Abstract
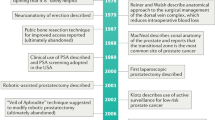
Men with prostate cancer have a variety of treatment choices available, including expectant management with deferred treatment, brachytherapy, external-beam radiation therapy, or both of the latter options—with or without hormonal therapy, cryotherapy, and radical prostatectomy (RP). Physicians have long endeavored to guide patients through these choices on the basis of the health threat posed by the cancer, the potential effectiveness and complications associated with treatment, and the patient's life expectancy. As early detection programs now identify cancers much earlier in their natural history, individual patients have a longer life expectancy than in the past. The patient and physician must, therefore, weigh the potential benefit of the selected treatment with the risk of early or delayed complications that would detract from the patient's quality of life. Optimally, when a surgical approach is used to treat prostate cancer, the operation removes the cancer completely with negative surgical margins, avoids excessive blood loss or serious perioperative complications, and culminates in complete recovery of continence and potency. To achieve this, the surgeon must treat sufficient periprostatic tissue to achieve cure while preserving the cavernosal nerves required for erectile function and the neuromusculature required for normal urinary and bowel function. Evidence suggests that the small details of how a surgery is performed have a major impact on the outcome of RP. Here the role of surgical techniques in determining oncologic and quality of life outcomes after RP, focusing on open RP, are presented.
Key Points
-
Oncologic and quality of life outcomes after radical prostatectomy are dependent on surgical technique; in order to achieve optimal outcomes for the patient, the surgeon must continually assess and reassess his/her results and modify the operation accordingly
-
While many of the operative steps of radical prostatectomy will be similar, the procedure must be individualized based on the features of the patient's cancer and his anatomy
-
One of the key aspects to performing a successful radical prostatectomy is reducing blood loss, as it provides a surgical field where visualization is improved and the fine details of neurovascular bundle preservation can be meticulously performed
-
Nerve-sparing radical prostatectomy is, in large part, neurosurgery; the neurovascular bundles are fragile and susceptible to excessive tension, thermal injury and direct damage, and techniques that minimize trauma to these delicate tissues should be used
-
The incidence of positive surgical margins can be reduced by excising as much periprostatic tissue as possible after the neurovascular bundles have been mobilized off the prostate; a deliberate incision through Denonvilliers' fascia and a sharp dissection of the prostate together with the fascial layer and some of the perirectal fat off the anterior rectal wall will best excise the periprostatic tissue
-
Even with complete bilateral nerve sparing, several millimeters of tissue can be resected adjacent to the majority of the gland
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Eastham JA et al. (1996) Risk factors for urinary incontinence after radical prostatectomy. J Urol 156: 1707–1713
Eastham JA and Scardino PT (2000) Radical prostatectomy for clinical stage T1 and T2 prostate cancer. In: Comprehensive Textbook of Genitourinary Oncology, 722–738 (Ed. Vogelzang N) Philadelphia: Lippincott Williams & Wilkins
Goad JR (1994) Modifications in the technique of radical prostatectomy to minimize blood loss. Atlas Urol Clin North Am 2: 65–80
Walsh PC (1998) Anatomic radical prostatectomy: evolution of the surgical technique. J Urol 160: 2418–2424
Begg CB et al. (2002) Variations in morbidity after radical prostatectomy. N Engl J Med 346: 1138–1144
Eastham JA et al. (2003) Variations among individual surgeons in the rate of positive surgical margins in radical prostatectomy specimens. J Urol 170: 2292–2295
Chang SS et al. (2004) Predicting blood loss and transfusion requirements during radical prostatectomy: the significant negative impact of increasing body mass index. J Urol 171:1861–1865
Shuford MD et al. (2004) Adverse prognostic significance of capsular incision with radical retropubic prostatectomy. J Urol 172: 119–123
Swindle P et al. (2005) Do margins matter? The prognostic significance of positive surgical margins in radical prostatectomy specimens. J Urol 174: 903–907
Karakiewicz PI et al. (2005) Prognostic impact of positive surgical margins in surgically treated prostate cancer: multi-institutional assessment of 5831 patients. Urology 66: 1245–1250
Walsh PC and Donker PJ (1982) Impotence following radical prostatectomy: insight into etiology and prevention. J Urol 128: 492–497
Quinlan DM et al. (1991) Sexual function following radical prostatectomy: influence of preservation of neurovascular bundles. J Urol 145: 998–1002
Rabbani F et al. (2000) Factors predicting recovery of erections after radical prostatectomy. J Urol 164: 1929–1934
Eichelberg C et al. (2007) Nerve distribution along the prostatic capsule. Eur Urol 51: 105–111
Costello AJ et al. (2004) Anatomical studies of the neurovascular bundle and cavernosal nerves. BJU Int 94: 1071–1076
Lunacek A et al. (2005) Anatomical radical retropubic prostatectomy: 'curtain dissection' of the neurovascular bundle. BJU Int 95: 1226–1231
Graefen M et al. (2006) Open retropubic nerve-sparing radical prostatectomy. Eur Urol 49: 38–48
Montorsi F et al. (2005) Improving the preservation of the urethral sphincter and neurovascular bundles during open radical retropubic prostatectomy. Eur Urol 48: 938–945
Sofer M et al. (2002) Positive surgical margins after radical retropubic prostatectomy: the influence of site and number on progression. J Urol 167: 2453–2456
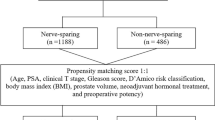
Ward JF et al. (2004) The impact of surgical approach (nerve bundle preservation versus wide local excision) on surgical margins and biochemical recurrence following radical prostatectomy. J Urol 172: 1328–1332
Palisaar RJ et al. (2005) Influence of nerve-sparing (NS) procedure during radical prostatectomy (RP) on margin status and biochemical failure. Eur Urol 47: 176–184
Ates M et al. (2007) Do tumor volume, tumor volume ratio, type of nerve sparing and surgical experience affect prostate specific antigen recurrence after laparoscopic radical prostatectomy? A matched pair analysis. J Urol 177: 1771–1776
Walsh PC et al. (1994) Cancer control and quality of life following anatomical radical retropubic prostatectomy: results at 10 years. J Urol 152: 1831–1836
Gao X et al. (2000) The extent of biopsy involvement as an independent predictor of extraprostatic extension and surgical margin status in low risk prostate cancer: implications for treatment selection. J Urol 164: 1982–1986
Partin AW et al. (2001) Contemporary update of prostate cancer staging nomograms (Partin Tables) for the new millennium. Urology 58: 843–848
Naya Y et al. (2004) Tumor length and location of cancer on biopsy predict side specific extraprostatic cancer extension. J Urol 171: 1093–1097
Tsuzuki T et al. (2005) Prediction of extraprostatic extension in the neurovascular bundle based on prostate needle biopsy pathology, serum prostate specific antigen and digital rectal examination. J Urol 173: 450–453
Walsh PC et al. (2000) Use of intraoperative video documentation to improve sexual function after radical retropubic prostatectomy. Urology 55: 62–67
Touijer K et al. (2005) Quality improvement in laparoscopic radical prostatectomy for pT2 prostate cancer: impact of video documentation review on positive surgical margin. J Urol 173: 765–768
Touijer K et al. (2006) Impact of a multidisciplinary continuous quality improvement program on the positive surgical margin rate after laparoscopic radical prostatectomy. Eur Urol 49: 853–858
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The author declares no competing financial interests.
Rights and permissions
About this article
Cite this article
Eastham, J. Surgery Insight: optimizing open nerve-sparing radical prostatectomy techniques for improved outcomes. Nat Rev Urol 4, 561–569 (2007). https://doi.org/10.1038/ncpuro0916
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpuro0916
This article is cited by
-
Robot-assisted versus open radical prostatectomy: a systematic review and meta-analysis of prospective studies
Journal of Robotic Surgery (2023)