Abstract
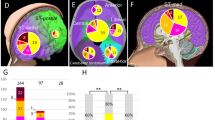
Meningiomas are the most common primary nervous system tumor. The tumor suppressor NF2 is disrupted in approximately half of all meningiomas1, but the complete spectrum of genetic changes remains undefined. We performed whole-genome or whole-exome sequencing on 17 meningiomas and focused sequencing on an additional 48 tumors to identify and validate somatic genetic alterations. Most meningiomas had simple genomes, with fewer mutations, rearrangements and copy-number alterations than reported in other tumors in adults. However, several meningiomas harbored more complex patterns of copy-number changes and rearrangements, including one tumor with chromothripsis. We confirmed focal NF2 inactivation in 43% of tumors and found alterations in epigenetic modifiers in an additional 8% of tumors. A subset of meningiomas lacking NF2 alterations harbored recurrent oncogenic mutations in AKT1 (p.Glu17Lys) and SMO (p.Trp535Leu) and exhibited immunohistochemical evidence of activation of these pathways. These mutations were present in therapeutically challenging tumors of the skull base and higher grade. These results begin to define the spectrum of genetic alterations in meningiomas and identify potential therapeutic targets.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Choy, W. et al. The molecular genetics and tumor pathogenesis of meningiomas and the future directions of meningioma treatments. Neurosurg. Focus 30, E6 (2011).
van Alkemade, H. et al. Impaired survival and long-term neurological problems in benign meningioma. Neuro-oncol. 14, 658–666 (2012).
Durand, A. et al. WHO grade II and III meningiomas: a study of prognostic factors. J. Neurooncol. 95, 367–375 (2009).
Perry, A., Scheithauer, B.W., Stafford, S.L., Lohse, C.M. & Wollan, P.C. “Malignancy” in meningiomas: a clinicopathologic study of 116 patients, with grading implications. Cancer 85, 2046–2056 (1999).
Goutagny, S. et al. Genomic profiling reveals alternative genetic pathways of meningioma malignant progression dependent on the underlying NF2 status. Clin. Cancer Res. 16, 4155–4164 (2010).
Krayenbühl, N., Pravdenkova, S. & Al-Mefty, O. De novo versus transformed atypical and anaplastic meningiomas: comparisons of clinical course, cytogenetics, cytokinetics, and outcome. Neurosurgery 61, 495–503, discussion 503–504 (2007).
Wen, P.Y., Quant, E., Drappatz, J., Beroukhim, R. & Norden, A.D. Medical therapies for meningiomas. J. Neurooncol. 99, 365–378 (2010).
Bass, A.J. et al. Genomic sequencing of colorectal adenocarcinomas identifies a recurrent VTI1A-TCF7L2 fusion. Nat. Genet. 43, 964–968 (2011).
Berger, M.F. et al. Melanoma genome sequencing reveals frequent PREX2 mutations. Nature 485, 502–506 (2012).
Berger, M.F. et al. The genomic complexity of primary human prostate cancer. Nature 470, 214–220 (2011).
Chapman, M.A. et al. Initial genome sequencing and analysis of multiple myeloma. Nature 471, 467–472 (2011).
Stransky, N. et al. The mutational landscape of head and neck squamous cell carcinoma. Science 333, 1157–1160 (2011).
Lohr, J.G. et al. Discovery and prioritization of somatic mutations in diffuse large B-cell lymphoma (DLBCL) by whole-exome sequencing. Proc. Natl. Acad. Sci. USA 109, 3879–3884 (2012).
Beroukhim, R. et al. The landscape of somatic copy-number alteration across human cancers. Nature 463, 899–905 (2010).
Greenman, C. et al. Patterns of somatic mutation in human cancer genomes. Nature 446, 153–158 (2007).
Mawrin, C. & Perry, A. Pathological classification and molecular genetics of meningiomas. J. Neurooncol. 99, 379–391 (2010).
Ketter, R. et al. Hyperdiploidy defines a distinct cytogenetic entity of meningiomas. J. Neurooncol. 83, 213–221 (2007).
Nunes, F. et al. Inactivation patterns of NF2 and DAL-1/4.1B (EPB41L3) in sporadic meningioma. Cancer Genet. Cytogenet. 162, 135–139 (2005).
Rausch, T. et al. Genome sequencing of pediatric medulloblastoma links catastrophic DNA rearrangements with TP53 mutations. Cell 148, 59–71 (2012).
Stephens, P.J. et al. Massive genomic rearrangement acquired in a single catastrophic event during cancer development. Cell 144, 27–40 (2011).
Takita, J. et al. Aberrations of NEGR1 on 1p31 and MYEOV on 11q13 in neuroblastoma. Cancer Sci. 102, 1645–1650 (2011).
Yang, H.W. et al. Alternative splicing of CHEK2 and codeletion with NF2 promote chromosomal instability in meningioma. Neoplasia 14, 20–28 (2012).
Kooistra, S.M. & Helin, K. Molecular mechanisms and potential functions of histone demethylases. Nat. Rev. Mol. Cell Biol. 13, 297–311 (2012).
Hadfield, K.D. et al. Molecular characterisation of SMARCB1 and NF2 in familial and sporadic schwannomatosis. J. Med. Genet. 45, 332–339 (2008).
Schmitz, U. et al. INI1 mutations in meningiomas at a potential hotspot in exon 9. Br. J. Cancer 84, 199–201 (2001).
Tsurusaki, Y. et al. Mutations affecting components of the SWI/SNF complex cause Coffin-Siris syndrome. Nat. Genet. 44, 376–378 (2012).
Reifenberger, J. et al. Missense mutations in SMOH in sporadic basal cell carcinomas of the skin and primitive neuroectodermal tumors of the central nervous system. Cancer Res. 58, 1798–1803 (1998).
Jones, D.T. et al. Dissecting the genomic complexity underlying medulloblastoma. Nature 488, 100–105 (2012).
Laurendeau, I. et al. Gene expression profiling of the hedgehog signaling pathway in human meningiomas. Mol. Med. 16, 262–270 (2010).
Aavikko, M. et al. Loss of SUFU function in familial multiple meningioma. Am. J. Hum. Genet. 91, 520–526 (2012).
Gorlin, R.J. Nevoid basal-cell carcinoma syndrome. Medicine (Baltimore) 66, 98–113 (1987).
Santos, D.C. et al. PTCH1 gene mutations in exon 17 and loss of heterozygosity on D9S180 microsatellite in sporadic and inherited human basal cell carcinomas. Int. J. Dermatol. 50, 838–843 (2011).
Bleeker, F.E. et al. AKT1E17K in human solid tumours. Oncogene 27, 5648–5650 (2008).
Wellenreuther, R. et al. Analysis of the neurofibromatosis 2 gene reveals molecular variants of meningioma. Am. J. Pathol. 146, 827–832 (1995).
Mathiesen, T., Lindquist, C., Kihlstrom, L. & Karlsson, B. Recurrence of cranial base meningiomas. Neurosurgery 39, 2–7, discussion 8–9 (1996).
Ellison, D.W. et al. Medulloblastoma: clinicopathological correlates of SHH, WNT, and non-SHH/WNT molecular subgroups. Acta Neuropathol. 121, 381–396 (2011).
Karst, A.M. et al. Stathmin 1, a marker of PI3K pathway activation and regulator of microtubule dynamics, is expressed in early pelvic serous carcinomas. Gynecol. Oncol. 123, 5–12 (2011).
Riobó, N.A., Lu, K., Ai, X., Haines, G.M. & Emerson, C.P. Jr. Phosphoinositide 3-kinase and Akt are essential for Sonic Hedgehog signaling. Proc. Natl. Acad. Sci. USA 103, 4505–4510 (2006).
Von Hoff, D.D. et al. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N. Engl. J. Med. 361, 1164–1172 (2009).
Janku, F. et al. PI3K/AKT/mTOR inhibitors in patients with breast and gynecologic malignancies harboring PIK3CA mutations. J. Clin. Oncol. 30, 777–782 (2012).
Parsons, D.W. et al. An integrated genomic analysis of human glioblastoma multiforme. Science 321, 1807–1812 (2008).
Samuels, Y. et al. High frequency of mutations of the PIK3CA gene in human cancers. Science 304, 554 (2004).
Demichelis, F. et al. SNP panel identification assay (SPIA): a genetic-based assay for the identification of cell lines. Nucleic Acids Res. 36, 2446–2456 (2008).
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25, 1754–1760 (2009).
DePristo, M.A. et al. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nat. Genet. 43, 491–498 (2011).
McKenna, A. et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303 (2010).
Reich, M. et al. GenePattern 2.0. Nat. Genet. 38, 500–501 (2006).
Chiang, D.Y. et al. High-resolution mapping of copy-number alterations with massively parallel sequencing. Nat. Methods 6, 99–103 (2009).
Krzywinski, M. et al. Circos: an information aesthetic for comparative genomics. Genome Res. 19, 1639–1645 (2009).
1000 Genomes Project Consortium. A map of human genome variation from population-scale sequencing. Nature 467, 1061–1073 (2010).
Acknowledgements
The authors would like to thank M. Lawrence, N. Stransky, M. Imielinski, K. Cibulskis, S. Carter, C. Stewart, C.-Z. Zhang, Y. Drier, S. Schumacher and B. Tabak for their assistance with genomic analyses; P. Wen, O. Al-Mefty, T. Batchelor, B. Reisler, M. Johnson, W. Richards and J. Kim for their assistance with tissue acquisition; and A. Pisarek-Horowitz, S.A. Horowitz, G. Bergthold and C.H. Brastianos for critical review of the manuscript. This work was supported by the Brain Science Foundation (I.F.D., P.K.B., R.B. and S.S.), the Pediatric Low-Grade Astrocytoma Foundation (R.B. and W.C.H.), the American Brain Tumor Association (P.K.B.), a Conquer Cancer Foundation Young Investigator Award (P.K.B.), US National Institutes of Health (NIH) grants K08 CA122833 (R.B.), K08 NS064168 (S.S.) and K12 CA090354-11 (P.K.B.), and US Department of Defense grant W81XWH-12-1-0136 (P.M.H.).
Author information
Authors and Affiliations
Contributions
P.K.B., P.M.H., I.F.D., R.B. and W.C.H. conceived the study, designed the experiments, analyzed the data and wrote the manuscript. P.M.H. performed the bioinformatics analyses, and A.M., G.G., R.B. and M.D.D. provided analytical advice. S.S., A.O.S.-R. and D.N.L. reviewed the histopathology, and S.S. performed the immunohistochemistry. K.L.L. managed the tissue repository. R.T.J., E.P., P.V.H., A.R., A.S. and L.E.M. provided technical support and performed sequencing. W.C.H., I.F.D. and R.B. supervised the study. All authors discussed the results and implications and commented on the manuscript.
Corresponding authors
Ethics declarations
Competing interests
W.C.H. is a consultant for Blueprint Medicines and Thermo Fisher. R.B. is a shareholder for AstraZeneca. W.C.H. and R.B. are consultants for and receive research support from Novartis.
Supplementary information
Supplementary Text and Figures
Supplementary Note, Supplementary Tables 1 and 6 and Supplementary Figures 1–5 (PDF 6192 kb)
Supplementary Table 2
Genes sequenced in the Validation set (separate excel file) (XLSX 31 kb)
Supplementary Table 3
Rearrangements in WGS samples (separate excel file) (XLSX 25 kb)
Supplementary Table 4
All mutated genes and significance (separate excel file) (XLSX 29 kb)
Supplementary Table 5
Samples and their individual mutations (separate excel file) (XLSX 16 kb)
Rights and permissions
About this article
Cite this article
Brastianos, P., Horowitz, P., Santagata, S. et al. Genomic sequencing of meningiomas identifies oncogenic SMO and AKT1 mutations. Nat Genet 45, 285–289 (2013). https://doi.org/10.1038/ng.2526
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ng.2526
This article is cited by
-
Transcriptomic and epigenetic dissection of spinal ependymoma (SP-EPN) identifies clinically relevant subtypes enriched for tumors with and without NF2 mutation
Acta Neuropathologica (2024)
-
A novel BRAF::PTPRN2 fusion in meningioma: a case report
Acta Neuropathologica Communications (2023)
-
Review of meningioma diagnosis and management
Egyptian Journal of Neurosurgery (2023)
-
Meningioma animal models: a systematic review and meta-analysis
Journal of Translational Medicine (2023)
-
Somatic mutation landscape in a cohort of meningiomas that have undergone grade progression
BMC Cancer (2023)