Abstract
Age is well recognized as a powerful prognostic factor in the setting of cardiovascular disease. With the aging of the US population, it is projected that more than 50 million people will be aged over 65 years by the year 2020. This growing elderly population has increased rates of morbidity and mortality owing to cardiovascular disease; however, proven therapies for prevention and treatment are often underused in older patients, largely because physicians perceive them as being frail and have limited understanding of age-related unique adverse and therapeutic effects. Advancing age is associated with a number of physiologic and pathophysiologic changes that impact the toxic effects, efficacy and dosing of many medications. Decreases in lean muscle mass affect the volume of distribution, and reductions in hepatic function affect the metabolism of many medications. Age-related reductions in renal function might have the most profound impact on the safety profile and dosing of medications in elderly patients. The strong association between renal and cardiovascular disease makes recognition of renal dysfunction and appropriate dose adjustment particularly important in elderly patients with cardiovascular disease. This article reviews current approaches to the estimation of renal function, and unique considerations related to prescribing medication for elderly patients with concomitant renal and cardiovascular disease.
Key Points
-
Renal function declines with age in healthy individuals, but the risk of chronic kidney disease is raised in elderly patients with cardiovascular disease
-
Proven therapies for prevention and treatment of cardiovascular disease are often underused in older patients because of physicians' limited understanding of adverse and therapeutic effects
-
Estimates of glomerular filtration rate based on serum creatinine levels and a urine albumin-to-creatinine ratio should be calculated to screen for chronic kidney disease or reduced renal function
-
Cardiologists and nephrologists should collaborate closely to assess risks and ensure elderly patients receive the most appropriate therapies
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
US Census Bureau (online 18 March 2004) US interim projections by age, sex, race, and hispanic origin. [http://www.census.gov/ipc/www/usinterimproj/] (accessed 1 August 2005)
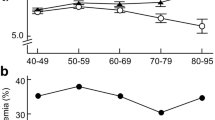
Rowe JW et al. (1976) The effect of age on creatinine clearance in men: a cross-sectional and longitudinal study. J Gerontol 31: 155–163
McCullough PA et al. (2000) Risks associated with renal dysfunction in patients in the coronary care unit. J Am Coll Cardiol 36: 679–684
Shlipak MG et al. (2002) Association of renal insufficiency with treatment and outcomes after myocardial infarction in elderly patients. Ann Intern Med 137: 555–562
Al Suwaidi J et al. (2002) Prognostic implications of abnormalities in renal function in patients with acute coronary syndromes. Circulation 106: 974–980
Wright RS et al. (2002) Acute myocardial infarction and renal dysfunction: a high risk combination. Ann Intern Med 137: 563–570
Shlipak MG et al. (2004) Renal function, digoxin therapy, and heart failure outcomes: evidence from the digoxin intervention group trial. J Am Soc Nephrol 15: 2195–2203
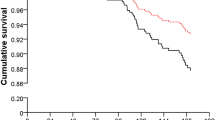
Go AS et al. (2004) Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351: 1296–1305
Weiner DE et al. (2004) Chronic kidney disease as a risk factor for cardiovascular disease and all-cause mortality: a pooled analysis of community-based studies. J Am Soc Nephrol 15: 1307–1315
Anavekar NS et al. (2004). Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med 351: 1285–1295
Tonelli M et al. (2001) Cardiac risk factors and the use of cardioprotective medications in patients with chronic renal insufficiency. Am J Kidney Dis 37: 484–489
McCullough PA et al. (2002) Benefits of aspirin and beta-blockade after myocardial infarction in patients with chronic kidney disease. Am Heart J 144: 226–232
Coresh J et al. (2003) Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis 41: 1–12
Coresh J et al. (2005) Chronic kidney disease awareness, prevalence, and trends among US adults, 1999 to 2000. J Am Soc Nephrol 16: 180–188
Corsonello A et al. (2005) Concealed renal insufficiency and adverse drug reactions in elderly hospitalized patients. Arch Intern Med 165: 790–795
National Kidney Foundation. Kidney disease outcomes quality initiative. Clinical practice guidelines [http://www.kidney.org/professionals/kdoqi/guidelines.cfm] (accessed 1 August 2005)
Cockcroft DW and Gault MH (1976) Prediction of creatinine clearance from serum creatinine. Nephron 16: 31–41
Levey AS et al. (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130: 461–470
Froissart M et al. (2005) Predictive performance of the MDRD and Cockcroft-Gault equations for estimating renal function. J Am Soc Nephrol 16: 763–773
Verhave JC et al. (2004) Drawbacks of the use of indirect estimates of renal function to evaluate the effect of risk factors on renal function. J Am Soc Nephrol 15: 1316–1322
Bostom AG et al. (2002) Predictive performance of renal function equations for patients with chronic kidney disease and normal serum creatinine levels. J Am Soc Nephrol 13: 2140–2144
Baracskay D et al. (1997) Geriatric renal function: estimating glomerular filtration in an ambulatory elderly population. Clin Nephrol 47: 222–228
Coresh J et al. (2002) Estimating the prevalence of low glomerular filtration rate requires attention to the creatinine assay calibration. J Am Soc Nephrol 13: 2811–2812
Coresh J et al. (2002) Calibration and random variation of the serum creatinine assay as critical elements of using equations to estimate the glomerular filtration rate. Am J Kidney Dis 39: 920–929
Fick DM et al. (2003) Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med 163: 2716–2724
Chobanian AV et al. (2003) Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 42: 1206–1252
The GISEN Group (Gruppo Italiano di Studi Epidemiologici in Nefrologia) (1997) Randomised placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy. Lancet 349: 857–1863
Brenner BM et al (2001) Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 345: 861–869
Lewis EJ et al. (2001) Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 345: 851–860
Shlipak MG (2003) Pharmacotherapy for heart failure in patients with renal insufficiency. Ann Intern Med 138: 917–924
Bakris GL and Weir M (2000) Angiotensin-converting enzyme inhibitor-associated elevations in serum creatinine: is this a cause for concern? Arch Intern Med 160: 685–693
Ljungman S et al. (1992) Renal function in severe congestive heart failure during treatment with enalapril (the Cooperative North Scandinavian Enalapril Survival Study [CONSENSUS] Trial). Am J Cardiol 70: 479–487
Tamirisa KP et al. (2004) Spironolactone-induced renal insufficiency and hyperkalemia in patients with heart failure. Am Heart J 148: 971–978
Dussol B et al. (2005) A randomized trial of furosemide vs hydrochlorothiazide in patients with chronic renal failure and hypertension. Nephrol Dial Transplant 20: 349–353
Oparil S et al. (1999) Fenoldopam: a new parenteral antihypertensive: consensus roundtable on the management of perioperative hypertension and hypertensive crises. Am J Hypertens 12: 653–664
Devlin JW et al. (2004) Fenoldopam versus nitroprusside for the treatment of hypertensive emergency. Ann Pharmacother 38: 755–759
Reddan D et al. (2003) Anticoagulation in acute cardiac care in patients with chronic kidney disease. Am Heart J 145: 586–594
Becker RC et al. (2002) Influence of patient characteristics and renal function on factor Xa inhibition, pharmacokinetics and pharmacodynamics after enoxaparin administration in non-ST-segment elevation acute coronary syndromes. Am Heart J 143: 753–759
Spinler SA et al. (2003) Safety and efficacy of unfractionated heparin versus enoxaparin in patients who are obese and patients with severe renal impairment: analysis from the ESSENCE and TIMI 11B studies. Am Heart J 146: 33–41
Kruse MW and Lee JJ (2004) Retrospective evaluation of a pharmacokinetic program for adjusting enoxaparin in renal impairment. Am Heart J 148: 582–589
Oster JR et al. (1995) Heparin-induced aldosterone suppression and hyperkalemia. Am J Med 98: 575–586
Smith NL (1999) Temporal trends in the use of anticoagulants among older adults with atrial fibrillation. Arch Intern Med 159: 1574–1578
Siguret V et al. (2005) Initiation of warfarin therapy in elderly medical inpatients: A safe and accurate regimen. Am J Med 118: 137–142
Ansell J et al. (2004) The pharmacology and management of the vitamin K antagonists: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest 126 (Suppl 3): 204S–233S
Buresly K et al. (2005) Bleeding complications associated with combinations of aspirin, thienopyridine derivatives, and warfarin in elderly patients following acute myocardial infarction. Arch Intern Med 165: 784–789
Baigent C et al. (2005) First United Kingdom Heart and Renal Protection (UK-HARP-1) study: biochemical efficacy and safety of simvastatin and safety of low dose aspirin in chronic kidney disease. Am J Kidney Dis 45: 473–484
Reddan DN et al. (2003) Treatment effects of eptifibatide in planned coronary stent implantation in patients with chronic kidney disease (ESPRIT Trial). Am J Cardiol 91: 17–21
Freeman RV et al. (2003) Influence of concurrent renal dysfunction on outcomes of patients with acute coronary syndromes and implications of the use of glycoprotein IIb/IIIa inhibitors. J Am Coll Cardiol 41: 718–724
Best PJ et al. (2003) Safety of abciximab in patients with chronic renal insufficiency who are undergoing percutaneous coronary interventions. Am Heart J 146: 213–214
Bianchi S et al. (2003) A controlled, prospective study of the effects of atorvastatin on proteinuria and progression of kidney disease. Am J Kidney Dis 41: 565–570
Tonelli M et al. (2003) Effect of pravastatin on loss of renal function in people with moderate chronic renal insufficiency and cardiovascular disease. J Am Soc Nephrol 14: 1605–1613
Sackner-Bernstein JD et al. (2005) Risk of worsening renal function with nesiritide in patients with acutely decompensated heart failure. Circulation 111: 1487–1491
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Wyatt, C., Kim, M. & Winston, J. Therapy Insight: how changes in renal function with increasing age affect cardiovascular drug prescribing. Nat Rev Cardiol 3, 102–109 (2006). https://doi.org/10.1038/ncpcardio0433
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpcardio0433
This article is cited by
-
Urologische Infektionen und Antibiotikamanagement bei geriatrischen Patienten
Der Urologe (2019)
-
Le rôle du médecin gériatre chez le patient âgé insuffisant rénal chronique
Les cahiers de l'année gérontologique (2009)
-
Besonderheiten der Pharmakotherapie beim älteren Hypertoniker
Der Internist (2009)
-
Renal dysfunction in heart failure patients: what is the evidence?
Heart Failure Reviews (2007)