Abstract
Epithelial to mesenchymal transition has been suggested as a relevant contributor to pulmonary fibrosis, but how and where this complex process is triggered in idiopathic pulmonary fibrosis is not fully understood. Beta-tubulin-III (Tubβ3), ZEB1, and β-catenin are partially under the negative control of miR-200, a family of micro-RNAs playing a major role in epithelial to mesenchymal transition, that are reduced in experimental lung fibrosis and idiopathic pulmonary fibrosis. We wonder whether in situ expression of these proteins is increased in idiopathic pulmonary fibrosis, to better understand the significance of miR-200 feedback loop and epithelial to mesenchymal transition. We investigated the immunohistochemical and immunofluorescent expression and precise location of ZEB1, Tubβ3, and β-catenin in tissue samples from 34 idiopathic pulmonary fibrosis cases and 21 controls (5 normal lungs and 16 other interstitial lung diseases). In 100% idiopathic pulmonary fibrosis samples, the three proteins were concurrently expressed in fibroblastic foci, as well in damaged epithelial cells overlying these lesions and in pericytes within neo-angiogenesis areas. These results were also confirmed by immunofluorescence assay. In controls the abnormal expression of the three proteins was absent or limited. This is the first study that relates concurrent expression of Tubβ3, ZEB1, and β-catenin to abnormal epithelial and myofibroblast differentiation in idiopathic pulmonary fibrosis, providing indirect but robust evidence of miR-200 deregulation and epithelial to mesenchymal transition activation in idiopathic pulmonary fibrosis. The abnormal expression and localization of these proteins in bronchiolar fibro-proliferative lesions are unique for idiopathic pulmonary fibrosis, and might represent a disease-specific marker in challenging lung biopsies.
Similar content being viewed by others
Main
Idiopathic pulmonary fibrosis is the most common and severe among idiopathic interstitial pneumonias with a median survival of 3–4 years.1 A growing body of evidence suggests that the development of the disease is related to a progressive loss of regenerative potential of the lung parenchyma due to localized epithelial stem cell failure, derangement of the cross talk between epithelial and mesenchymal components, with eventual triggering of parenchymal fibrosis and abnormal airway remodeling.2, 3 Despite several experimental supports were provided to this picture, there is still a debate on idiopathic pulmonary fibrosis pathogenesis.4, 5 Activation of epithelial mesenchymal transition was proposed as one relevant mechanism leading to pneumocyte loss, myofibroblast accumulation, and lung fibrosis in both human and experimental studies.6, 7, 8 Nevertheless, the pathogenic specificity of epithelial to mesenchymal transition in idiopathic pulmonary fibrosis is still questionable.9 Epithelial to mesenchymal transition can be triggered through different mechanisms,7 including the activation of major signaling pathways (TGF-β, Wnt/β-catenin, Notch, and others), and recent studies revealed a further level of complexity based on the differential expression of micro-RNAs (miRNAs).10, 11 Noticeably, miR-200 family members are downregulated in human and experimental pulmonary fibrosis, and the restoration of miR-200s expression prevents experimental pulmonary fibrosis.12 Inhibition of miR-200s exerts a variety of functions, including the maintenance of epithelial to mesenchymal transition, and enhancement of tumor growth and metastatic spread. miR-200s can regulate epithelial to mesenchymal transition by repressing ZEB1 and ZEB2/SIP1, transcription factors that downregulate E-cadherin and other epithelial markers.13 miR-200 family and its target proteins exert a fundamental influence during primary and secondary alveolarization,14 by suppressing several relevant pathways (TGF-β, Wnt, Notch) that play relevant roles for human lung repair and differentiation,15, 16, 17 and are abnormally activated in experimental and human pulmonary fibrosis.18, 19, 20 ZEB1 expression is upregulated by Wnt and TGFβ pathways and repressed by Grainyhead-like-2 (GRHL2), a transcriptional factor dysregulated in idiopathic pulmonary fibrosis as well.21
Noticeably, also class III β-tubulin (Tubβ3) expression, a common mechanism of resistance to microtubule-targeting agents in many types of cancer, is under the control of miR-200s.22 Recent evidence has been provided that microtubules and tubulins are key players at the early phases of epithelial to mesenchymal transition, since microtubule disruption is crucial by inducing basement membrane breakdown, and tubulins are involved in the regulation of cell polarity and migration,23 and Tubβ3 expression is stimulated in some experimental systems by TGFβ.24 Although data concerning the expression of β-catenin in idiopathic pulmonary fibrosis are already available,18, 19 information regarding ZEB1 and Tubβ3 are still scanty.25 On this basis we investigated the expression of these proteins in lung tissue samples of idiopathic pulmonary fibrosis compared with controls. Since ZEB1 and β-catenin, but not Tubβ3, are well known to be linked to epithelial to mesenchymal transition activation, we investigated this issue using previously established cell lines.26, 27
Materials and methods
Histological and Immunohistochemical Analysis on Lung Samples
All samples were routinely fixed in buffered formalin, embedded in paraffin, and stained with hematoxylin and eosin following histological procedures. The study group consisted of 34 previously untreated cases, with clinical, radiographic, and physiologic findings consistent with a diagnosis of idiopathic pulmonary fibrosis.1 Histological examination of lung biopsies (30 surgical lung biopsies and 4 transbronchial cryobiopsies)28 revealed all the major features of usual interstitial pneumonia according to recently defined criteria.1 Control samples included normal lung tissue (n=5 samples of unaffected tissue from patients submitted to large excisions for lung carcinoma), and 16 biopsies with non-idiopathic pulmonary fibrosis interstitial lung diseases: diffuse alveolar damage (5 cases), nonspecific interstitial pneumonia (5 cases), chronic hypersensitivity pneumonitis (3 cases), desquamative interstitial pneumonia (2 cases) and cryptogenic organizing pneumonia (6 cases).
Representative blocks from all specimens were immunostained with a monoclonal antibody recognizing Tubβ3 (clone TUJ1; Covance), a polyclonal antibody recognizing ZEB1 (rabbit; Sigma Chem.), and a monoclonal antibody recognizing β-catenin (clone 15B8; Sigma Chem.). Heat-induced antigen retrieval (citrate buffer 0.01 M pH 6.0 for 30 min) and immunostaining were performed within an automated Bond immunostainer (Vision-Biosystem/Leica) using a sensitive ‘Bond-polymer-Refine’ detection system. Sections incubated without the primary antibody served as negative controls.
To better define the nature of the epithelial and mesenchymal cells expressing the three proteins ZEB1, Tubβ3, and β-catenin a panel of markers was utilized, with either two-marker immunoenzymatic or immunofluorescence protocols on selected cases (5) based on tissue availability and fixation quality. The panel included antibodies recognizing Twist, a nuclear transcription factor related to epithelial to mesenchymal transition (clone Twist2C1a; Santa Cruz Biotechnology),29 α-smooth muscle actin (α-SMA) (clone 1A4; Dako), E-cadherin (clone NCH38; Dako), tenascin (clone TN2; Dako), nuclear antigen specific for endothelial cells LMO230 (clone 229BC; Abcam) and ERG (clone EPR3864; Epitomics), the type-II pneumocyte markers Surfactant protein A (clone 32E12; Novocastra), and ABCA3 (clone 17-H5-24; Seven Hills Bioreagents); bronchiolar basal cell markers such as cytokeratin-5 (clone XM26; Novocastra), and ΔN-p63 (clone p40; Biocare), the macrophage marker CD68 (clone PG-M1; Dako), the epithelial cell marker cytokeratin-8 (clone TS1; Novocastra), the cellular senescence-related marker p16 (clone JC8; Santa Cruz Biotechnology), and Cathepsin-K, a marker of epithelioid macrophages and granulomas (clone 3F9; Abcam).31
Immunofluorescence
Selected pairs of markers (Tubβ3/ZEB1, Tubβ3/p63, and ZEB1/cytokeratin-8) were investigated on paraffin-embedded 3-μm-thick sections. Antigen retrieval was performed in pre-warmed citrate buffer (pH 6 temp. 95 °C) for 30 min. The sections were incubated with a protein block serum-free solution for 15 min to block nonspecific binding. After 1 h incubation with the primary antibody, slides were incubated with the secondary antibodies (anti-mouse or anti-rabbit Ig) conjugated with either Alexa-488 or Alexa-546 (1:800; Invitrogen Molecular Probe). Reduction of the autofluorescence was performed by incubation with Sudan Black B 0.1% (Sigma-Aldrich). Nuclei were stained with Prolong Gold anti-fade reagent with DAPI (Invitrogen Molecular Probe).
Results
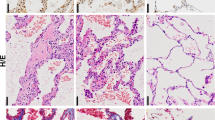
Tubβ3, ZEB1 and β-Catenin Expression in Idiopathic Pulmonary Fibrosis/Usual Interstitial Pneumonia Samples
In all investigated idiopathic pulmonary fibrosis/usual interstitial pneumonia samples Tubβ3, ZEB1 and nuclear β-catenin immunoreactivity was variably distributed in areas characterized by parenchymal damage and abnormal remodeling as following.
Areas of alveolar damage in idiopathic pulmonary fibrosis
In all cases variable concurrent expression of the three molecules was demonstrated in areas where alveolar damage was observed. Alveolar damage was characterized by the presence of pneumocyte type-II hyperplasia, with cell enlargement and mild atypia, appearing as either isolated gland-like clusters enclosed in a dense fibrotic tissue, or linear rows of alveolar epithelial cells lying on variably thickened interstitial structures (Figure 1a). These areas often contain blood vessels and a variable inflammatory infiltrate. The expression of TTF1, surfactant protein-A, and/or ABCA3 was used to confirm the pneumocyte type-II nature of these damaged cells (Figure 1b and c). Most type-II pneumocytes in damaged alveoli expressed diffuse cytoplasmic Tubβ3 and nuclear β-catenin (Figure 1c and d) while those expressed nuclear ZEB1 were a minority. The epithelial nature of ZEB1 immunoreactive cells was confirmed by co-expression of cytokeratin-8 by double-marker immunohistochemistry and immunofluorescence (Figure 1e and f). Most cytokeratin-negative stromal cells, including blood vessels and fibroblasts, exhibited strong nuclear ZEB1 immunoreactivity (Figure 1e). Tubβ3 and ZEB1 were not expressed in epithelial cells of normal parenchyma, whereas β-catenin was expressed, but invariably membranous. Hyperplastic pneumocytes in these lesions expressed reduced E-cadherin, the cell-senescence-associated protein p16 (Figure 1g and h), and were variably positive for markers related to cell migration and/or activation, such as heath-shock protein-27, Laminin-5 γ-2 chain, and CK14.
Alveolar damage in idiopathic pulmonary fibrosis. Alveolar damage is constantly observed in involved areas of idiopathic pulmonary fibrosis samples, as hyperplastic type-II pneumocytes (a, green arrows) and/or gland-like epithelial structures embedded in collagenized stroma (a, yellow arrows). Gland-like epithelial structures, formed by hyperplastic/atypical ABCA3+ (b) pneumocytes, are embedded in a dense collagen-rich stroma containing numerous blood vessels and a variable chronic inflammatory infiltrate. These alveolar epithelial remnants express at high levels of Tubβ3 (c, red; nuclear TTF1, brown), nuclear β-catenin (d), and, at lower levels, ZEB1 (e, f). The epithelial nature of ZEB1+ cells is confirmed by double-marker analyses with CK8 expression (nuclear ZEB1, brown and CK8, red, at immunohistochemistry; nuclear ZEB1, green, CK8, red, at immunofluorescence). The same alveolar epithelial clusters express low levels of the epithelial to mesenchymal transition-related protein E-cadherin (g), and high levels of the cellular senescence-related protein p16 (h).
Normal areas in idiopathic pulmonary fibrosis samples, including bronchiolar and alveolar components, were identical to normal samples for all three molecules investigated.
Blood vessels
At sites of alveolar damage and early fibrosis, consisting of fibroblasts and myofibroblasts, Tubβ3 decorated a large proportion of small blood vessels (Figure 2a) located around epithelial remnants and fibroblastic foci. Double-marker analysis using Tubβ3 and endothelial markers like ERG and LMO2 clearly demonstrated that Tubβ3-expressing cells in vascular structures were in fact ERG/LMO2-negative pericytes (Figure 2b and c). These vessels were numerous around damaged alveolar structures in areas of dense fibrosis (Figure 2a), near fibroblastic foci in micro-honeycomb lesions, and also in areas where smooth muscle hyperplasia, osseous metaplasia, and/or subpleural fatty metaplasia were present (Figure 2d and e).
Angiogenesis in idiopathic pulmonary fibrosis. Numerous Tubβ3+ blood vessels are present within affected tissue areas in idiopathic pulmonary fibrosis, frequently surrounding alveolar remnants (a). Double-marker analysis of Tubβ3 (red) together with the endothelial marker ERG (nuclear, brown) (b, arrows) LMO2 (nuclear, brown) clearly demonstrate that Tubβ3+ cells are in fact pericytes, surrounded by Tubβ3-negative, LMO2+ endothelial cells (c, arrows). Tubβ3+ blood vessels are also frequently observed around foci of osseous metaplasia when present (d), and in areas of smooth muscle hyperplasia (e, Tubβ3+ red, α-smooth muscle actin, brown).
Fibroblastic foci
Both myofibroblasts and their overlying epithelial cells were intensely Tubβ3 positive in fibroblastic foci (Figure 3a). The myofibroblast nature of Tubβ3-expressing cells in these lesions was confirmed by morphology and by the co-expression of α-SMA and the extracellular matrix protein tenascin. Tubβ3+ myofibroblasts in fibroblastic foci also expressed nuclear β-catenin, as previously demonstrated,18 and the epithelial to mesenchymal transition-related proteins Twist and ZEB1, as shown by double-marker immunohistochemical and immunofluorescence analyses (Figure 3b–d).
Fibroblastic foci. Strong Tubβ3 expression in fibroblastic foci: the protein is expressed by both myofibroblasts and overlying bronchiolar epithelial cells (a). Myofibroblasts in a fibroblast focus express both Tubβ3 (red immunostain) and the epithelial to mesenchymal transition-related transcription factor Twist (dark brown immunostain) (b). Co-expression of ZEB1 (nuclear, dark brown immunostain) and Tubβ3 (red immunostain) in myofibroblasts (c), as also confirmed by immunofluorescence analysis (d, ZEB1, green fluorescence; Tubβ3, red fluorescence; arrows).
Micro-honeycombing
Most Tubβ3+ fibroblastic foci were located within areas of micro-honeycombing (Figure 4a and b) in association with short segments of bronchiolar epithelium exhibiting diffuse expression of Tubβ3, in both basal and luminal cells as demonstrated by immunohistochemistry and immunofluorescence using the basal cell markers ΔN-p63 and CK5 (Figure 4c–e). Tubβ3+ expression in honeycomb cysts was heterogeneous, with alternate segments of either Tubβ3 positive or negative epithelium (Figure 4f). The three major Tubβ3+ elements involved in tissue remodeling of idiopathic pulmonary fibrosis, namely fibroblastic foci, bronchiolar abnormal epithelial cells, and damaged alveoli were often closely located in remodeled lung parenchyma (Figure 5a). Tubβ3+ expression was demonstrated in bronchiolar epithelial cells, either basal or luminal, exhibiting morphological and molecular changes (loss of cilia and cuboidal shape in luminal cells, occurrence of ΔN-p63+ enlarged nuclei in basal cells). These basal cells co-expressed the senescence-marker p16 (Figure 5b), as well as molecules related to cell migration and activation (heath-shock protein-27, laminin-5-γ-2 chain, and cytokeratin-14) (Figure 5c–e). In honeycomb lesions, Tubβ3 decorated severely modified portions of bronchiolar structures, characterized by epithelial distortion, fibrosis, and angiogenesis (Figure 5f).
Honeycomb lesions. Tubβ3 is widely expressed in honeycomb lesions of two idiopathic pulmonary fibrosis samples (a, b). In bronchiolar epithelial cells the Tubβ3 expression is heterogeneous, but mostly parallels the underlying fibrotic reaction (Tubβ3, red; αSMA, brown) (c). In (d) a bronchiolar lesion overlying a fibroblast focus is shown: strong Tubβ3 immunoreactivity (brown, bold arrow) is demonstrated in myofibroblasts, and ΔN-p63+ basal cells (red nuclei, arrow). The basal cell nature of Tubβ3+ cells in a bronchiolar lesion is confirmed by immunofluorescence with Tubβ3 (red fluorescence) and ΔN-p63 (nuclear, green fluorescence) (e and f, at different magnifications).
Honeycomb lesions, molecular abnormalities. Strong Tubβ3 expression is observed in different lesions recapitulating the sequential events of tissue remodeling in idiopathic pulmonary fibrosis (as described,36 including alveolar damage (green arrows), fibroblastic foci (ff) and overlying bronchiolar epithelium (red arrow) (a). The bronchiolar epithelial cells overlying the fibroblast focus in a honeycomb lesion express at high levels of the cellular senescence-marker p16. Also the underlying myofibroblasts show variable p16 immunoreactivity (b, arrows). The basal epithelial cells in the same bronchiolar lesion express the migratory markers lamin-5 γ-2 chain (c, arrow) and hsp27 (d, arrow), as previously demonstrated.21 CK14 is aberrantly expressed in basal cell clusters within severely distorted bronchiolar structures ((e), CK14 red immunostain, ΔN-p63 brown immunostain—arrow) that also express high levels of Tubβ3 ((f), Tubβ3 brown immunostain, ΔN-p63 red).
Tubβ3 and ZEB1 Expression in Normal Control Lung and other Lung Diseases
Normal adult lung
In all samples of normal adult lung Tubβ3 expression was absent with the sole exception of thin interstitial nerve fibers (Figure 6a) while ZEB1 was widely expressed in mesenchymal cells.
Control lung samples. Complete lack of Tubβ3 expression in normal lung parenchyma (arrow: thin nerve fibers as an internal positive control) (a). Strong linear Tubβ3 expression decorates pneumocyte damage/repair in a case of nonspecific interstitial pneumonia (arrow) (b); focal expression of Tubβ3 (red immunostain) in a case of chronic hypersensitivity pneumonitis; an associated giant cell macrophage is evidenced by anti-cathepsin-k antibody (brown immunostain) (c); minimal focal Tubβ3 expression in a case of desquamative interstitial pneumonia (arrow) (d); strong Tubβ3 immunostaining in a Masson’s polyp of organizing pneumonia is evidenced in both myofibroblasts and regenerating pneumocytes (e). Diffuse and intense Tubβ3 expression in a case of diffuse alveolar damage (f).
Nonspecific interstitial pneumonia (five cases)
Variable expression of Tubβ3 was observed in nonspecific interstitial pneumonia from almost negative (two cases) to positive (three cases). In the positive cases Tubβ3 expression was confined to short lines of pneumocytes at sites of alveolar damage (Figure 6b). Vascular structures containing Tubβ3-expressing pericytes were either absent or rare. ZEB1 immunoreactivity was evidenced in mesenchymal cells, as in normal lung samples.
Chronic hypersensitivity pneumonia (three cases)
Tubβ3 immunoreactivity was negative in two cases, with focal expression in areas of epithelial damage observed around small cathepsin-k positive epithelioid macrophages (Figure 6c). In the third case characterized by usual interstitial pneumonia pattern the fibroblastic foci were Tubβ3 positive.
ZEB1 expression was comparable to that observed in normal control samples.
Desquamative interstitial pneumonia (two cases)
Low focal Tubβ3 immunoreactivity was observed in both cases (Figure 6d). ZEB1 expression was comparable to that observed in normal control samples.
Cryptogenic organizing pneumonia (five cases)
In all five cases, expression of cytoplasmic Tubβ3 and nuclear ZEB1 was observed in myofibroblasts forming Masson’s polyps (Figure 6e).
Diffuse alveolar damage (five cases)
Strong signal was observed for Tubβ3 protein at immunohistochemical and western blot analyses in all diffuse alveolar damage samples, always higher than in idiopathic pulmonary fibrosis (Figure 6f and Supplementary Figure SE1). The expression of Tubβ3 was widespread, in both interstitial myofibroblasts and hyperplastic type-II pneumocytes. ZEB1 was widely distributed in fibroblasts/myofibroblasts and blood vessels in thickened interstitial spaces, with variable but consistent staining in the nuclei of hyperplastic pneumocytes.
Lung adenocarcinoma
Variable expression of Tubβ3 was demonstrated in lung adenocarcinoma cells, ranging from negative to strongly positive (Supplementary Figure SE1). ZEB1 was only focally expressed in one of five investigated cases.
Discussion
The main hypothesis investigated in this study is that three target proteins of the miR-200-family, namely Tubβ3, ZEB1 and β-catenin, can contribute to the complex sequence of molecular and cellular events characterizing the pathogenesis of idiopathic pulmonary fibrosis. miR-200s are known to control each of these three proteins, exerting a variety of functions, including the maintenance of epithelial to mesenchymal transition, tumor growth, cancer cell migration and invasion. Furthermore, miR-200s play important roles in the development and differentiation of human lung epithelium.10, 11, 12, 14 The reliability of this hypothesis is warranted, since both the aberrant recapitulation of developmental programs and epithelial to mesenchymal transition have been proposed as relevant factors in the pathogenesis of idiopathic pulmonary fibrosis. Methodologically, the demonstration of target proteins of miRNA-200s may provide relevant new information, since the in situ investigation of microRNA is technically cumbersome, and cannot easily provide precise localization of the complex molecular networks involved in abnormal lung tissue remodeling. Our work provides strong evidence that the three proteins are abnormally expressed at sites of damage and repair in idiopathic pulmonary fibrosis, with peculiar distribution in fibroblastic foci and epithelial cells of honeycomb areas (Figures 2 and 3). As already suggested, ZEB1 is a crucial activator of epithelial to mesenchymal transition, and its expression in epithelial cells is triggered by different signaling pathways and transcription factors, including Wnt-β catenin, TGFβ, and Twist, all molecules upregulated in idiopathic pulmonary fibrosis.21, 29
We also demonstrated that Tubβ3, a tubulin isoform mostly expressed in neuronal-type tissues under the control of miR-200s,22 is strongly expressed at sites of alveolar damage and fibrosis in all diffuse alveolar disease and idiopathic pulmonary fibrosis samples of our series. We also showed using established epithelial to mesenchymal transition protocols with lung carcinoma and hepatoma cell lines (see the Supplementary Information) that Tubβ3 expression is related to epithelial to mesenchymal transition (see Supplementary Figure SE1). The immunohistochemical expression of Tubβ3 in idiopathic pulmonary fibrosis was strong but strictly confined at sites of early fibrosis and epithelial damage. This latter observation explains why low Tubβ3 expression was evidenced by Western blot in idiopathic pulmonary fibrosis samples, differently from diffuse alveolar disease (see Supplementary Figure SE1). In particular, we clearly demonstrated that Tubβ3 expression is precisely localized in fibroblastic foci, where the epithelial to mesenchymal transition-related transcription factors ZEB1 and Twist are also expressed. Fibroblastic foci are lens-shaped collections of spindled α-SMA+ myofibroblasts, covered by sheets of epithelial cells. These lesions are considered the histological hallmark of active disease, where ongoing parenchyma destruction and abnormal tissue renewal take place.32 Interestingly, double-marker analysis in our study clearly showed that, within these lesions, both myofibroblasts and epithelial cells co-express Tubβ3 and nuclear β-catenin. β-catenin is the final transcription factor of the canonical Wnt-signaling: a pathway playing a relevant role in epithelial to mesenchymal transition that is abnormally activated in experimental pulmonary fibrosis and human idiopathic pulmonary fibrosis.18, 19
The abnormal expression of these three proteins was observed in all the major morphological changes characterizing tissue remodeling in this disease, namely (i) activated type-II pneumocytes in parenchyma, (ii) fibroblastic foci, and (iii) the bronchiolar proliferative lesions in honeycomb cysts.33, 34, 35 Alveolar damage is widely recognized as the first pathogenic event in the development of idiopathic pulmonary fibrosis, either related to intrinsic genetic defects, as in familial cases, or due to the progressive regenerative failure of lung epithelial progenitors.2, 3, 36, 37 Cell senescence has been proposed as a key mechanism of early alveolar damage in idiopathic pulmonary fibrosis.3, 36, 37 Accordingly, the alveolar epithelial remnants expressing β-catenin, Tubβ3, and ZEB1 in most specimens of our study expressed p16 (Figure 5), an established marker of cell senescence.38 The co-expression of p16 with β-catenin and Tubβ3 was also evidenced in fibroblastic foci and bronchiolar epithelial lesions (Figure 5a and b). A possible explanation of this observation is that all these lesions develop as a consequence of the aberrant signaling triggered by alveolar damage (eg by paracrine Wnt/β-catenin pathway acting as an oncogene activating cell senescence).39, 40 Interestingly, cell senescence in aging may affect the miRNA signature, thus altering the fibroblast phenotype and promoting lung fibrosis.11
Within honeycomb lesions Tubβ3 and nuclear β-catenin were expressed in linear clusters of bronchiolar basal cells (recognized by cytokeratin-5 and ΔN-p63 immunoreactivity) overlying fibroblastic foci. As we showed in previous studies,41 these bronchiolar lesions (for which we proposed the nick-name ‘sandwich foci’ for their peculiar three-layered morphology) abnormally express a variety of molecules related to cell proliferation, cellular senescence, epithelial to mesenchymal transition, mechanical strain, and cell migration, and likely represent key elements in the abnormal lung remodeling characterizing idiopathic pulmonary fibrosis (Figures 4 and 5).18, 41 Accordingly, a recent study demonstrated that basal bronchiolar cells in idiopathic pulmonary fibrosis and in culture acquire mesenchymal features.42 The relationship between Tubβ3 and epithelial to mesenchymal transition, as well as with deranged mechanisms of epithelial damage and repair, may represent relevant new information in understanding the significance of its abnormal expression, not only in fibrosing lung diseases but also in drug resistance of human carcinoma.43 In fact, the expression of different β-tubulin isotypes is disrupted in cancer cells, and understanding how this contributes to disease progression and drug resistance is essential.
Another interesting new observation of our study is that Tubβ3 is expressed at high levels in blood vessels neighboring fibroblastic foci in idiopathic pulmonary fibrosis, differently from a variety of control lung samples where vascular Tubβ3 expression was either not observed, or minimal. Double-marker analysis clearly showed that Tubβ3-expressing cells are not endothelial cells, but pericytes, a cell type recently proposed as related to active angiogenesis when expresses Tubβ3.44 Interestingly, miR-200 family can contribute to regulate tumor angiogenesis,45 and the role of Tubβ3 expression in this mechanism and its possible pharmacological inhibition warrants further evaluation. This finding is the first in situ evidence of the previously proposed occurrence of abnormal angiogenesis and vascular remodeling occurring in idiopathic pulmonary fibrosis and its precise evaluation on tissue samples can be facilitated in our view by Tubβ3 immunostaining. The translational relevance of such observation is warranted since deregulated production of angiogenic mediators (eg gremlin, a potent inhibitor of the bone morphogenetic protein pathway) may potentially lead to pulmonary hypertension.46
The possible derangement of cross talk between epithelial and mesenchymal cells in idiopathic pulmonary fibrosis, as proposed by several groups, likely involves mesenchymal stem cells recruitment in affected lung parenchyma. Mesenchymal precursors reside in perivascular niches, and can differentiate into different cell lineages including adipocytes, osteoblasts, and myofibroblasts.47, 48 Tubβ3 can be induced in mesenchymal stem cells, and this finding was previously interpreted as ‘neuronal trans-differentiation’.49, 50 Nevertheless, this notion has been challenged, since despite the neuronal-like morphology and neural protein expression, Tubβ3-expressing mesenchymal stem cells do not acquire basic functional neuronal properties.47 Indeed, several lines of evidence have been recently provided, demonstrating that Tubβ3 is expressed by mesenchymal precursors.49 The observation that Tubβ3 is expressed at high levels in pericytes and myofibroblasts suggests that this molecule may represent a marker of a particular step in mesenchymal cell differentiation. In fact, Tubβ3 is conserved in myofibroblasts forming young lesions, but not expressed in more differentiated mesenchymal cells (fibroblasts, endothelial cells, smooth muscle cells, adipocytes, etc). Pericytes may thus represent a key element in the pathogenesis of idiopathic pulmonary fibrosis,51 representing a major source for the variety of stromal components that accumulate in idiopathic pulmonary fibrosis affected lung parenchyma, explaining the abnormal accumulation of differentiated mesenchymal components, including smooth muscle hyperplasia, sub-pleural fatty metaplasia, and also osseous metaplasia (Figure 2).52, 53 Thus, our study extends previous observations and indirectly confirms the role of the miR-200/epithelial to mesenchymal transition axis in the pathogenesis of idiopathic pulmonary fibrosis, highlighting the concurrent role of miR-200 target proteins ZEB1, Tubβ3, and β-catenin at sites of ongoing epithelial damage and fibrosis. According to our findings, dysregulated miR-200/epithelial to mesenchymal transition axis in idiopathic pulmonary fibrosis can severely affect both the epithelial (either alveolar and/or bronchiolar) and mesenchymal components of lung tissue, and may represent a potential target for new treatments (eg using the existing variety of β-catenin and tubulin-interfering substances).
Finally, we would like to propose Tubβ3 expression as a robust marker of epithelial damage and repair in lung tissues, with potential diagnostic utility if properly validated. In all control cases in fact Tubβ3 expression closely paralleled the occurrence of epithelial damage and early fibrosis and clearly showed even at low microscope magnifications the type and extent of histological changes. This approach may provide higher levels of specificity in new diagnostic scenarios where more invasive surgical lung biopsy will be progressively replaced by less harmful means, such as cryobiopsies.54
References
Raghu G, Collard HR, Egan JJ et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011;183:788–824.
Selman M, Pardo A, Kaminski N . Idiopathic pulmonary fibrosis: aberrant recapitulation of developmental programs? PLoS Med 2008;5:e62.
Chilosi M, Doglioni C, Murer B et al. Epithelial stem cell exhaustion in the pathogenesis of idiopathic pulmonary fibrosis. Sarcoidosis Vasc Diffuse Lung Dis 2010;27:7–18.
Alder JK, Barkauskas CE, Limjunyawong N et al. Telomere dysfunction causes alveolar stem cell failure. Proc Natl Acad Sci USA 2015;112:5099–5104.
Povedano JM, Martinez P, Flores JM et al. Mice with pulmonary fibrosis driven by telomere dysfunction. Cell Rep 2015;12:286–299.
Wu Z, Yang L, Cai L et al. Detection of epithelial to mesenchymal transition in airways of a bleomycin induced pulmonary fibrosis model derived from an alpha-smooth muscle actin-Cre transgenic mouse. Respir Res 2007;8:1.
Gonzalez DM, Medici D . Signaling mechanisms of the epithelial-mesenchymal transition. Sci Signal 2014;7:re8.
Willis BC, Liebler JM, Luby-Phelps K et al. Induction of epithelial-mesenchymal transition in alveolar epithelial cells by transforming growth factor-beta1: potential role in idiopathic pulmonary fibrosis. Am J Pathol 2005;166:1321–1332.
Rock JR, Barkauskas CE, Cronce MJ et al. Multiple stromal populations contribute to pulmonary fibrosis without evidence for epithelial to mesenchymal transition. Proc Natl Acad Sci USA 2011;108:E1475–E1483.
Gregory PA, Bracken CP, Bert AG et al. MicroRNAs as regulators of epithelial-mesenchymal transition. Cell Cycle 2008;7:3112–3118.
Nho RS . Alteration of aging-dependent microRNAs in idiopathic pulmonary fibrosis. Drug Dev Res 2015;76:343–353.
Yang S, Banerjee S, de Freitas A et al. Participation of miR-200 in pulmonary fibrosis. Am J Pathol 2012;180:484–493.
Gregory PA, Bert AG, Paterson EL et al. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat Cell Biol 2008;10:593–601.
Benlhabib H, Guo W, Pierce BM et al. The miR-200 family and its targets regulate type II cell differentiation in human fetal lung. J Biol Chem 2015;290:22409–22422.
Caprioli A, Villasenor A, Wylie LA et al. Wnt4 is essential to normal mammalian lung development. Dev Biol 2015;406:222–234.
Vallejo DM, Caparros E, Dominguez M . Targeting Notch signalling by the conserved miR-8/200 microRNA family in development and cancer cells. EMBO J 2011;30:756–769.
Brabletz S, Bajdak K, Meidhof S et al. The ZEB1/miR-200 feedback loop controls Notch signalling in cancer cells. EMBO J 2011;30:770–782.
Chilosi M, Poletti V, Zamo A et al. Aberrant Wnt/beta-catenin pathway activation in idiopathic pulmonary fibrosis. Am J Pathol 2003;162:1495–1502.
Konigshoff M, Balsara N, Pfaff EM et al. Functional Wnt signaling is increased in idiopathic pulmonary fibrosis. PLoS One 2008;3:e2142.
Zhou B, Liu Y, Kahn M et al. Interactions between beta-catenin and transforming growth factor-beta signaling pathways mediate epithelial-mesenchymal transition and are dependent on the transcriptional co-activator cAMP-response element-binding protein (CREB)-binding protein (CBP). J Biol Chem 2012;287:7026–7038.
Cieply B, Farris J, Denvir J et al. Epithelial-mesenchymal transition and tumor suppression are controlled by a reciprocal feedback loop between ZEB1 and Grainyhead-like-2. Cancer Res 2013;73:6299–6309.
Cochrane DR, Spoelstra NS, Howe EN et al. MicroRNA-200c mitigates invasiveness and restores sensitivity to microtubule-targeting chemotherapeutic agents. Mol Cancer Ther 2009;8:1055–1066.
Whipple RA, Matrone MA, Cho EH et al. Epithelial-to-mesenchymal transition promotes tubulin detyrosination and microtentacles that enhance endothelial engagement. Cancer Res 2010;70:8127–8137.
Chung EJ, Chun JN, Jung SA et al. TGF-beta-stimulated aberrant expression of class III beta-tubulin via the ERK signaling pathway in cultured retinal pigment epithelial cells. Biochem Biophys Res Commun 2011;415:367–372.
Park JS, Park HJ, Park YS et al. Clinical significance of mTOR, ZEB1, ROCK1 expression in lung tissues of pulmonary fibrosis patients. BMC Pulm Med 2014;14:168.
Sagmeister S, Eisenbauer M, Pirker C et al. New cellular tools reveal complex epithelial-mesenchymal interactions in hepatocarcinogenesis. Br J Cancer 2008;99:151–159.
van Zijl F, Mall S, Machat G et al. A human model of epithelial to mesenchymal transition to monitor drug efficacy in hepatocellular carcinoma progression. Mol Cancer Ther 2011;10:850–860.
Casoni GL, Tomassetti S, Cavazza A et al. Transbronchial lung cryobiopsy in the diagnosis of fibrotic interstitial lung diseases. PLoS One 2014;9:e86716.
Pozharskaya V, Torres-Gonzalez E, Rojas M et al. Twist: a regulator of epithelial-mesenchymal transition in lung fibrosis. PLoS One 2009;4:e7559.
Gratzinger D, Zhao S, West R et al. The transcription factor LMO2 is a robust marker of vascular endothelium and vascular neoplasms and selected other entities. Am J Clin Pathol 2009;131:264–278.
Reghellin D, Poletti V, Tomassett S et al. Cathepsin-K is a sensitive immunohistochemical marker for detection of micro-granulomas in hypersensitivity pneumonitis. Sarcoidosis Vasc Diffuse Lung Dis 2010;27:57–63.
Katzenstein AL, Zisman DA, Litzky LA et al. Usual interstitial pneumonia: histologic study of biopsy and explant specimens. Am J Surg Pathol 2002;26:1567–1577.
Chilosi M, Poletti V, Murer B et al. Abnormal re-epithelialization and lung remodeling in idiopathic pulmonary fibrosis: the role of deltaN-p63. Lab Invest 2002;82:1335–1345.
Plantier L, Crestani B, Wert SE et al. Ectopic respiratory epithelial cell differentiation in bronchiolised distal airspaces in idiopathic pulmonary fibrosis. Thorax 2011;66:651–657.
Seibold MA, Smith RW, Urbanek C et al. The idiopathic pulmonary fibrosis honeycomb cyst contains a mucocilary pseudostratified epithelium. PLoS One 2013;8:e58658.
Thannickal VJ . Mechanistic links between aging and lung fibrosis. Biogerontology 2013;14:609–615.
Chilosi M, Carloni A, Rossi A et al. Premature lung aging and cellular senescence in the pathogenesis of idiopathic pulmonary fibrosis and COPD/emphysema. Transl Res 2013;162:156–173.
Campisi J . Aging, cellular senescence, and cancer. Annu Rev Physiol 2013;75:685–705.
Campisi J, Andersen JK, Kapahi P et al. Cellular senescence: a link between cancer and age-related degenerative disease? Semin Cancer Biol 2011;21:354–359.
Kovacs T, Csongei V, Feller D et al. Alteration in the Wnt microenvironment directly regulates molecular events leading to pulmonary senescence. Aging Cell 2014;13:838–849.
Chilosi M, Zamo A, Doglioni C et al. Migratory marker expression in fibroblast foci of idiopathic pulmonary fibrosis. Respir Res 2006;7:95.
Jonsdottir HR, Arason AJ, Palsson R et al. Basal cells of the human airways acquire mesenchymal traits in idiopathic pulmonary fibrosis and in culture. Lab Invest 2015;95:1418–1428.
Zhang HL, Ruan L, Zheng LM et al. Association between class III beta-tubulin expression and response to paclitaxel/vinorebine-based chemotherapy for non-small cell lung cancer: a meta-analysis. Lung Cancer 2012;77:9–15.
Stapor PC, Murfee WL . Identification of class III beta-tubulin as a marker of angiogenic perivascular cells. Microvasc Res 2012;83:257–262.
Pecot CV, Rupaimoole R, Yang D et al. Tumour angiogenesis regulation by the miR-200 family. Nat Commun 2013;4:2427.
Farkas L, Gauldie J, Voelkel NF et al. Pulmonary hypertension and idiopathic pulmonary fibrosis: a tale of angiogenesis, apoptosis, and growth factors. Am J Respir Cell Mol Biol 2011;45:1–15.
Campagnolo P, Cesselli D, Al Haj Zen A et al. Human adult vena saphena contains perivascular progenitor cells endowed with clonogenic and proangiogenic potential. Circulation 2010;121:1735–1745.
Wong SP, Rowley JE, Redpath AN et al. Pericytes, mesenchymal stem cells and their contributions to tissue repair. Pharmacol Ther 2015;151:107–120.
Foudah D, Monfrini M, Donzelli E et al. Expression of neural markers by undifferentiated mesenchymal-like stem cells from different sources. J Immunol Res 2014;2014:987678.
Sanchez-Ramos J, Song S, Cardozo-Pelaez F et al. Adult bone marrow stromal cells differentiate into neural cells in vitro. Exp Neurol 2000;164:247–256.
Hung C, Linn G, Chow YH et al. Role of lung pericytes and resident fibroblasts in the pathogenesis of pulmonary fibrosis. Am J Respir Crit Care Med 2013;188:820–830.
Ohta K, Mortenson RL, Clark RA et al. Immunohistochemical identification and characterization of smooth muscle-like cells in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 1995;152:1659–1665.
Kim TS, Han J, Chung MP et al. Disseminated dendriform pulmonary ossification associated with usual interstitial pneumonia: incidence and thin-section CT-pathologic correlation. Eur Radiol 2005;15:1581–1585.
Lee HJ, Bao J, Miller A et al. Structure-based discovery of novel small molecule Wnt signaling inhibitors by targeting the cysteine-rich domain of Frizzled. J Biol Chem 2015;290:30596–30606.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Modern Pathology website
Supplementary information
Rights and permissions
About this article
Cite this article
Chilosi, M., Caliò, A., Rossi, A. et al. Epithelial to mesenchymal transition-related proteins ZEB1, β-catenin, and β-tubulin-III in idiopathic pulmonary fibrosis. Mod Pathol 30, 26–38 (2017). https://doi.org/10.1038/modpathol.2016.147
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2016.147
This article is cited by
-
Flt1 produced by lung endothelial cells impairs ATII cell transdifferentiation and repair in pulmonary fibrosis
Cell Death & Disease (2023)
-
Integrative omics analysis identifies biomarkers of idiopathic pulmonary fibrosis
Cellular and Molecular Life Sciences (2022)
-
The pathogenic role of epithelial and endothelial cells in early-phase COVID-19 pneumonia: victims and partners in crime
Modern Pathology (2021)
-
ZEB1: New advances in fibrosis and cancer
Molecular and Cellular Biochemistry (2021)
-
Augmenting canonical Wnt signalling in therapeutically inert cells converts them into therapeutically potent exosome factories
Nature Biomedical Engineering (2019)