Abstract
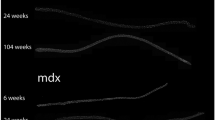
Duchenne muscular dystrophy (DMD), the most common inherited muscular dystrophy of childhood, leads to death due to cardiorespiratory failure. Paradoxically, mdx mice with the same genetic deficiency of dystrophin exhibit minimal cardiac dysfunction, impeding the development of therapies. We postulated that the difference between mdx and DMD might result from differences in telomere lengths in mice and humans. We show here that, like DMD patients, mice that lack dystrophin and have shortened telomeres (mdx/mTRKO) develop severe functional cardiac deficits including ventricular dilation, contractile and conductance dysfunction, and accelerated mortality. These cardiac defects are accompanied by telomere erosion, mitochondrial fragmentation and increased oxidative stress. Treatment with antioxidants significantly retards the onset of cardiac dysfunction and death of mdx/mTRKO mice. In corroboration, all four of the DMD patients analysed had 45% shorter telomeres in their cardiomyocytes relative to age- and sex-matched controls. We propose that the demands of contraction in the absence of dystrophin coupled with increased oxidative stress conspire to accelerate telomere erosion culminating in cardiac failure and death. These findings provide strong support for a link between telomere length and dystrophin deficiency in the etiology of dilated cardiomyopathy in DMD and suggest preventive interventions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Liew, C. C. & Dzau, V. J. Molecular genetics and genomics of heart failure. Nat. Rev. Genet. 5, 811–825 (2004).
Hoffman, E. P., Brown, R. H. Jr & Kunkel, L. M. Dystrophin: the protein product of the Duchenne muscular dystrophy locus. Cell 51, 919–928 (1987).
Petrof, B. J., Shrager, J. B., Stedman, H. H., Kelly, A. M. & Sweeney, H. L. Dystrophin protects the sarcolemma from stresses developed during muscle contraction. Proc. Natl Acad. Sci. USA 90, 3710–3714 (1993).
Bushby, K., Muntoni, F. & Bourke, J. P. 107th ENMC international workshop: the management of cardiac involvement in muscular dystrophy and myotonic dystrophy. 7th–9th June 2002, Naarden, the Netherlands. Neuromuscul. Disord. 13, 166–172 (2003).
Baxter, P. Treatment of the heart in Duchenne muscular dystrophy. Dev. Med. Child Neurol. 48, 163 (2006).
Duan, D. Challenges and opportunities in dystrophin-deficient cardiomyopathy gene therapy. Human Mol. Genet. 15 (Spec No 2), R253–R261 (2006).
McNally, E. M. New approaches in the therapy of cardiomyopathy in muscular dystrophy. Annu. Rev. Med. 58, 75–88 (2007).
Cohn, J. N. Heart failure: future treatment approaches. Am. J. Hypertens. 13, 74S–78S (2000).
Cohn, R. D. et al. Angiotensin II type 1 receptor blockade attenuates TGF- β-induced failure of muscle regeneration in multiple myopathic states. Nat. Med. 13, 204–210 (2007).
Bulfield, G., Siller, W. G., Wight, P. A. & Moore, K. J. X chromosome-linkedmuscular dystrophy (mdx) in the mouse. Proc. Natl Acad. Sci. USA 81, 1189–1192 (1984).
Bridges, L. R. The association of cardiac muscle necrosis and inflammation with the degenerative and persistent myopathy of MDX mice. J. Neurol. Sci. 72, 147–157 (1986).
Torres, L. F. & Duchen, L. W. The mutant mdx : inherited myopathy in the mouse. Morphological studies of nerves, muscles and end-plates. Brain 110 (pt 2), 269–299 (1987).
Greider, C. W. & Blackburn, E. H. The telomere terminal transferase of Tetrahymena is a ribonucleoprotein enzyme with two kinds of primer specificity. Cell 51, 887–898 (1987).
Kipling, D. & Cooke, H. J. Hypervariable ultra-long telomeres in mice. Nature 347, 400–402 (1990).
Hemann, M. T. & Greider, C. W. Wild-derived inbred mouse strains have short telomeres. Nucleic Acids Res. 28, 4474–4478 (2000).
Lee, H. W. et al. Essential role of mouse telomerase in highly proliferative organs. Nature 392, 569–574 (1998).
Sacco, A. et al. Short telomeres and stem cell exhaustion model Duchenne muscular dystrophy in mdx/mTR mice. Cell 143, 1059–1071 (2010).
Bergmann, O. et al. Evidence for cardiomyocyte renewal in humans. Science 324, 98–102 (2009).
Blasco, M. A. et al. Telomere shortening and tumor formation by mouse cells lacking telomerase RNA. Cell 91, 25–34 (1997).
Im, W. B. et al. Differential expression of dystrophin isoforms in strains of mdx mice with different mutations. Human Mol. Genet. 5, 1149–1153 (1996).
Emery, A. E. Population frequencies of inherited neuromuscular diseases—A world survey. Neuromuscul. Disord. 1, 19–29 (1991).
Finsterer, J. & Stollberger, C. The heart in human dystrophinopathies. Cardiology 99, 1–19 (2003).
Sanyal, S. K. & Johnson, W. W. Cardiac conduction abnormalities in children with Duchenne’s progressive muscular dystrophy: electrocardiographic features and morphologic correlates. Circulation 66, 853–863 (1982).
Schneider, J. E. et al. Fast, high-resolution in vivo cine magnetic resonance imaging in normal and failing mouse hearts on a vertical 11.7 T system. J. Magn. Reson. Imaging 18, 691–701 (2003).
Flores, I. et al. The longest telomeres: a general signature of adult stem cell compartments. Genes Dev. 22, 654–667 (2008).
Gonzalez-Suarez, E., Samper, E., Flores, J. M. & Blasco, M. A. Telomerase-deficient mice with short telomeres are resistant to skin tumorigenesis. Nat. Genet. 26, 114–117 (2000).
Meeker, A. K. & De Marzo, A. M. Recent advances in telomere biology: implications for human cancer. Curr. Opin. Oncol. 16, 32–38 (2004).
Meeker, A. K. et al. Telomere length assessment in human archival tissues: combined telomere fluorescence in situ hybridization and immunostaining. Am. J. Pathol. 160, 1259–1268 (2002).
Meeker, A. K. et al. Telomere shortening occurs in subsets of normal breast epithelium as well as in situ and invasive carcinoma. Am. J. Pathol. 164, 925–935 (2004).
Sahin, E. et al. Telomere dysfunction induces metabolic and mitochondrial compromise. Nature 470, 359–365 (2011).
Brown, D. A. & O’Rourke, B. Cardiac mitochondria and arrhythmias. Cardiovasc. Res. 88, 241–249 (2010).
Iglewski, M., Hill, J. A., Lavandero, S. & Rothermel, B. A. Mitochondrial fission and autophagy in the normal and diseased heart. Curr. Hypertens. Rep. 12, 418–425 (2010).
Murdoch, C. E., Zhang, M., Cave, A. C. & Shah, A. M. NADPH oxidase-dependent redox signalling in cardiac hypertrophy, remodelling and failure. Cardiovasc. Res. 71, 208–215 (2006).
Takimoto, E. et al. Oxidant stress from nitric oxide synthase-3 uncoupling stimulates cardiac pathologic remodeling from chronic pressure load. J. Clin. Invest. 115, 1221–1231 (2005).
Van Empel, V. P. et al. Downregulation of apoptosis-inducing factor inharlequin mutant mice sensitizes the myocardium to oxidative stress-related cell death and pressure overload-induced decompensation. Circ. Res. 96, e92–e101 (2005).
Sawyer, D. B. Oxidative stress in heart failure: what are we missing? Am. J. Med. Sci. 342, 120–124 (2011).
Rasmussen, H. H., Hamilton, E. J., Liu, C. C. & Figtree, G. A. Reversible oxidative modification: implications for cardiovascular physiology and pathophysiology. Trends Cardiovasc. Med. 20, 85–90 (2010).
Kratsios, P. et al. Antioxidant amelioration of dilated cardiomyopathy caused by conditional deletion of NEMO/IKK γ in cardiomyocytes. Circ. Res. 106, 133–144 (2010).
Shigenaga, M. K., Gimeno, C. J. & Ames, B. N. Urinary 8-hydroxy-2’-deoxyguanosine as a biological marker of in vivo oxidative DNA damage. Proc. Natl Acad. Sci. USA 86, 9697–9701 (1989).
Shirendeb, U. et al. Abnormal mitochondrial dynamics, mitochondrial loss and mutant huntingtin oligomers in Huntington’s disease: implications for selective neuronal damage. Human Mol. Genet. 20, 1438–1455 (2011).
Li, Y. et al. Cytosolic, but not mitochondrial, oxidative stress is a likely contributor to cardiac hypertrophy resulting from cardiac specific GLUT4 deletion in mice. FEBS J. (2011).
Sanyal, S. K., Johnson, W. W., Thapar, M. K. & Pitner, S. E. An ultrastructural basis for electrocardiographic alterations associated with Duchenne’s progressive muscular dystrophy. Circulation 57, 1122–1129 (1978).
Finder, J. D. et al. Respiratory care of the patient with Duchenne muscular dystrophy: ATS consensus statement. Am. J. Respir. Crit. Care Med. 170, 456–465 (2004).
Deconinck, A. E. et al. Utrophin-dystrophin-deficient mice as a model for Duchenne muscular dystrophy. Cell 90, 717–727 (1997).
Megeney, L. A. et al. Severe cardiomyopathy in mice lacking dystrophin and MyoD. Proc. Natl Acad. Sci. USA 96, 220–225 (1999).
Rooney, J. E. et al. Severe muscular dystrophy in mice that lack dystrophin and α7 integrin. J. Cell Sci. 119, 2185–2195 (2006).
Grady, R. M. et al. Role for α-dystrobrevin in the pathogenesis of dystrophin-dependent muscular dystrophies. Nat. Cell Biol. 1, 215–220 (1999).
Chandrasekharan, K. et al. A human-specific deletion in mouse Cmah increases disease severity in the mdx model of Duchenne muscular dystrophy. Sci. Transl. Med. 2, 42ra54 (2010).
Qi, L. et al. Short telomeres and ataxia-telangiectasia mutated deficiency cooperatively increase telomere dysfunction and suppress tumorigenesis. Cancer Res. 63, 8188–8196 (2003).
Wong, K. K. et al. Telomere dysfunction and Atm deficiency compromises organ homeostasis and accelerates ageing. Nature 421, 643–648 (2003).
Chamberlain, J. S. Duchenne muscular dystrophy models show their age. Cell 143, 1040–1042 (2010).
Frankel, K. A. & Rosser, R. J. The pathology of the heart in progressive muscular dystrophy: epimyocardial fibrosis. Hum. Pathol. 7, 375–386 (1976).
Esposito, L. A., Melov, S., Panov, A., Cottrell, B. A. & Wallace, D. C. Mitochondrial disease in mouse results in increased oxidative stress. Proc. Natl Acad. Sci. USA 96, 4820–4825 (1999).
Narula, N. et al. Adenine nucleotide translocase 1 deficiency results in dilated cardiomyopathy with defects in myocardial mechanics, histopathological alterations, and activation of apoptosis. JACC Cardiovasc. Imaging 4, 1–10 (2011).
Brouilette, S., Singh, R. K., Thompson, J. R., Goodall, A. H. & Samani, N. J. White cell telomere length and risk of premature myocardial infarction. Arterioscler. Thromb. Vasc. Biol. 23, 842–846 (2003).
Urashima, T. et al. Molecular and physiological characterization of RV remodeling in a murine model of pulmonary stenosis. Am. J. Physiol. Heart Circ. Physiol. 295, H1351–H1368 (2008).
McCalmon, S. A. et al. Modulation of angiotensin II-mediated cardiac remodeling by the MEF2A target gene Xirp2. Circ. Res. 106, 952–960 (2010).
Yin, F. C. P., Spurgeon, H. A., Rakusan, K., Myron, L. & Lakatta, W. E. G. Use of tibial length to quantify cardiac hypertrophy: application in the aging rat. Am. J. Physiol. Heart Circ. Physiol. 243, H941–H947 (1982).
Acknowledgements
We thank E. Ashley (Director, Stanford Center for Inherited Cardiovascular Disease), J. Cooke (Associate Director of Cardiovascular Institute, Stanford), M. V. McConnell (Cardiovascular Medicine, Stanford), A. Connolly (Pathology, Stanford), S. Artandi (Medicine-Hematology, Stanford) and J. Pomerantz (Center of Regeneration Medicine and Stem Cell Research, UCSF) for insightful discussions and critical comments. We greatly appreciate the input and thoughtful discussions from all Blau laboratory members and would like to especially thank S. Sampath for critical comments on the manuscript and A.T. Van Ho for help with the final formatting of the Supplementary Videos. We are grateful to D. Regula (Department of Pathology, Stanford) for providing the control cardiac samples, and M. Halushka (Department of Pathology, Johns Hopkins), A. H. Beggs (Harvard University) and H. Lidov (Department of Pathology, Boston Children’s Hospital) for providing us with DMD cardiac samples. Moreover, we are grateful to Muscular Dystrophy Center Core Laboratories at University of Minnesota, the Department of Pathology at Boston Children’s Hospital, and the DMD patients and their families who contribute to the tissue repository. We thank: E. Neri (Data Manager, Stanford) for computational algorithms for analysis of telomere lengths, A. Olson at the NMS (Stanford Neuroscience Microscopy Service, supported by NIH NS069375), K. Koleckar (Blau laboratory), and P. Chu (Comparative Medicine, Stanford), L. J. Pisani (MIPS MRI Physicist, Stanford Small Imaging Facility), J. Perrino (Electron Microscopy Facility, Stanford) as well as R. Zasio and E. Florendo (Stanford Mouse Facility) for excellent technical assistance. This work was supported by: the American Heart Association Scientist Development Grant 10SDG3510024 (F.M.); NIH/NIAMS P30 grants AR057220 (J.W.D.) and R01CA84628 (R.A.D.); NIH grants HL061535 (D.B.), P50CA058236 (W. Nelson) and NIHSPORE in ProstateCancer (A.K.M.); grants from the Robert A. and Renee E. Belfer Foundation (R.A.D., A.M. and A.P.); NIH grants HL096113, HL100397, AG020961 and AG009521 (H.M.B.); MDA grant 4320 (H.M.B.); and the Baxter Foundation (H.M.B.).
Author information
Authors and Affiliations
Contributions
F.M. designed the studies and performed the experiments, J.K. performed mouse work, histology, immunohistochemistry, mitochondrial quantification analysis and design of schematic diagrams, P.K. maintained the mouse colony and performed histological sections, F.M., A.K.M., M.K-A. and R.A.D. aided with telomere analyses in mouse samples, F.M. and A.K.M. performed the telomere analysis in human samples, F.M. and D.B. performed the ECG analyses, F.M. and M-M.Z. performed the osmotic minipump experiments, J.W.D. provided human cardiac samples, and F.M. and H.M.B. designed the experiments, discussed and interpreted the results, and wrote the paper with input from A.K.M., R.A.D. and D.B.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
Supplementary Figure 1 Development of minimal hypertrophy in G2 mice and size of G2 cardiac muscle cells.
(a) Breeding scheme describing the generation of mdx/mTR mice. Each C57BL6 mdx4cv (dystrophin mutations located on exon 53) or mTRHet (lacking the RNA component of telomerase), mouse is the result of isogenic breeding with C57BL6 wildtype (WT) mice from Jackson Laboratories to eliminate spontaneous mutations in the subsequent crosses. The resulting heterozygous mice (mdx/mTRHet designated as Het) were further intercrossed (intercousin matings only to preserve genetically uniform mice) to generate the first generation of double-mutant mdx mice totally lacking dystrophin and telomerase activity (mdx/mTRG1 designated as G1). G1 mice were intercrossed (cousin matings only) to produce second-generation double mutant mice (mdx/mTRG2 designated as G2). (b) Cardiac tissues were weighed from mice at 32 weeks of age. Data are represented as the weight of the tissue divided by the weight of the whole mouse, a standard control for telomere shortening16. Left graph shows comparison of heart to whole body weight (HW/BW) and right graph shows comparison of heart weight to tibial length (HW/TL), standard measurements of progressive development of cardiac dilation58. Data are represented as mean ± s.e.m. (n = 3–5). Two-tailed, unpaired Student’s t-test, P values are indicated. (c) Highly proliferative organs with substantial cell turnover, such as testis, liver, spleen and lung do not display significant differences in weight at G2. Data are represented as mean ± s.e.m. (n = 3–5); Two-tailed, unpaired Student’s t-test, P>0.2 (n.s.). (d) Representative image of nuclei (blue, DAPI, left panel) and cardiac myofibres (green, cTnT, right panel). These sections were used for the nuclei measurements. A total of 3 hearts per genotype were analyzed. (e) Histogram reveals a small decrease in the size of cardiac nuclei of G2 mice compared to controls. Number of measured nuclei: mdx/mTRHet (Het) (N = 102), mdx/mTRG2 (G2) (N = 134) and mdx/mTRG2 (N = 97). (f) Morphometric analysis (frequency distribution of the diameter of cardiac fibres) show that G2 fibres are thinner that controls. Number of fibres scored: mdx/mTRHet (Het) (N = 88), mdx/mTRG2 (G2) (N = 98) and mTRG2 (N = 96). Source data are shown in Supplementary Table S1.
Supplementary Figure 2 Echocardiography measurements show similar measurements in young G2 animals, but significant differences in old G1 and young G3 animals.
(a–b) No major differences in fractional shortening (%FS), Left Ventricular Transverse Area in diastole (LVTAd) and systole (LVTAs). (n = 4–9) of (a) 12- (b) and 20-weeks-old mice. Two-tailed, unpaired Student’s t-test, P>0.1 (n.s.). (c) Cardiac dysfunction is evident in 80-weeks-old G1 animals (grey bars) and young 8-weeks-old G3 mice (white bars) compared to 32-weeks-old (black bars) animals. Data are represented as mean ± s.e.m. (n = 5–8); Two-tailed, unpaired Student’s t-test, * indicates P<0.05, ** P<0.02 and ***P<0.001. Source data are shown in Supplementary Table S1.
Supplementary Figure 3 Angiotensin II induced stress induces premature heart failure in young G2 mice.
(a) Scheme of experimental procedure. Mice were tested for cardiac function by echocardiography prior to minipump insertion. Osmotic minipumps delivering either saline (S) or Angiotensin II (A) were implanted subcutaneously into 12-week-old asymptomatic G2 and control mice and cardiac function was measured weekly. (b) Representative images 3 weeks after minipump insertion show left ventricular dilation and compromised contractility only in G2 hearts that received Angiotensin II (See also Supplementary Videos S2.). (c) Echocardiographic measurements over time show reduction in fractional shortening (FS), increase in left ventricular transverse area in diastole (LVTAd) and increase in left ventricular transverse area in systole (LVTAs), only in hearts of G2 animals with Angiotensin II, compared to the control mice. Data are represented as mean±SEM (n = 5–6); ANOVA followed by Bonferonni test for multiple comparisons, ** indicates P<0.01 and ***P<0.001. (d) Representative histological analysis using Trichrome staining on longitudinal paraffin sections show increased fibrotic tissue deposition in hearts of Angiotensin II treated G2 mice compared to controls. (e) Quantification of fibrosis. Data are represented as mean±SEM (n = 4); Two-tailed, unpaired Student’s t-test, P value is indicated. Source data are shown in Supplementary Table S1.
Supplementary Figure 4 Telomere Q-FISH analysis of mouse and human DMD hearts.
(a) Representative Telomere Q-FISH images (red telomeric probe; blue DAPI-stained nuclei, and green immunofluorescence of cardiac Troponin T reveals striated cardiomyocytes). White arrows indicate nuclei within cardiomyocytes. DAPI staining was used to define nuclear area and Cy3 staining was used to quantify telomere fluorescence. Each Cy3 image was an overlay of the DAPI image. The nuclei within cardiomyocytes (as defined by cardiac Troponin T) were selected in the DAPI images and the Telometer program automatically calculated the pixels (Cy3+ telomeres) on the selected nuclei. (b) Representative Telomere Q-FISH images (red telomeric probe, blue DAPI-stained nuclei, and green immunofluorescence of α-smooth muscle cells reveals cardiac vessels). (c) Quantification of telomere shortening in α-smooth muscle mouse cells represents the intensity sum of all telomere pixels (Cy3+ telomeres) divided by the intensity sum of all nuclear DNA pixels of the entire nucleus (DAPI). n = 3 hearts per genotype analyzed. The number of nuclei scored: WT (N = 290), Het (N = 140), G1 (N = 195), G2 (N = 186), mTRG2 (N = 282). Data are represented as mean±SEM; Two-tailed, unpaired Student’s t-test, P>0.7 (n.s.), (d) Representative Telomere Q-FISH mouse testis images (red, telomeric probe, blue DAPI-stained nuclei). (e) Quantification of the telomere shortening in the mouse testes’ spermatocytes of all different genotypes. n = 3 testes per genotype analyzed. The number of nuclei scored: WT (N = 359), Het (N = 320), G1 (N = 300), G2 (N = 221), mTRG2 (N = 219). Data are represented as mean±SEM. Two-tailed, unpaired Student’s t-test, P>0.3 (n.s.). (f) Representative human Telomere Q-FISH images (red, telomeric probe; blue, DAPI-stained nuclei and green, cardiac Troponin T staining). (g) Representative human Telomere Q-FISH images (red telomeric probe, blue DAPI-stained nuclei, and green immunofluorescence of α-smooth muscle cells reveals cardiac vessels). (h) Quantification of telomere shortening in α-smooth muscle cells in human hearts represents the intensity sum of all telomere pixels (Cy3+ telomeres) divided by the intensity sum of all nuclear DNA pixels of the entire nucleus (DAPI). A total of 3 control and 3 DMD cardiac samples were analyze and the number of nuclei scored: Control 1 (N = 43), Control 2 (N = 35), Control 3 (N = 52), DMD 2 (N = 76), DMD 3 (N = 41) and DMD 4 (N = 58). Two-tailed, unpaired Student’s t-test, P>0.06 (n.s.). Source data are shown in Supplementary Table S1.
Supplementary Figure 5 Cardiomyocyte proliferation and death in G2 hearts.
(a) Representative image (red Ki67; blue DAPI-stained nuclei, and green immunofluorescence of cardiac Troponin T reveals striated cardiomyocytes) used to assess cardiac proliferation measurements. (b) No major differences on cardiomyocytes proliferation are detected by Ki67 (left graph) and phospho-Histone-3 (right graph) analysis. A total of 8–10 hearts per genotype were analyzed. Two-tailed, unpaired Student’s t-test, P>0.08 (n.s.). (c) Representative image (green TUNEL; blue DAPI-stained nuclei, and red immunofluorescence of cardiac Troponin T reveals striated cardiomyocytes) used to assess cardiac apoptosis measurements. (d) Increase on cardiomyocytes apoptosis is detected by TUNEL (left graph) and cleaved caspase-3 (right graph) analysis. Data are represented as mean ± s.e.m. (n = 3); Two-tailed, unpaired Student’s t-test, P values are indicated. Source data are shown in Supplementary Table S1.
Supplementary Figure 6 Decreased cardiac fibrosis and dysfunction in anti-oxidant treated G2 animals.
(a) Representative Trichrome staining of cardiac sections of G2-saline (left) and G2-MnTBAP injected hearts. The fibrosis of hearts from G2-MnTBAP injected mice is still present but significant reduced compared to controls. (b) Quantification of fibrosis. (n = 5 mice per condition). Two-tailed, unpaired Student’s t-test, P>0.07 (n.s.). (c) Comparison of heart to whole body weight (HW/BW) at 32 weeks. Data are represented as mean±SEM (n = 6–7); Two-tailed, unpaired Student’s t-test, * indicates P<0.05. (d) Representative images from G2-saline and G2-MnTBAP hearts showing restoration of left ventricular dilation and contractility. Source data are shown in Supplementary Table S1.
Supplementary information
Supplementary Information
Supplementary Information (PDF 1771 kb)
Supplementary Table 1
Supplementary Information (XLS 144 kb)
Echocardiographic analysis indicates defect in G2 hearts.
Representative movies from 32-week-old animals show increased LV size and impairment in ventricular function in G2 hearts. (AVI 3095 kb)
Cardiac defect in G2 mice that received Angiotensin II.
Representative movies 3 weeks after the mini-osmotic pump experiment from 12-week-old mdx/mTRHet (Het) and G2 hearts received either saline or Ang II. Note that the G2 hearts with Ang II show left ventricular dilation, thin myocardial wall and compromised contraction. (AVI 3153 kb)
Rights and permissions
About this article
Cite this article
Mourkioti, F., Kustan, J., Kraft, P. et al. Role of telomere dysfunction in cardiac failure in Duchenne muscular dystrophy. Nat Cell Biol 15, 895–904 (2013). https://doi.org/10.1038/ncb2790
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ncb2790
This article is cited by
-
Folic acid alleviated oxidative stress-induced telomere attrition and inhibited apoptosis of neurocytes in old rats
European Journal of Nutrition (2024)
-
Tamoxifen treatment ameliorates contractile dysfunction of Duchenne muscular dystrophy stem cell-derived cardiomyocytes on bioengineered substrates
npj Regenerative Medicine (2022)
-
The multifaceted view of heart problem in Duchenne muscular dystrophy
Cellular and Molecular Life Sciences (2021)
-
Association between leucocyte telomere length and cardiovascular disease in a large general population in the United States
Scientific Reports (2020)
-
The protective function of non-coding DNA in DNA damage accumulation with age and its roles in age-related diseases
Biogerontology (2019)