Abstract
Resolution of severe Respiratory Syncytial Virus (RSV)-induced bronchiolitis is mediated by alternatively activated macrophages (AA-Mφ) that counteract cyclooxygenase (COX)-2-induced lung pathology. Herein, we report that RSV infection of 5-lipoxygenase (LO)−/− and 15-LO−/− macrophages or mice failed to elicit AA-Mφ differentiation and concomitantly exhibited increased COX-2 expression. Further, RSV infection of 5-LO−/− mice resulted in enhanced lung pathology. Pharmacologic inhibition of 5-LO or 15-LO also blocked differentiation of RSV-induced AA-Mφ in vitro and, conversely, treatment of 5-LO−/− macrophages with downstream products, lipoxin A4 and resolvin E1, but not leukotriene B4 or leukotriene D4, partially restored expression of AA-Mφ markers. Indomethacin blockade of COX activity in RSV-infected macrophages increased 5-LO and 15-LO, as well as arginase-1 mRNA expression. Treatment of RSV-infected mice with indomethacin also resulted not only in enhanced lung arginase-1 mRNA expression and decreased COX-2, but also decreased lung pathology in RSV-infected 5-LO−/− mice. Treatment of RSV-infected cotton rats with a COX-2-specific inhibitor resulted in enhanced lung 5-LO mRNA and AA-Mφ marker expression. Together, these data suggest a novel therapeutic approach for RSV that promotes AA-Mφ differentiation by activating the 5-LO pathway.
Similar content being viewed by others
Introduction
Respiratory Syncytial Virus (RSV) infection generally elicits mild respiratory disease in healthy adults, but is potentially lethal for infants, young children, elderly, and immunosuppressed individuals.1 In fact, RSV infection is the most common cause of virus-induced death in children under the age of 5 years worldwide.1 Although a highly effective prophylactic monoclonal antibody is available in the United States of America for at-risk infants,2 the cost of such treatment is prohibitive in most countries. Currently, there is no vaccine or therapeutic treatment for severe RSV disease.3
Although airway epithelial cells are the initial targets of RSV infection, RSV also infects lung macrophages. This results in the early release of potent proinflammatory cytokines and chemokines that recruit inflammatory cells that mediate a robust inflammatory response including cyclooxygenase (COX)-2-mediated pathology.4 This proinflammatory profile is typical of classically activated macrophages (CA-Mφ or M1).5, 6 We have previously reported that differentiation of alternatively activated macrophages (AA-Mφ or M2) occurs later in infection. These cells counteract the earlier inflammatory responses through induction of anti-inflammatory cytokines such as interleukin (IL)-10, IL-4, and IL-13, and mediate repair of lung damage through induction of enzymes such as FIZZ1, Ym1, and arginase-1.7
Arachidonic acid is a substrate for both the COX and lipoxygenase (LO) enzymes. The COX-1 and COX-2 enzymes convert arachidonic acid into prostaglandins and thromboxanes. COX-1 is ubiquitously expressed and functions in homeostatic roles, whereas COX-2 expression is highly correlated with the inflammatory process.8, 9, 10 In contrast to the COX enzymes, the LO pathway converts arachidonic acid to proinflammatory leukotrienes and anti-inflammatory lipoxins through enzymes including 5-, 12-, and 15-LO.8, 11 This pathway has been implicated in the pathogenesis or resolution of certain inflammatory diseases such as asthma and inflammatory bowel disease, respectively.12, 13 Brown et al reported that mice deficient in 5-LO exhibited persistent Lyme disease-induced arthritis.14 Although numerous cell types, including macrophages, are known to express 5-LO, 12-LO, and 15-LO, the level of expression is cell type-dependent.8, 15
In this report, we show an unexpected reciprocal relationship between induction of COX-2 and arginase-1 (and other AA-Mφ markers) in RSV-infected wild-type (WT) vs. 5-LO−/− and 15-LO−/− macrophages. This observation strongly suggested that the balance between COX-2 and LO pathways is critical to the development of pathology vs. resolution of lung injury and suggests a novel therapeutic approach for amelioration of RSV-induced disease.
Results
RSV-infected macrophages induce 5-LO and 15-LO mRNA and LO enzymatic activity
Previous studies showed that COX-2 is responsible for RSV-induced lung pathology.4 We also reported that pharmacologic inhibition of COX-2 decreased RSV-induced pathology while increasing expression of AA-Mφ genes.7 As arachidonic acid is a substrate for both COX-2 and 5-LO, and 5-LO has been shown to resolve inflammation through the release of lipoxins and resolvins,8 we sought to evaluate the possibility of a functional relationship between COX-2 and 5-LO with respect to RSV-induced lung pathology.
To determine whether RSV infection upregulates expression of 5-LO and/or 15-LO mRNA, purified mouse alveolar and peritoneal exudate macrophages were stimulated in vitro with medium only or recombinant interleukin-4 (rIL-4) (positive control for induction of AA-Mφ), or infected with RSV (Figure 1a). Although rIL-4 did not induce COX-2, RSV significantly induced COX-2 mRNA early in infection that was reduced to basal levels by 72 h in both alveolar and peritoneal macrophages. Similar to rIL-4, RSV induced expression of both 5-LO and 15-LO mRNA within several hours of infection, and both returned to baseline by 72 h (Figure 1a). Lung homogenates from RSV-infected mice showed similar results with both 5-LO and 15-LO mRNA being induced early, on day 1 post infection, and returning to and remaining at basal levels by days 4 and 6 post infection (Figure 1a). RSV failed to induce 12-LO mRNA expression either in vitro or in vivo (data not shown).
Respiratory Syncytial Virus (RSV) infection induces 5-lipoxygenase (LO) and 15-LO mRNA and lipoxygenase activity in vitro. (a) Highly purified wild-type (WT) C57BL/6J alveolar and peritoneal macrophage cultures were treated with medium only, recombinant interleukin-4 (rIL-4) (40 ng/ml), or infected with RSV (multiplicity of infection=2). WT C57BL/6J mice were mock infected with phosphate-buffered saline or infected with RSV. Lungs were collected on the days indicated. Gene expression was analyzed by quantitative real-time reverse transcription PCR. Data represent means±s.e.m. from three (macrophages) and two (whole lungs) separate experiments. (b) WT C57BL/6J and cotton rat macrophages were treated as in panel a. Lipoxygenase enzymatic activity was determined by the ferrous oxidation-xylenol orange assay. Data represent means±s.e.m. from three separate assays. (c) WT C57BL/6J mice and cotton rats were infected with RSV and lipoxygenase enzymatic activity was determined as in panel b. Data represent means±s.e.m. from two separate assays with three to six animals per treatment group in two experiments (mouse) and one experiment (cotton rat; representative of three separate experiments with similar results). *P<0.05.
The cotton rat (Sigmodon hispidus) is the model of choice for RSV infection because the lung responses more closely reflect that of humans.16 LO enzymatic activity peaked between 24 and 48 h in both mouse (Figure 1b, left panel) and cotton rat macrophages (Figure 1b, right panel) and in lung homogenates 2 days post infection in both RSV-infected mice (Figure 1c, left panel) and cotton rats (Figure 1c, right panel).
Both the 5-LO and 15-LO enzymes are required for AA-Mφ induction
No LO activity was observed in RSV-infected 5-LO−/− macrophages (data not shown). Therefore, to assess whether the 5-LO pathway is involved in the differentiation of RSV-induced AA-Mφ, WT C57BL/6 J or 5-LO−/− macrophages (on a C57BL/6 background) were stimulated with medium only or rIL-4, or infected with RSV, followed by analysis of prototype AA-Mφ markers, arginase-1 and mannose receptor mRNA, by quantitative real-time reverse transcription PCR. Both arginase-1 and mannose receptor mRNA levels were increased comparably in rIL-4-treated and RSV-infected WT macrophages, whereas RSV infection failed to induce arginase-1 mRNA in 5- or 15-LO−/− macrophages (Figure 2a). Conversely, RSV-infected 5-LO−/− and 15-LO−/− macrophages expressed greatly augmented steady-state levels of COX-2 mRNA (Figure 2a). Thus, under conditions where AA-Mφ are not induced by RSV, i.e., in the absence of 5-LO or 15-LO, a significant upregulation of COX-2 mRNA expression was observed. Similar findings were seen in vivo. Figure 2b illustrates that arginase-1 and mannose receptor mRNA expression is greatly increased in the lungs of WT, but not 5-LO−/− mice, whereas COX-2 mRNA is greatly increased in RSV-infected 5-LO−/− mice. That rIL-4 induced arginase-1, mannose receptor, and enhanced COX-2 mRNA expression in the 5/15-LO-deficient mice suggests that these enzymes act upstream of the induction of IL-4. Indeed, levels of IL-4 and IL-13 mRNA, but not levels of IL-4Rα, were decreased in the 5-LO and 15-LO macrophages (data not shown).
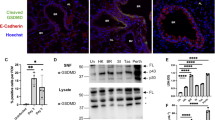
The 5-lipoxygenase (LO) pathway is required for Respiratory Syncytial Virus (RSV)-induced alternatively activated macrophages differentiation and lack of 5-LO results in increased pathology in response to RSV infection in vivo. (a) Wild-type (WT) C57BL/6J, 5-LO−/−, and 15-LO−/− peritoneal macrophages were treated as in Figure 1 and mRNA expression measured. Data are means±s.e.m. from two separate experiments. (b) WT and 5-LO−/− mice were mock or RSV infected. Mice were killed 6 days post infection, and arginase-1 and cyclooxygenase (COX)-2 mRNA measured in lungs by quantitative real-time reverse transcription PCR. (c) WT and 5-LO−/− mice were treated as in panel b. Lung pathology was scored as described in “Methods.” Results are compiled from two independent experiments *P<0.05. (d) Lung sections derived from WT and 5LO−/− mice that were RSV infected. Lungs were harvested 6 days post infection. Images were taken at × 400 magnification and the bars shown are 200 μM.
Consistent with these findings, analysis of lung sections from RSV-infected 5-LO−/− mice revealed significantly greater pathology than seen in RSV-infected WT mice (Figure 2c and d) for each histological parameter scored (i.e., peribronchiolitis, perivasculitis, interstitial pneumonitis, and alveolitis). Thus, 5/15-LO enzymes contribute to both the differentiation of AA-Mφ and to amelioration of lung pathology induced by RSV infection.
To confirm the observation that the 5-LO and/or 15-LO pathways reciprocally regulate AA-Mφ differentiation and COX-2 expression, WT macrophages were treated with 5-LO pathway inhibitor AA-861 or 15-LO pathway inhibitor, PD-146176. Blocking either 5-LO and/or 15-LO inhibited the induction of both arginase-1 and mannose receptor mRNA in both rIL-4-treated and RSV-infected WT macrophages, whereas enhancing the induction of COX-2 mRNA (Figure 3a). To challenge the hypothesis further, 5-LO−/− macrophages were treated exogenously with lipoxin A4 (LXA4), leukotriene B4 (LTB4) or leukotriene D4 (LTD4), end products of the 5-LO pathway. LXA4 has been shown to exert anti-inflammatory actions, whereas LTB4 and LTD4 have been shown to exert pro-inflammatory actions.8 Macrophages were also treated with resolvin E1 (RvE1), an endogenous lipid mediator known to be involved in the resolution of acute inflammation that is also an end product of the LO pathway, but is derived from the 5-LO substrate, eicosapentaenoic acid, rather than arachidonic acid.8, 17 Figure 3b shows that LXA4 and RvE1, but neither LTB4 nor LTD4, increased expression of arginase-1 and mannose receptor mRNA significantly in 5-LO−/− macrophages infected with RSV.
Pharmacological blockade of the lipoxygenase (LO) pathway inhibits alternatively activated macrophages differentiation. (a) Wild-type (WT) C57BL/6J peritoneal macrophages were pre-treated with AA-861 (5-LO inhibitor; 1 μg ml−1), PD-146176 (15-LO inhibitor; 1 μg ml−1), or both AA-861 and PD-146176 for 2 h. Macrophages were then treated with medium alone, recombinant interleukin-4 (rIL-4), or infected with Respiratory Syncytial Virus (RSV) for 48 h. Gene expression was measured by quantitative real-time reverse transcription PCR (qRT-PCR). (b) 5-LO−/− peritoneal macrophages were pre-treated with lipoxin A4 (LXA4; 1 μg ml−1) overnight, resolvin E1 (RvE1; 1 μg ml−1), leukotriene B4 (LTB4; 1 μg ml−1), or LTD4 (1 μg ml−1) for 1 h. Macrophages were treated with medium alone or infected with RSV for 48 h. Gene expression was measured by qRT-PCR. (c and d) WT C57BL/6J peritoneal macrophages were pre-treated with LY25583 (100 ng ml−1) or zileuton (1 μM) for 1 h. Macrophages were then treated with medium alone, LTB4 (1 μg ml−1) or LTD4 (1 μg ml−1), rIL-4 (40 ng ml−1), or infected with RSV for 48 h. Gene expression was measured by qRT-PCR. All data represent means±s.e.m. from two experiments. *P<0.05.
Although it has been previously reported that infection with RSV can lead to the production of leukotrienes,18, 19 neither study showed that these molecules contributed to the cytokine induction or inflammatory responses associated with RSV. To assess further the possible involvement of leukotrienes during RSV infection in macrophages and their role in AA-Mφ development, WT macrophages were treated with either an antagonist of the leukotriene receptors, BLT1 and BLT2 (LY255283), or an inhibitor of the cysteinyl leukotriene pathway (zileuton), and then infected with RSV. Neither inhibitor affected induction of RSV-induced arginase-1, mannose receptor, or COX-2 mRNA (Figure 3c and d, respectively), suggesting that in contrast to lipoxins and resolvins, leukotrienes do not mediate the macrophage inflammatory response induced by RSV. Together, these observations strengthen the hypothesis that the 5-LO pathway reciprocally regulates expression of COX-2 and AA-Mφ gene expression and favors the production of the anti-inflammatory lipoxins or resolvins during RSV infection.
Inhibition of COX enzymes in vitro or in vivo enhances 5-LO leading to AA-Mφ induction
Richardson et al. previously showed that RSV selectively upregulates COX-2 mRNA and protein in lung macrophages and that the pan-COX inhibitor, indomethacin, blocked RSV-induced pathology.4 To extend these findings, murine macrophages were infected with RSV in the absence or presence of indomethacin followed by the analysis of arginase-1 mRNA. RSV-induced arginase-1 mRNA was increased when indomethacin was included in the macrophage cultures (Figure 4a). In parallel, both 5-LO and 15-LO mRNA were also significantly increased during RSV infection in indomethacin-treated macrophages (Figure 4a).
Blocking cyclooxygenase (COX) activity enhances alternatively activated macrophages (AA-Mφ) and 5-lipoxygenase (LO) mRNA. (a) Wild-type (WT) C57BL/6J macrophages were treated with medium alone or infected with Respiratory Syncytial Virus (RSV; multiplicity of infection=2) in the absence or presence of indomethacin (100 nM; Indo) for 48 h. Gene expression for mRNA was measured by quantitative real-time PCR. Data represents means±s.e.m. from two experiments (*P<0.05). (b–d) WT and 5-LO−/− mice were mock or RSV infected. Starting at day 2 post infection, mice were either treated with saline or Indo (0.3 mg kg−1) for five consecutive days. Mice were killed 6 days post infection, and (b) arginase-1 and COX-2 mRNA measured in lungs by quantitative real-time reverse transcription PCR (qRT-PCR). (c) Lung pathology was scored as described in “Methods” (b, c: * is WT vs. WT comparison, P<0.05; #is 5-LO−/− vs. 5-LO−/− comparison, P<0.05; ** WT vs. 5-LO−/− comparison, P<0.05). (d) Lung sections derived from 5-LO−/− mice that were RSV infected and treated with either saline or Indo. Lungs were harvested 6 days post infection. Images were taken at × 100 magnification and the bars shown are 500 μM. (e) Cotton rats were treated daily with vehicle (saline) or parecoxib (50 mg kg−1) in 200 μl volume i.p. starting 2 days before infection for prophylactic group and starting on the day of infection (day 0) for therapeutic group. Animals were infected intranasal with RSV A/Long (1 × 106 p.f.u. per 100 μl per animal) intranasal on day 0. Treatment on day 0 was done ∼4 h post infection. Animals were killed on day 6 p.i. and 5-LO mRNA expression was analyzed by qRT-PCR. Uninfected and non-treated animals were used as controls.
When RSV-infected WT or 5-LO−/− mice were treated with indomethacin and their lungs harvested on day 6 post infection, again, indomethacin treatment increased arginase-1 mRNA in the WT lungs, but failed to upregulate arginase 1 in the 5-LO−/− mice (Figure 4b, left panel). Conversely, indomethacin treatment significantly decreased the RSV-induced COX-2 mRNA expression in both the WT and the 5-LO−/− mice (Figure 4b, right panel). This decreased COX-2 correlated with a significant decrease in RSV-induced lung pathology that was more striking in the 5-LO−/− lungs (Figure 4c and d).
Parecoxib, a COX-2-specific inhibitor, was shown previously to block COX-2 while upregulating expression of arginase-1 and mannose receptor gene expression in lungs of RSV-infected cotton rats.7 To test the hypothesis that COX-2 and 5-LO induction are reciprocally regulated in response to RSV infection, cotton rats were pretreated with saline or parecoxib, infected with RSV, then treated with saline or parecoxib after infection or paracoxib was administered after RSV infection only. Both groups of parecoxib-treated, RSV-infected cotton rats exhibited significantly increased expression of 5-LO mRNA (Figure 4e). Collectively, these data indicate that increased COX-2 inhibits both 5-LO induction and AA-Mφ differentiation, underlying increased pathology in RSV-infected mice and cotton rats.
Discussion
RSV, the most serious lower respiratory tract infection in infants and young children,1 results in up to 125,000 hospitalizations20 and ∼500 deaths yearly in the United States of America.21 RSV-specific immunity has been implicated in both protection and the immunopathological mechanism(s) that lead to severe lower respiratory tract disease and long-term changes in the immunological environment of the lung, i.e., RSV infection in early infancy has been correlated with development of allergic and asthmatic symptoms later in life.22 The idea that the immune response has an adverse role in RSV-induced disease is based largely on the outcome of a failed clinical trial in the 1960s in which vaccination of infants with formalin-inactivated RSV (FI-RSV) resulted in enhanced lower respiratory tract involvement upon subsequent RSV infection, including two deaths. Graham et al.23 first reported that formalin-inactivated RSV-induced enhanced disease was associated with a ‘Th2 type’ response. BALB/c mice immunized with formalin-inactivated RSV then challenged with RSV exhibited a pattern of cytokine mRNA expression characterized by an increased ratio of IL-4/interferon-γ and eosinophilia, whereas unvaccinated animals showed a ‘Th1 type’ response to RSV infection, with undetectable levels of IL-4.23 This led to the long-held idea that the Th2 response to RSV is pathologic.
RSV infection leads to an early ‘cytokine storm’ and production of prostaglandins.4, 24 Prostaglandins have an important role in the pathophysiology following RSV infection. There is a strong upregulation of COX-2 in bronchiolar epithelial cells and macrophages after RSV.24 COX-2 has been reported to mediate lung pathology in both RSV and influenza infections.4, 25 Later during infection, RSV-infected macrophages differentiate into the AA-Mφ phenotype that repairs the damage from inflammation.7 This is seen in both BALB/c and C57BL/6 mice with peak induction at 48 h post infection in vitro in both strains.7 Chen et al. showed that infection with influenza in mice can also lead to the development of AA-Mφ that were proposed to facilitate secondary bacterial infections such as Streptococcus pneumoniae.26 A recent study by von Moltke et al. showed macrophage-induced inflammation occurred through inflammasome-dependent production of eicosanoids, such as prostaglandins and leukotrienes, that occurred within minutes of treating cells with either anthrax lethal toxin or flagella and had pathological effects.27 Tam et al. recently showed a lipidomic profile during influenza infection in both mouse and human that supports the LO pathway for resolution of infection-induced inflammation.28 Although prostaglandins and leukotrienes are well-known as inflammatory mediators, lipoxins and resolvins require the LO pathway for their synthesis and stimulate the resolution of inflammation in multiple diseases.8 The data presented herein extend these observations by showing that RSV-infected 5-LO−/− mice fail to develop AA-Mφ and exhibit increased lung pathology because of elevated COX-2, suggesting the essentiality of the LO pathway for RSV-induced AA-Mφ and resolution of lung injury. Blocking COX-2 leads to increased 5-LO and 15-LO mRNA, as well as enhanced arginase-1 and mannose receptor mRNA.7 That RSV induces both COX-2 and LOs, and both compete for the same substrate, arachidonic acid, supports the concept of an ‘eicosanoid storm,’ as recently proposed by von Moltke et al.,27 that contributes to both the pathology by COX-2, as well as the amelioration of the initial inflammatory damage by AA-Mφ. However, if the anti-inflammatory responses are not well controlled, then this pathway may result in a predisposition to subsequent airway hyperreactivity. In fact, asthma often develops in children following severe RSV and other respiratory viral infections such as rhinovirus and influenza early in life.29 Overall, our data (i) indicate that targeting COX-2/5-LO pathways therapeutically may provide benefit in the context of severe RSV infection, and (ii) provide a novel mechanism for the control and regulation of AA-Mφ that may have broader implications in the context of other intracellular pathogens.
Methods
Virus and reagents for in vitro and in vivo studies. RSV Long strain (group A) was obtained from American Type Culture Collection (Manassas, VA), and propagated as described.4 Parecoxib was obtained from Exim-Pharm International (Mumbai, India). Indomethacin was purchased from Sigma-Aldrich (St Louis, MO). AA-861 and PD-1746, 5-LO- and 15-LO-specific inhibitors, respectively, were purchased from Biomol International (Farmingdale, NY).30, 31 LTD4, LY25583, and zileuton were purchased from Cayman Chemicals (Ann Arbor, MI).32, 33
Animals and macrophage cell cultures. Six- to eight-week-old WT C57BL/6J and Alox5−/− (5-LO−/−) mice were purchased (Jackson Laboratory, Bar Harbor, ME). Alox15−/− (15-LO−/−) mice were bred at Cincinnati Children’s Hospital. Four- to six-week-old inbred cotton rats (Sigmodon hispidus) were bred at Sigmovir Biosystems, Inc. (Rockville, MD). All animal experiments were conducted with institutional approval.
Highly purified (>97%) murine or cotton rat thioglycollate-elicited peritoneal macrophages, and murine BAL macrophages (>98%) were enriched as previously described (Shirey et al.7). Peritoneal macrophages were plated in 6-well (4 × 106 cells/well) or 12-well (2 × 106 cells per well), and BAL macrophages were plated in 24-well (2.5 × 105 cells per well) tissue culture plates. Macrophages were stimulated with medium alone, or murine or cotton rat rIL-4 (40 ng ml−1; R&D Systems, Minneapolis, MN), or infected with RSV (multiplicity of infection=2) and incubated at 37 °C for the indicated times.
For in vivo studies, WT C57BL/6J and 5-LO−/− mice and cotton rats were inoculated with sterile phosphate-buffered saline or infected with RSV (1 × 106 p.f.u. per animal) intranasal Lungs were harvested 1, 4, or 6 days later for RNA and histopathology.
Quantitative real-time reverse transcription PCR. Total RNA isolation and real-time PCR were performed as previously described.7, 34 Levels of mRNA for specific genes are reported as relative gene expression normalized to medium-treated samples. Cotton rat primers for 5-LO: forward 5′-TCAAGCAGCACAGGCGTAAAG-3′; reverse 5′-GTCCACGATGAAAATGTTCCCTTC.
Ferrous oxidation-xylenol orange assay for LO activity. LO enzymatic activity was measured using the ferrous oxidation-xylenol orange assay.35, 36 Treated macrophages were washed with cold 1 × phosphate-buffered saline two times, then lysed with 50 μl Cell Lysis Buffer (0.1% Triton X-100 containing 5 μg pepstatin, 5 μg aprotinin, and 5 μg antipain) by gentle shaking for 30 min at room temperature. The lysates were diluted 1:1 by adding 50 μl of 50 mM Tris-HCl, pH 7.4, and heated at 55 °C for 10 min and cooled for 5 min at 4 °C. Cell lysis was incubated at 4 °C for 5 min and 50 μl of cell lysate was transferred to a second 1.5-ml microcentrifuge tube where 50 μl of arachidonic acid was added to a final concentration 70 μM. The mixture was incubated at 37 °C for 10 min with a ferrous II sulfate and methanol solution to stop the reaction. Aliquot 100 μl cell lysis solution to a 96-well plate triplicate in each condition with standard curve, read at 630 nm.
Reconstitution assay. 5-LO−/− macrophages were treated with either LXA4 (1 μg ml−1; all reagents kindly provided by Christopher L Karp) overnight or LTB4 (1 μg ml−1), LTD4 (1 μg ml−1), or RvE1 (1 μg ml−1) for 1 h under a nitrogen blanket. Macrophages were then treated with medium alone or infected with RSV (multiplicity of infection=2) for 48 h before total RNA was isolated and gene expression analyzed by quantitative real-time PCR.
Inhibitor assays. For inhibition of 5-LO or 15-LO, WT C57BL/6J thioglycollate-elicited macrophages were treated with either AA-861 (1 μg ml−1) and/or PD-146176 (1 μg ml−1), 5-LO and 15-LO inhibitors, respectively, for 2 h. For inhibition of LTB4 or LTD4, WT C57BL/6J thioglycollate-elicited macrophages were treated with either LY25583 (100 ng/ml) or zileuton (1 μM) for 1 h. Macrophages were then treated with medium alone, rIL-4 (40 ng/ml), or infected with RVS (multiplicity of infection=2) for 48 h. Total RNA was isolated and gene expression for arginase-1 and COX-2 was analyzed by real-time PCR.
To assess the effect of inhibiting COX induction, WT C57BL/6J thioglycollate-elicited macrophages were treated with medium alone or infected with RVS (multiplicity of infection=2) in the presence or absence of indomethacin (100 nM) for 48 h. Total RNA was isolated and arginase-1 gene expression was analyzed by real-time PCR.
For the in vivo therapeutic treatment of mice with indomethacin, WT C57BL/6J and 5-LO−/− mice were inoculated with sterile phosphate-buffered saline or infected with RSV (1 × 106 p.f.u. per animal) intranasal Starting at day 2 post infection mice were either injected with saline or indomethacin (0.3 mg kg−1 in 100 μl) intraperitoneal (i.p.) for five consecutive days. Lungs were harvested on day 6 for RNA and histopathology.
For the prophylactic and therapeutic treatment of RSV infections with the COX-2-specific inhibitor, parecoxib, cotton rats were treated daily with vehicle (saline) or parecoxib (50 mg kg−1) in 200 μl volume i.p. starting 2 days before infection for prophylactic group and starting on the day of infection (day 0) for therapeutic group. Animals were infected with RSV A/Long (106 p.f.u. per 100 μl per animal) intranasal on day 0. Treatment on day 0 was done ∼4 h post infection. Animals were killed on day 6 p.i. and 5-LO mRNA expression was analyzed by quantitative real-time PCR. Uninfected and non-treated animals were used as a control.
Histopathology. Fixed sections (10 μm) of paraffin-embedded lungs were stained with hematoxylin and eosin. Four inflammatory parameters were scored independently from 0 to 4 for each section as previously describedPrince LI 99: peribronchiolitis (inflammatory cells, primarily lymphocytes, surrounding a bronchiole), perivasculitis (inflammatory cells, primarily lymphocytes, surrounding a blood vessel), alveolitis (inflammatory cells within alveolar spaces), and interstitial pneumonitis (increased thickness of alveolar walls associated with inflammatory cells). Slides were randomized, read blindly, and scored for each.
Statistics. Statistical differences between two groups were determined using an unpaired, two-tailed Student’s t-test with significance set at P<0.05. For comparisons between three or more groups, analysis was carried out by one-way analysis of variance, followed by Tukey’s multiple comparison test with significance determined at P<0.05.
References
Welliver, R.C. Review of epidemiology and clinical risk factors for severe respiratory syncytial virus (RSV) infection. J. Pediatr 143, S112–S117 (2003).
IMpact-RSV Study Group. Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. Pediatrics 102, 531–537 (1998).
Blanco, J.C.G., Boukhvalova, M.S., Shirey, K, Prince, G.A. & Vogel, S.N. New insights for development of a safe and protective RSV vaccine. Hum. Vaccine 6, 1–11 (2010).
Richardson, J.Y. et al. Respiratory syncytial virus (RSV) infection induces cyclooxygenase 2: a potential target for RSV therapy. J. Immunol 174, 4356–4364 (2005).
Gordon, S. Alternative activation of macrophages. Nat. Rev. Immunol. 3, 23–35 (2003).
Mosser, D.M. & Edwards, J.P. Exploring the full spectrum of macrophage activation. Nat. Rev. Immunol. 8, 958–969 (2008).
Shirey, K. et al. Control of RSV-induced lung injury by alternatively activated macrophages is IL-4Rα-. TLR4-, and IFN-β-dependent. Mucosal Immunol 3, 291–300 (2010).
Serhan, C.N. & Haeggstrom, J.Z. Lipid mediators in acute inflammation and resolution: eicosanoids, PAF, resolvins, and protectins In Fundamentals of Inflammation Serhan C.N., Ward P.A., Gilroy D.W., eds 153–174 Cambridge University Press: New York, NY, (2010).
Smith, W.L. Prostanoid biosynthesis and mechanisms of action. Am. J. Physiol. 263, F18 (1992).
Dubois, R.N. et al. Cyclooxygenase in biology and disease. FASEB J 12, 1063 (1998).
Karp, C.L. & Cooper, A.M. An oily, sustained counter-regulatory response to TB. J. Clin. Invest. 115, 1473–1476 (2005).
Wenzel, S.E. Arachidonic acid metabolites: mediators of inflammation in asthma. Pharmacotherapy 17, 3S–12S (1997).
Rask-Madsen, J, Bukhave, K, Laursen, L.S. & Lauritsen, K. 5-Lipoxygenase inhibitors for the treatment of inflammatory bowel disease. Agents Action Spec 36, C37–C46 (1992).
Blaho, V.A., Zhang, Y, Hugh-Hanks, J.M. & Brown, C.R. 5-Lipoxygenase-deficient mice infected with Borrelia burgdorferi develop persistent arthritis. J. Immunol. 186, 3076–3084 (2011).
Kuhn, H & O’Donnell, V.B. Inflammation and immune regulation by 12/15-lipoxygenases. Prog. Lipid Res 45, 334–356 (2006).
Prince, G.A., Prieels, J.P., Slaoui, M & Porter, D.D. Pulmonary lesions in primary respiratory syncytial virus infection, reinfection, and vaccine-enhanced disease in the cotton rat (Sigmodon hispidus). Lab. Invest. 79, 1385–1392 (1999).
Ohira, T. et al. Resolvin E1 receptor activation signals phosphorylation and phagocytosis. J. Biol. Chem 285, 3451–3461 (2010).
Behera, A.K., Kumar, M, Matsuse, H, Lockey, R.F. & Mohapatra, S.S. Respiratory syncytial virus induces the expression of 5-lipoxygenase and endothelin-1 in bronchial epithelial cells. Biochem. Biophys. Res. Commun 251, 704–709 (1998).
Weede-Beer, K, Hu, C, Rodriguez, M.M. & Piedimonte, G. Leukotrienes mediate inflammation in lungs of young rats infected with respiratory syncytial virus. Am. J. Physiol. Lung Cell Mol. Physiol 282, L1143–L1150 (1988).
Shay, D.K. et al. Bronchiolitis-associated hospitalizations among US children, 1980-1996. JAMA 282, 1440–1446 (1999).
Shay, D.K., Holman, R.C., Roosevelt, G.E., Clarke, M.J. & Anderson, L.J. Bronchiolitis-associated mortality and estimates of respiratory syncytial virus-associated deaths among US children, 1979-1997. J. Infect. Dis. 183, 16–22 (2001).
Sigurs, N, Bjarnason, R, Sigurbergsson, F, Kjellman, B & Bjorksten, B. Asthma and immunoglobulin E antibodies after respiratory syncytial virus bronchiolitis: a prospective cohort study with matched controls. Pediatrics 95, 500–505 (1995).
Graham, B.S. et al. Priming immunization determines T helper cytokine mRNA expression patterns in lungs of mice challenged with respiratory syncytial virus. J. Immunol 151, 2032–2040 (1993).
Radi, Z.A., Meyerholz, D.K. & Ackermann, M.R. Pulmonary cyclooxygenase-1 (COX-1) and COX-2 cellular expression and distribution after respiratory syncytial virus and parainfluenza virus infection. Viral Immunol 23, 43–48 (2010).
Carey, M.A. et al. Contrasting effects of cyclooxygenase-1 (COX-1) and COX-2 deficiency on the host response to influenza A viral infection. J. Immunol 175, 6878–6884 (2005).
Chen, W.H. et al. Potential role for alternatively activated macrophages in the secondary bacterial infection during recovery from influenza. Immunol. Lett 141, 227–234 (2012).
von Moltke, J. et al. Rapid induction of inflammatory lipid mediators by the inflammasome in vivo. Nature 490, 107–111 (2012).
Tam, V.C. et al. Lipidomic profiling of influenza infection identifies mediators that induce and resolve inflammation. Cell 154, 213–227 (2013).
Dulek, D.E. & Peebles, R.S. Jr Viruses and asthma. Biochim. Biophys. Acta 1810, 1080–1090 (2011).
Du, L. et al. Binding investigation of human 5-lipoxygenase with its inhibitors by SPR technology correlating with molecular docking simulation. J. Biochem 139, 715–723 (2006).
Sordillo, L.M. et al. Enhanced 15-HPETE production during oxidant stress induces apoptosis on endothelial cells. Prostaglandins Other Lipid Mediat 76, 19–34 (2005).
Yokomizo, T, Kato, K, Hagiya, H, Izumi, T & Shimizu, T. Hydroxyeicosanoids bind to and activate the low affinity leukotriene B4 receptor, BLT2. J. Biol. Chem. 276, 12454–12459 (2001).
Carter, G.W. et al. 5-lipoxygenase inhibitory activity of zileuton. J. Pharmacol. Exp. Ther 256, 929–937 (1991).
Shirey, K, Cole, L.E., Keegan, A.D. & Vogel, S.N. Francisella tularensis LVS induces macrophage alternative activation as a survival mechanism. J. Immunol. 181, 4159–4167 (2008).
Waslidge, N.B. & Hayes, D.J. A colorimetric method for the determination of lipoxygenase activity suitable for use in a high throughput assay format. Anal. Biochem 231, 354–358 (1995).
Cho, Y.S., Kim, H.S., Kim, C.H. & Cheon, H.G. Application of the ferrous oxidation-xylenol orange assay for screening of 5-lipoxygenaes inhibitors. Anal. Biochem. 351, 62–68 (2006).
Acknowledgements
This study was supported by NIH grants AI-057575 (J.C.G.B.) and AI-18797 (S.N.V.) and Cystic Fibrosis Foundation RDP Center Grant (C.L.K.).
Author contributions
K.A.S. and S.N.V. carried out the study design, with advice from J.C.G.B. and C.L.K. K.A.S., W.L., J.C.G.B., and L.M.P. performed experiments. C.L.K. and S.D. provided crucial reagents for the study. K.A.S. and S.N.V. prepared the manuscript, with input and approval of all other co-authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declared no conflict of interest.
Rights and permissions
About this article
Cite this article
Shirey, K., Lai, W., Pletneva, L. et al. Role of the lipoxygenase pathway in RSV-induced alternatively activated macrophages leading to resolution of lung pathology. Mucosal Immunol 7, 549–557 (2014). https://doi.org/10.1038/mi.2013.71
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mi.2013.71
This article is cited by
-
A metabolic associated fatty liver disease risk variant in MBOAT7 regulates toll like receptor induced outcomes
Nature Communications (2022)
-
Mild COVID-19 imprints a long-term inflammatory eicosanoid- and chemokine memory in monocyte-derived macrophages
Mucosal Immunology (2022)
-
Role of specialized pro-resolving lipid mediators and their receptors in virus infection: a promising therapeutic strategy for SARS-CoV-2 cytokine storm
Archives of Pharmacal Research (2021)
-
Immune recovery following bronchiolitis is linked to a drop in cytokine and LTC4 levels
Pediatric Research (2020)
-
Specialized pro-resolving mediators: endogenous regulators of infection and inflammation
Nature Reviews Immunology (2016)