koch, G. et al. rTMS of supplementary motor area modulates therapy-induced dyskinesias in Parkinson disease. Neurology 65, 623–625 (2005).This study shows that rTMS at 1 Hz markedly reduced drug-induced dyskinesias, whereas stimulation at 5 Hz did not affect it, suggesting possible therapeutic effects only of stimulation frequencies able to induce synaptic depotentiation.
Filipović, S.R., Rothwell, J.C., van de Warrenburg, B.P. & Bhatia, K. Repetitive transcranial magnetic stimulation for levodopa-induced dyskinesias in Parkinson’s disease. Mov. Disord. 24, 246–253 (2009).
Koch, G. et al. Cerebellar magnetic stimulation decreases levodopa-induced dyskinesias in Parkinson disease. Neurology 73, 113–119 (2009).
Cerasa, A. et al. A network centred on the inferior frontal cortex is critically involved in levodopa-induced dyskinesias. Brain 138, 414–427 (2015).
Ceballos-Baumann, A.O. et al. Overactive prefrontal and underactive motor cortical areas in idiopathic dystonia. Ann. Neurol. 37, 363–372 (1995).
Brusa, L. et al. Improvement of choreic movements by 1 Hz repetitive transcranial magnetic stimulation in Huntington’s disease patients. Ann. Neurol. 58, 655–656 (2005).
Shukla, A., Jayarajan, R.N., Muralidharan, K. & Jain, S. Repetitive transcranial magnetic stimulation not beneficial in severe choreiform movements of Huntington disease. J. ECT 29, e16–e17 (2013).
Moisello, C. et al. TMS enhances retention of a motor skill in Parkinson’s disease. Brain Stimul. 8, 224–230 (2015).
Udupa, K. et al. Cortical plasticity induction by pairing subthalamic nucleus deep-brain stimulation and primary motor cortical transcranial magnetic stimulation in Parkinson’s disease. J. Neurosci. 36, 396–404 (2016).
Acknowledgements
This work was supported by grants from Progetto di Ricerca di Interesse Nazionale (PRIN) 2011 (prot. 2010AHHP5H) (to A.P. and P.C.), Fondazione Cariplo, grant no. 2014-0660 (to P.C.), Italian Ministry of Education, University and Research, FIRB Call Program “Futuro in Ricerca” Project no. RBFR13S4LE_002 (to V.G.) and from the Italian Ministry of Health, Ricerca Finalizzata and Giovani Ricercatori (GR-2010-2316671 to V.G., RF-2013-02357386 to B.P. and RF-2013-02356215 to P.C.).
Author information
Authors and Affiliations
Contributions
A.P., J.A.O., J.R. and P.C. conceived and planned the Perspective. P.C. wrote the first draft of the Perspective. All authors contributed to the discussion and edited the Perspective. B.P. and V.G. edited the manuscript and made the figures.
Ethics declarations
Competing interests
P.C. receives research support from Bayer Schering, Biogen, Merck Sharp & Dohme, Sanofi-Aventis, and UCB Pharma.
Rights and permissions
About this article
Cite this article
Calabresi, P., Pisani, A., Rothwell, J. et al. Hyperkinetic disorders and loss of synaptic downscaling. Nat Neurosci 19, 868–875 (2016). https://doi.org/10.1038/nn.4306
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nn.4306
This article is cited by
-
Slow wave activity across sleep-night could predict levodopa-induced dyskinesia
Scientific Reports (2023)
-
Cerebellar stimulation prevents Levodopa-induced dyskinesia in mice and normalizes activity in a motor network
Nature Communications (2022)
-
Impairment of sleep homeostasis in cervical dystonia patients
Scientific Reports (2022)
-
Range of voluntary neck motility predicts outcome of pallidal DBS for cervical dystonia
Acta Neurochirurgica (2019)
-
Dystonia
Nature Reviews Disease Primers (2018)