Abstract
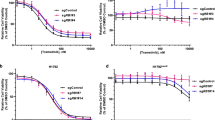
One strategy for combating cancer-drug resistance is to deploy rational polytherapy up front that suppresses the survival and emergence of resistant tumor cells. Here we demonstrate in models of lung adenocarcinoma harboring the oncogenic fusion of ALK and EML4 that the GTPase RAS–mitogen-activated protein kinase (MAPK) pathway, but not other known ALK effectors, is required for tumor-cell survival. EML4-ALK activated RAS-MAPK signaling by engaging all three major RAS isoforms through the HELP domain of EML4. Reactivation of the MAPK pathway via either a gain in the number of copies of the gene encoding wild-type K-RAS (KRASWT) or decreased expression of the MAPK phosphatase DUSP6 promoted resistance to ALK inhibitors in vitro, and each was associated with resistance to ALK inhibitors in individuals with EML4-ALK–positive lung adenocarcinoma. Upfront inhibition of both ALK and the kinase MEK enhanced both the magnitude and duration of the initial response in preclinical models of EML4-ALK lung adenocarcinoma. Our findings identify RAS-MAPK dependence as a hallmark of EML4-ALK lung adenocarcinoma and provide a rationale for the upfront inhibition of both ALK and MEK to forestall resistance and improve patient outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Solomon, B.J. et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N. Engl. J. Med. 371, 2167–2177 (2014).
Shaw, A.T. et al. Ceritinib in ALK-rearranged non-small-cell lung cancer. N. Engl. J. Med. 370, 1189–1197 (2014).
Camidge, D.R. & Doebele, R.C. Treating ALK-positive lung cancer—early successes and future challenges. Nat. Rev. Clin. Oncol. 9, 268–277 (2012).
Shaw, A.T. et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N. Engl. J. Med. 368, 2385–2394 (2013).
Robert, C. et al. Improved overall survival in melanoma with combined dabrafenib and trametinib. N. Engl. J. Med. 372, 30–39 (2015).
Chapman, P.B., Solit, D.B. & Rosen, N. Combination of RAF and MEK inhibition for the treatment of BRAF-mutated melanoma: feedback is not encouraged. Cancer Cell 26, 603–604 (2014).
Johnson, D.B. et al. Combined BRAF (Dabrafenib) and MEK inhibition (Trametinib) in patients with BRAFV600E-mutant melanoma experiencing progression with single-agent BRAF inhibitor. J. Clin. Oncol. 32, 3697–3704 (2014).
Flaherty, K.T. et al. Combined BRAF and MEK inhibition in melanoma with BRAF V600 mutations. N. Engl. J. Med. 367, 1694–1703 (2012).
Long, G.V. et al. Combined BRAF and MEK inhibition versus BRAF inhibition alone in melanoma. N. Engl. J. Med. 371, 1877–1888 (2014).
Lemmon, M.A. & Schlessinger, J. Cell signaling by receptor tyrosine kinases. Cell 141, 1117–1134 (2010).
The Cancer Genome Atlas Research Network. Comprehensive molecular profiling of lung adenocarcinoma. Nature 511, 543–550 (2014).
Lovly, C.M. et al. Rationale for co-targeting IGF-1R and ALK in ALK fusion- positive lung cancer. Nat. Med. 20, 1027–1034 (2014).
Alessandrini, A. et al. Mek1 phosphorylation site mutants activate Raf-1 in NIH 3T3 cells. J. Biol. Chem. 271, 31612–31618 (1996).
Takezawa, K. et al. Role of ERK-BIM and STAT3-survivin signaling pathways in ALK inhibitor-induced apoptosis in EML4-ALK-positive lung cancer. Clin. Cancer Res. 17, 2140–2148 (2011).
Hainsworth, J.D. et al. A phase II, open-label, randomized study to assess the efficacy and safety of AZD6244 (ARRY-142886) versus pemetrexed in patients with non-small cell lung cancer who have failed one or two prior chemotherapeutic regimens. J. Thorac. Oncol. 5, 1630–1636 (2010).
Bivona, T.G. et al. Phospholipase Cγ activates Ras on the Golgi apparatus by means of RasGRP1. Nature 424, 694–698 (2003).
Grabocka, E. et al. Wild-type H- and N-Ras promote mutant K-Ras-driven tumorigenesis by modulating the DNA damage response. Cancer Cell 25, 243–256 (2014).
Hancock, J.F. Ras proteins: different signals from different locations. Nat. Rev. Mol. Cell Biol. 4, 373–384 (2004).
Bivona, T.G. & Philips, M.R. Ras pathway signaling on endomembranes. Curr. Opin. Cell Biol. 15, 136–142 (2003).
Mano, H. ALKoma: a cancer subtype with a shared target. Cancer Discov. 2, 495–502 (2012).
Shaw, A.T. & Solomon, B. Targeting anaplastic lymphoma kinase in lung cancer. Clin. Cancer Res. 17, 2081–2086 (2011).
Soda, M. et al. Identification of the transforming EML4-ALK fusion gene in non- small-cell lung cancer. Nature 448, 561–566 (2007).
Richards, M.W. et al. Crystal structure of EML1 reveals the basis for Hsp90 dependence of oncogenic EML4-ALK by disruption of an atypical B-propeller domain. Proc. Natl. Acad. Sci. USA 111, 5195–5200 (2014).
Pollmann, M. et al. Human EML4, a novel member of the EMAP family, is essential for microtubule formation. Exp. Cell Res. 312, 3241–3251 (2006).
Choi, Y.L. et al. Identification of novel isoforms of the EML4-ALK transforming gene in non-small cell lung cancer. Cancer Res. 68, 4971–4976 (2008).
Shimizu, T. et al. The clinical effect of the dual-targeting strategy involving PI3K/AKT/mTOR and RAS/MEK/ERK pathways in patients with advanced cancer. Clin. Cancer Res. 18, 2316–2325 (2012).
Zhao, Y.S. & Adjei, A.A. The clinical development of MEK inhibitors. Nat Rev Clin Oncol. 11, 385–400 (2014).
Katayama, R. et al. Mechanisms of acquired crizotinib resistance in ALK- rearranged lung cancers. Sci. Transl. Med. 4, 120ra117 (2012).
Pfister, S. et al. BRAF gene duplication constitutes a mechanism of MAPK pathway activation in low-grade astrocytomas. J. Clin. Invest. 118, 1739–1749 (2008).
Graham, J.M. Jr. et al. Genomic duplication of PTPN11 is an uncommon cause of Noonan syndrome. Am. J. Med. Genet. 149A, 2122–2128 (2009).
Caunt, C.J. & Keyse, S.M. Dual-specificity MAP kinase phosphatase (MKPs): shaping the outcome of MAP kinase signaling. FEBS J. 280, 489–504 (2013).
Ercan, D. et al. Reactivation of ERK signaling causes resistance to EGFR kinase inhibitors. Cancer Discov. 2, 934–947 (2012).
Wilson, T.R. et al. Widespread potential for growth factor-driven resistance to anticancer kinase inhibitors. Nature 487, 505–509 (2012).
Huang, S. et al. MED12 controls the response to multiple cancer drugs through regulation of TGF-B signaling. Cell 151, 937–950 (2012).
Crystal, A.S. et al. Patient-derived models of acquired resistance can identify effective drug combinations for cancer. Science 346, 1480–1486 (2014).
Nissan, M.H. et al. Loss of NF1 in cutaneous melanoma is associated with RAS activation and MEK dependence. Cancer Res. 74, 430–2350 (2014).
Esfahani, K., Agulnik, J.S. & Cohen, V. A systemic review of resistance mechanisms and ongoing clinical trials in ALK-rearranged non-small cell lung cancer. Front Oncol. 4, 174 (2014).
Doebele, R.C. et al. Mechanisms of resistance to crizotinib in patients with ALK gene rearranged non-small cell lung cancer. Clin. Cancer Res. 18, 1472–1482 (2012).
Wilson, F.H. et al. A Functional landscape of resistance to ALK inhibition in lung cancer. Cancer Cell 27, 397–408 (2015).
Tanizaki, J. et al. Combined effect of ALK and MEK inhibitors in EML4-ALK-positive non-small-cell lung cancer cells. Br. J. Cancer 106, 763–767 (2012).
Lin, L. et al. Mapping the molecular determinants of BRAF oncogene dependence in human lung cancer. Proc. Natl. Acad. Sci. USA 111, E748–E757 (2014).
Camidge, D.R. et al. Optimizing the detection of lung cancer patients harboring anaplastice lymphoma kinase (ALK) gene rearrangements potentially suitable for ALK inhibitor treatment. Clin. Cancer Res. 16, 5581–5590 (2010).
Acknowledgements
We thank M. McMahon, F. McCormick, K. Shannon and M. Von Zastrow (UCSF) for advice and discussions, and H. Mano (University of Tokyo) for EML4-ALK cDNA constructs and for advice. We acknowledge funding support from the following sources: a US National Institute of Health (NIH) Director's New Innovator Award, the Howard Hughes Medical Institute, the Doris Duke Charitable Foundation, the American Lung Association, the National Lung Cancer Partnership, the Sidney Kimmel Foundation for Cancer Research and the Searle Scholars Program (T.G.B.); the UCSF Clinical and Translational Science Institute (G.H.); the National Cancer Institute (NCI) of the NIH (R01CA121210 and P01CA129243), a Damon Runyon Clinical Investigator Award and a LUNGevity Career Development Award (C.M.L.); the NIH (NCI5K12CA086913) (R.C.D.); an NIH Paul Calabresi Cancer Development Award in Clinical Oncology (K12CA138464) (J.W.R.); the NIH (NCI-P30CA046934) and Lung Cancer SPORE (NCI-P50CA058187) (M.V.G.); and the La Caixa Foundation and Redes Temáticas de Investigación en Cáncer (RD12/0036/0072) (R.R.).
Author information
Authors and Affiliations
Contributions
G.H. contributed to the design, conduct and interpretation of all experiments; V.O. contributed in vivo experiments; E.P., A.T., C.M.B., R.A.O., D.S.N., E.C., A.S. and A.V. contributed cell line experiments and aided in experimental design; S.A. contributed deep-sequencing analysis; L.L. contributed sequencing library preparation; J.F., M.V.-G., D.L.A. and R.C.D. contributed analysis of patient tumor data; S.-H.I.O., P.C.M., N.K., R.R., J.W.R. and R.C.D. contributed patient tumor samples and clinical data; E.A.C. contributed to experimental design and interpretation; E.I. and C.M.L. contributed patient-derived cell lines and conducted experiments; T.G.B. supervised the project and contributed to the design and interpretation of all experiments; and G.H. and T.G.B. wrote the manuscript with input from all co-authors.
Corresponding author
Ethics declarations
Competing interests
T.G.B. is a consultant to Driver Group, Novartis, Clovis Oncology, Natera and Genoptix and is the recipient of a research grant from Servier, all of which are each engaged in cancer diagnostics and/or treatment.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–10 (PDF 8873 kb)
Rights and permissions
About this article
Cite this article
Hrustanovic, G., Olivas, V., Pazarentzos, E. et al. RAS-MAPK dependence underlies a rational polytherapy strategy in EML4-ALK–positive lung cancer. Nat Med 21, 1038–1047 (2015). https://doi.org/10.1038/nm.3930
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.3930
This article is cited by
-
The role of APOBEC3B in lung tumor evolution and targeted cancer therapy resistance
Nature Genetics (2024)
-
ALK-positive lung cancer: a moving target
Nature Cancer (2023)
-
Rational combinations of targeted cancer therapies: background, advances and challenges
Nature Reviews Drug Discovery (2023)
-
EML4-ALK fusion protein in Lung cancer cells enhances venous thrombogenicity through the pERK1/2-AP-1-tissue factor axis
Journal of Thrombosis and Thrombolysis (2023)
-
Molecular pathways, resistance mechanisms and targeted interventions in non-small-cell lung cancer
Molecular Biomedicine (2022)