Abstract
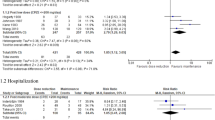
Few controlled trials compared second-generation antipsychotics (SGAs) with first-generation antipsychotics (FGAs) regarding relapse prevention in schizophrenia. We conducted a systematic review/meta-analysis of randomized trials, lasting ⩾6 months comparing SGAs with FGAs in schizophrenia. Primary outcome was study-defined relapse; secondary outcomes included relapse at 3, 6 and 12 months; treatment failure; hospitalization; and dropout owing to any cause, non-adherence and intolerability. Pooled relative risk (RR) (±95% confidence intervals (CIs)) was calculated using random-effects model, with numbers-needed-to-treat (NNT) calculations where appropriate. Across 23 studies (n=4504, mean duration=61.9±22.4 weeks), none of the individual SGAs outperformed FGAs (mainly haloperidol) regarding study-defined relapse, except for isolated, single trial-based superiority, and except for risperidone's superiority at 3 and 6 months when requiring ≥3 trials. Grouped together, however, SGAs prevented relapse more than FGAs (29.0 versus 37.5%, RR=0.80, CI: 0.70–0.91, P=0.0007, I2=37%; NNT=17, CI: 10–50, P=0.003). SGAs were also superior regarding relapse at 3, 6 and 12 months (P=0.04, P<0.0001, P=0.0001), treatment failure (P=0.003) and hospitalization (P=0.004). SGAs showed trend-level superiority for dropout owing to intolerability (P=0.05). Superiority of SGAs regarding relapse was modest (NNT=17), but confirmed in double-blind trials, first- and multi-episode patients, using preferentially or exclusively raw or estimated relapse rates, and for different haloperidol equivalent comparator doses. There was no significant heterogeneity or publication bias. The relevance of the somewhat greater efficacy of SGAs over FGAs on several key outcomes depends on whether SGAs form a meaningful group and whether mid- or low-potency FGAs differ from haloperidol. Regardless, treatment selection needs to be individualized considering patient- and medication-related factors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Lieberman JA . Atypical antipsychotic drugs as a first-line treatment of schizophrenia: a rationale and hypothesis. J Clin Psychiatry 1996; 57 (Suppl 11): 68–71.
Alexander GC, Gallagher SA, Mascola A, Moloney RM, Stafford RS . Increasing off-label use of antipsychotic medications in the United States, 1995–2008. Pharmacoepidemiol Drug Safety 2011; 20: 177–184.
Rummel-Kluge C, Komossa K, Schwarz S, Hunger H, Schmid F, Kissling W et al. Second-generation antipsychotic drugs and extrapyramidal side effects: A systematic review and meta-analysis of head-to-head comparisons. Schizophr Bull. Advance online publication, 31 May 2010 (e-pub ahead of print).
Correll CU, Leucht S, Kane JM . Lower risk for tardive dyskinesia associated with second-generation antipsychotics: a systematic review of 1-year studies. Am J Psychiatry 2004; 161: 414–425.
American Diabetes Association; American Psychiatric Association; American Association of Clinical Endocrinologists; North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. J Clin Psychiatry 2004; 65: 267–272.
Correll CU, Manu P, Olshanskiy V, Napolitano B, Kane JM, Malhotra AK . Cardiometabolic risk of second-generation antipsychotic medications during first-time use in children and adolescents. JAMA 2009; 302: 1765–1773.
Rosenheck R, Perlick D, Bingham S, Liu-Mares W, Collins J, Warren S et al. Effectiveness and cost of olanzapine and haloperidol in the treatment of schizophrenia: a randomized controlled trial. JAMA 2003; 290: 2693–2702.
Lieberman JA, Stroup TS, Mcevoy JP, Swartz MS, Rosenheck RA, Perkins DO et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005; 353: 1209–1223.
Jones PB, Barnes TR, Davies L, Dunn G, Lloyd H, Hayhurst KP et al. Randomized controlled trial of the effect on quality of life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry 2006; 63: 1079–1087.
Kahn RS, Fleischhacker WW, Boter H, Davidson M, Vergouwe Y, Keet IP et al. Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial. Lancet 2008; 371: 1085–1097.
Leucht S, Barnes TR, Kissling W, Engel RR, Correll C, Kane JM . Relapse prevention in schizophrenia with new-generation antipsychotics: a systematic review and exploratory meta-analysis of randomized, controlled trials. Am J Psychiatry 2003; 160: 1209–1222.
Tran PV, Dellva MA, Tollefson GD, Wentley AL, Beasley Jr CM . Oral olanzapine versus oral haloperidol in the maintenance treatment of schizophrenia and related psychoses. Br J Psychiatry 1998; 172: 499–505.
DerSimonian R, Laird N . Meta-analysis in clinical trials. Control Clin Trials 1986; 7: 177–188.
Higgins JP, Thompson SG, Deeks JJ, Altman DG . Measuring inconsistency in meta-analyses. BMJ 2003; 327: 557–560.
Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO et al. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry 2004; 161 (2 Suppl): 1–56.
Egger M, Davey SG, Schneider M, Minder C . Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315: 629–634.
Tamminga CA, Thaker GK, Moran M, Kakigi T, Gao XM . Clozapine in tardive dyskinesia: observations from human and animal model studies. J Clin Psychiatry 1994; 55 (Suppl B): 102–106.
Essock SM, Hargreaves WA, Covell NH, Goethe J . Clozapine's effectiveness for patients in state hospitals: results from a randomized trial. Psychopharmacol Bull 1996; 32: 683–697.
Speller JC, Barnes TR, Curson DA, Pantelis C, Alberts JL . One-year, low-dose neuroleptic study of in-patients with chronic schizophrenia characterised by persistent negative symptoms. Amisulpride v. haloperidol. Br J Psychiatry 1997; 171: 564–568.
Daniel DG, Wozniak P, Mack RJ, McCarthy BG . Long-term efficacy and safety comparison of sertindole and haloperidol in the treatment of schizophrenia. The Sertindole Study Group. Psychopharmacol Bull 1998; 34: 61–69.
Rosenheck R, Evans D, Herz L, Cramer J, Xu W, Thomas J et al. How long to wait for a response to clozapine: a comparison of time course of response to clozapine and conventional antipsychotic medication in refractory schizophrenia. Schizophr Bull 1999; 25: 709–719.
Colonna L, Saleem P, Dondey-Nouvel L, Rein W . Long-term safety and efficacy of amisulpride in subchronic or chronic schizophrenia. Amisulpride Study Group. Int Clin Psychopharmacol 2000; 15: 13–22.
Csernansky JG, Mahmoud R, Brenner R . A comparison of risperidone and haloperidol for the prevention of relapse in patients with schizophrenia. N Engl J Med 2002; 346: 16–22.
de Sena EP, Santos-Jesus R, Miranda-Scippa A, Quarantini LC, Oliveira IR . Relapse in patients with schizophrenia: a comparison between risperidone and haloperidol. Rev Bras Psiquiatr 2003; 25: 220–223.
Kasper S, Lerman MN, McQuade RD, Saha A, Carson WH, Ali M et al. Efficacy and safety of aripiprazole vs haloperidol for long-term maintenance treatment following acute relapse of schizophrenia. Int J Neuropsychopharmacol 2003; 6: 325–337.
Lieberman JA, Phillips M, Gu H, Stroup S, Zhang P, Kong L et al. Atypical and conventional antipsychotic drugs in treatment-naive first-episode schizophrenia: a 52-week randomized trial of clozapine vs chlorpromazine. Neuropsychopharmacology 2003; 28: 995–1003.
Marder SR, Glynn SM, Wirshing WC, Wirshing DA, Ross D, Widmark C et al. Maintenance treatment of schizophrenia with risperidone or haloperidol: 2-year outcomes. Am J Psychiatry 2003; 160: 1405–1412.
Schooler N, Rabinowitz J, Davidson M, Emsley R, Harvey PD, Kopala L et al. Risperidone and haloperidol in first-episode psychosis: a long-term randomized trial. Am J Psychiatry 2005; 162: 947–953.
Lieberman JA, Tollefson G, Tohen M, Green AI, Gur RE, Kahn R et al. Comparative efficacy and safety of atypical and conventional antipsychotic drugs in first-episode psychosis: a randomized, double-blind trial of olanzapine versus haloperidol. Am J Psychiatry 2003; 160: 1396–1404.
Green AI, Lieberman JA, Hamer RM, Glick ID, Gur RE, Kahn RS et al. Olanzapine and haloperidol in first episode psychosis: two-year data. Schizophr Res 2006; 86: 234–243.
Gaebel W, Riesbeck M, Wolwer W, Klimke A, Eickhoff M, von Wilmsdorff M et al. Maintenance treatment with risperidone or low-dose haloperidol in first-episode schizophrenia: 1-year results of a randomized controlled trial within the German Research Network on Schizophrenia. J Clin Psychiatry 2007; 68: 1763–1774.
Kane JM, Lauriello J, Laska E, Di Marino M, Wolfgang CD . Long-term efficacy and safety of iloperidone: results from 3 clinical trials for the treatment of schizophrenia. J Clin Psychopharmacol 2008; 28 (2 Suppl 1): S29–S35.
Crespo-Facorro B, Perez-Iglesias R, Mata I, Caseiro O, Martinez-Garcia O, Pardo G et al. Relapse prevention and remission attainment in first-episode non-affective psychosis. A randomized, controlled 1-year follow-up comparison of haloperidol, risperidone and olanzapine. J Psychiatr Res 2010; 45: 763–769.
Gitlin M, Nuechterlein K, Subotnik KL, Ventura J, Mintz J, Fogelson DL et al. Clinical outcome following neuroleptic discontinuation in patients with remitted recent-onset schizophrenia. Am J Psychiatry 2001; 158: 1835–1842.
Rosenheck RA, Leslie DL, Sindelar J, Miller EA, Lin H, Stroup TS et al. Cost-effectiveness of second-generation antipsychotics and perphenazine in a randomized trial of treatment for chronic schizophrenia. Am J Psychiatry 2006; 163: 2080–2089.
Rosenheck RA, Leslie DL, Doshi JA . Second-generation antipsychotics: cost-effectiveness, policy options, and political decision making. Psychiatr Serv 2008; 59: 515–520.
Rosenheck RA . Pharmacotherapy of first-episode schizophrenia. Lancet 2008; 371: 1048–1049.
Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM . Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet 2009; 373: 31–41.
Kane JM, Correll CU . Past and present progress in the pharmacologic treatment of schizophrenia. J Clin Psychiatry 2010; 71: 1115–1124.
Leucht S, Heres S, Kissling W, Davis JM . Evidence-based pharmacotherapy of schizophrenia. Int J Neuropsychopharmacol 2011; 14: 269–284.
Dolder CR, Lacro JP, Dunn LB, Jeste DV . Antipsychotic medication adherence: is there a difference between typical and atypical agents? Am J Psychiatry 2002; 159: 103–108.
Velligan DI, Weiden PJ, Sajatovic M, Scott J, Carpenter D, Ross R et al. The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. J Clin Psychiatry 2009; 70 (Suppl 4): 1–46.
Leucht C, Heres S, Kane JM, Kissling W, Davis JM, Leucht S . Oral versus depot antipsychotic drugs for schizophrenia—a critical systematic review and meta-analysis of randomised long-term trials. Schizophr Res 2011; 127: 83–92.
Lambert M, Schimmelmann BG, Schacht A, Suarez D, Haro JM, Novick D et al. Differential 3-year effects of first- versus second-generation antipsychotics on subjective well-being in schizophrenia using marginal structural models. J Clin Psychopharmacol 2011; 31: 226–230.
Rosenheck RA . Evaluating the cost-effectiveness of reduced tardive dyskinesia with second-generation antipsychotics. Br J Psychiatry 2007; 191: 238–245.
Nielsen J, Skadhede S, Correll CU . Antipsychotics associated with the development of type 2 diabetes in antipsychotic-naive schizophrenia patients. Neuropsychopharmacology 2010; 35: 1997–2004.
Rummel-Kluge C, Komossa K, Schwarz S, Hunger H, Schmid F, Lobos CA et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res 2010; 123: 225–233.
Correll CU, Lencz T, Malhotra AK . Antipsychotic drugs and obesity. Trends Mol Med 2011; 17: 97–107.
De Hert M, Detraux J, van Winkel R, Yu W, Correll CU . Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol; Advance online publication, 18 October 2011; doi:10.1038/nrendo.2011.156 (e-pub ahead of print).
Leucht S, Wahlbeck K, Hamann J, Kissling W . New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis. Lancet 2003; 361: 1581–1589.
Acknowledgements
This work was supported in part by The Zucker Hillside Hospital Advanced Center for Intervention and Services Research for the Study of Schizophrenia (MH090590) from the National Institute of Mental Health, Bethesda, MD, USA. The sponsor had no influence on the design, data acquisition, data analysis, data interpretation or writing of the report. We thank Gennady Gelman, MD, and Allyssa Brody, BS, for help with the literature search and data abstraction. We thank the following authors and pharmaceutical companies for providing additional, unpublished data on their studies relevant for this meta-analysis: Drs Benedicto Crespo-Facorro, Eduardo Pondé de Sena, Jeffrey A Lieberman, Robert Hamer, Eli Lilly (Drs Bruce Kinon and Virginia Stauffer), Janssen-Cilag Brazil (Dr de Sena) and Novartis Pharmaceuticals Corporation (Dr Marla Hochfeld).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Kishimoto has received speaker's honoraria from Banyu, Eli Lilly, Dainippon Sumitomo, Janssen, Otsuka and Pfizer. He has received grant support from the Byoutaitaisyakenkyukai Fellowship (Fellowship of Astellas Foundation of Research on Metabolic Disorders) and Eli Lilly Fellowship for Clinical Psychopharmacology. Dr Agarwal has nothing to disclose. Dr Kishi has received speaker's honoraria from Astellas, Dainippon Sumitomo, Eli Lilly, GlaxoSmithKline, Janssen, Otsuka and Pfizer, and has received grant support from the Fellowship of Japan Research Foundation for Clinical Pharmacology. Dr Leucht received speaker/consultancy/advisory board honoraria from SanofiAventis, BMS, Eli Lilly, Essex Pharma, Astra-Zeneca, Alkermes, GlaxoSmithKline, Janssen/Johnson & Johnson, Lundbeck, Medavante and Pfizer, SanofiAventis and Eli Lilly supported research projects by SL. Dr Kane has been a consultant to Astra-Zeneca, Janssen, Pfizer, Eli Lilly, Bristol-Myers Squibb, Dainippon Sumitomo/Sepracor/Sunovion, Johnson & Johnson, Otsuka, Vanda, Proteus, Takeda, Targacept, IntraCellular Therapies, Merck, Lundbeck, Novartis, Roche, Rules Based Medicine and Sunovion, and has received honoraria for lectures from Otsuka, Eli Lilly, Esai, Boehringer-Ingelheim, Bristol-Myers Squibb and Janssen. He has received grant support from The National Institute of Mental Health. Dr Correll has been a consultant and/or advisor to or has received honoraria from Actelion, Astra-Zeneca, Bristol-Myers Squibb, Cephalon, Eli Lilly, GSK, IntraCellular Therapies, Ortho-McNeill/Janssen/J&J, Merck, Novartis, Otsuka, Pfizer and Sunovion. He has received grant support from the Feinstein Institute for Medical Research, the National Institute of Mental Health (NIMH), and the National Alliance for Research in Schizophrenia and Depression (NARSAD), BMS, Otsuka and Ortho-McNeill/Janssen/J&J.
Additional information
Part of the data was presented in poster format at the 51st Annual Meeting of the New Clinical Drug Evaluation Unit (NCDEU), Boca Raton, FL, USA, 15 June 2011.
Supplementary Information accompanies the paper on the Molecular Psychiatry website
Supplementary information
Rights and permissions
About this article
Cite this article
Kishimoto, T., Agarwal, V., Kishi, T. et al. Relapse prevention in schizophrenia: a systematic review and meta-analysis of second-generation antipsychotics versus first-generation antipsychotics. Mol Psychiatry 18, 53–66 (2013). https://doi.org/10.1038/mp.2011.143
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mp.2011.143
Keywords
This article is cited by
-
Family Fellowship Society for Psychosocial Rehabilitation Services (1993–2019): A Self-help Movement
Journal of Psychosocial Rehabilitation and Mental Health (2024)
-
Symptomatic, functional and quality of life measures of remission in 194 outpatients with schizophrenia followed naturalistically in a 6-month, non-interventional study of aripiprazole once-monthly
Schizophrenia (2023)
-
Where the public health principles meet the individual: a framework for the ethics of compulsory outpatient treatment in psychiatry
BMC Medical Ethics (2022)
-
Cost analysis of lurasidone for the treatment of schizophrenia in adolescents and adults within the United Kingdom
BMC Health Services Research (2022)
-
Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics
Schizophrenia (2022)