Abstract
Conventional approaches to the diagnosis of infectious diarrhea must include several modalities to detect an array of potential viruses, bacteria, and parasites. We will provide a general overview of the wide range of diagnostic modalities available for enteropathogens, briefly discuss some of the limitations of conventional methods, and then focus on new molecular methods, including real-time PCR and next-generation sequencing. In particular, we will discuss quantitation of pathogen load with these techniques. We will then describe examples whereby novel diagnostics may help illuminate the etiology of infectious diarrhea, where they may not, and how they may benefit studies of immunity to enteric infections.
Similar content being viewed by others
Introduction
Infectious diarrhea remains an enormous global health problem and a leading cause of death in children <5 years of age.1 Infections with many diarrhea-associated pathogens have also been associated with substantial additional morbidity in the form of intestinal barrier dysfunction, malnutrition, and cognitive impairment.2 Traditionally, enteric infection is conceptualized as a binary state—the pathogen is either present in the gut or it is not. The goal of this review is an understanding of the broad range of diagnostics available for enteropathogen infections associated with diarrhea and how molecular diagnostics might help provide a more nuanced picture of infection and immunity. For example, studies of children in developing countries suggest frequent asymptomatic low-level infection as well as mixed infection. We expect that quantitative diagnostics will be helpful in interpreting this complex picture.
Conventional Approaches to Detecting Enteropathogens
A wide range of etiological agents have been associated with infectious diarrhea, including viruses, bacteria, and parasites.3 Diagnostically, a patchwork of modalities is available, including culture, microscopy, and antigen-based tests. Each combination of pathogen and test has distinct performance characteristics, and there are limitations to all available modalities. Culture methods are often low yield for enteropathogens, particularly in the setting of antibiotic use.4 Microscopy for parasites is widely used because it is inexpensive, but it is insensitive and requires substantial time, equipment, and training. Antigen-based tests have represented a substantial advance for diarrheal diagnostics; however, the test characteristics are variable, and commercial assays are not available for all relevant pathogens.5, 6 Molecular tests will be detailed below. In the context of epidemiological studies of diarrhea as well as syndromic testing, standardization of a work-flow involving this wide range of modalities is challenging.7
Culture-Based Diagnostics: the Example of Campylobacter Species
Bacterial stool culture is an integral part of the standard microbiological work-up of a clinical sample but is limited by a low yield.8 Techniques that improve the yield can limit the isolation of potentially important pathogens. For example, Campylobacter species are difficult to isolate in the presence of normal stool flora, thus selective techniques are commonly employed. Such techniques, in particular the use of antibiotic-containing selective media, proved critical for an understanding of the epidemiology of Campylobacter jejuni, the species most commonly implicated in human disease.9 In addition to the use of antibiotic-containing media, selective techniques for the growth of Campylobacter species take advantage of their evolution in avian hosts by modifying the thermal and atmospheric conditions.10 Although these selective techniques have clearly improved the isolation of C. jejuni and Campylobacter coli, they have limited detection of other Campylobacter species. Alternative strategies, including filtration techniques, have led to the characterization of additional emerging Campylobacter species whose clinical relevance is beginning to be understood, most clearly for Campylobacter upsaliensis.11, 12, 13 In Cape Town, South Africa, using less selective culture techniques, C. jejuni isolates represent only about 40% of all Campylobacter isolates from children with diarrhea.14 Molecular approaches, including the use of 16S ribosomal RNA (rRNA) sequencing, suggest that an even broader range of Campylobacter species can be isolated from human stool samples but that relatively few of them have been demonstrated to be pathogenic.12, 15 The example of Campylobacter emphasizes that diagnostic techniques are not agnostic. They represent the cumulative experience of microbiology laboratories and potential associated biases, which can hinder the ability of broad diagnostic work-ups to provide a level playing field.7
Antigen-Based Diagnostics
Antigen-based testing represents a substantial advance for diarrheal diagnostics, in particular for viral and protozoal pathogens. For example, enzyme immunoassay (EIA)-based detection was universally used for case ascertainment in rotavirus vaccine clinical trials.16, 17, 18, 19 However, there is some evidence that these tests are insensitive in comparison to a PCR gold standard. One comparison of PCR and EIA-based detection of rotavirus on clinical samples suggested a sensitivity of roughly 50%.20 Norovirus immunoassays have historically demonstrated poor sensitivity when used on clinical specimens.21 During the 2011 outbreak of Shiga toxin-producing Escherichia coli (STEC) in Germany, EIA sensitivity was 76.8% compared with a culture gold standard.22 Specificity can also be unacceptably low with EIA tests, especially in low-prevalence settings. For example, this has prompted a transition to PCR-based testing for Clostridium difficile infection.23 All of these tests are reported as positive or negative based on an optical density cutoff, typically representing the mean optical density of negative samples plus three standard deviations. Above the cutoff, the optical density value is thought to be a semi-quantitative measure of antigen level.
Serological Diagnostics and Biomarkers
Serological diagnostics are used extensively in infectious diseases, typically for pathogens that are difficult to isolate directly. Due to the need to test both acute and convalescent sera, the practicality of serological diagnostics for acute infectious diarrhea is limited. Additionally, the accuracy of any serological test is dependent on the specificity of capture antigen (e.g., crude extracts vs. specific proteins), the titer of antibodies for that antigen in serum, and the detection modality used (e.g., EIA vs. Western blot). That said, serological tests may have value for epidemiological studies. In studies of pneumonia etiology, serological studies frequently are more sensitive than direct sample testing, in particular for viral etiologies.24 In epidemiological studies of the relationship between infection with enteric pathogens and long-term outcomes, longitudinal serological measurements could provide a more comprehensive view of exposure to enteric pathogens by identifying exposures missed by intermittent stool sampling. Steinberg et al.25 measured immunoglobulin G antibodies by an enzyme-linked immunoassay to characterize exposure to waterborne pathogens enterotoxigenic E. coli, norovirus and Cryptosporidium parvum in children in rural Guatemala. They demonstrated a high seroprevalence of antibodies to each pathogen by 3 years of age, suggesting that this is a sensitive marker of exposure. Priest et al.26 have developed a multiplex bead assay for Cryptosporidium and Giardia intestinalis. It is likely that such tests will be available for a broader range of pathogens in the near future. Such tests may improve our understanding of the association between early exposure to specific enteropathogens and long-term outcomes such as malnutrition and poor vaccine response.
Mass Spectrometry–Based Diagnostics
Another promising avenue for clinical microbiology is the development of mass spectrometry–based identification of pathogens, which broadly fall into two categories. The first is matrix-assisted laser desorption ionization time-of-flight mass spectrometry–based systems for rapid pathogen identification directly from colonies. Such systems offer species-level identification of organisms in less than an hour. This is particularly appealing for blood culture, where detection can be performed directly on positive blood culture broths.27 For the detection of pathogens from stool, this method is still limited by the need for successful isolation of the pathogen. The second, PCR-electrospray ionization mass spectrometry, identifies the nucleic acid composition of multiple PCR-amplified, broadly conserved regions of bacterial, viral, or fungal genomes, which is then compared with a composition database for a wide variety of organisms. Such an approach has been used recently for identification of influenza and funga pathogens from respiratory specimens as well as direct detection of bacterial and fungal pathogens from heart valve tissue.28, 29, 30
Molecular Diagnostics
Molecular diagnostics have an emerging role in the diagnosis of infectious diseases. These tests generally involve the amplification of DNA or RNA. US FDA (Food and Drug Administration)-approved nucleic acid amplification tests now exist for a number of bacterial, mycobacterial, and viral infections. These molecular tests have consistently demonstrated excellent sensitivity when compared with traditional diagnostics. There is a great promise for molecular diagnostics for diarrhea in particular, where enhanced sensitivity is desirable and diagnostic yield is typically poor. Recently, the first PCR-based multiplex panel for etiologies of gastroenteritis was approved by the FDA, which can detect Campylobacter, C. difficile, E. coli 0157, enterotoxigenic E. coli, Salmonella, Shigella, STEC, norovirus, rotavirus, Cryptosporidium, and Giardia.31
The first critical step for any molecular-based test is the extraction of nucleic acid from the sample. Stool is a complex mixture rich in background nucleic acid and amplification inhibitors. The detection of a known amount of nucleic acid is often several logs reduced when placed in a stool mixture. There is some evidence that magnetic bead-based extraction systems yield less inhibitors than column-based systems.32, 33 Inclusion of an extrinsic control before extraction can identify false-negative results and allow for an estimation of the combined extraction and amplification efficiency.34
PCR is, by far, the most common technique for nucleic acid amplification. Molecular targets have been reported for the majority of known enteropathogens.35 The sensitivity of PCR has started to change our understanding of diarrheal disease. For instance, in a study of 127 fecal samples from patients with symptoms of acute gastroenteritis, 18 were culture positive for Campylobacter, whereas 58 were PCR positive.36 An investigation of real-time PCR detection of microsporidia demonstrated a lower limit of detection of 102 spores per ml stool compared with 106 spores per ml for microscopy.37 Amar et al.38 employed PCR to re-examine the English case-control Infectious Intestinal Disease Study. This increased the enteropathogen detection rate from 53% to 75% of cases as well as from 19% to 42% of controls. The detection rate increased for both viral and bacterial enteropathogens and, not surprisingly, the number of samples with multiple pathogens detected increased. Although the potential for increased diagnostic yield is substantial, the clinical significance of isolated PCR findings can become less clear.
Multiplex and Arrayed Singleplex PCR
The wide variety of potential pathogens mandates the ability to efficiently amplify multiple targets. This can be accomplished using either multiplex or arrayed singleplex PCR. The former allows for the detection of multiple targets in a single reaction. Discrimination requires target-specific probes, determination of the relative size or composition of the DNA amplicons by gel analysis, or analysis of the melting characteristics of amplicons.39, 40, 41, 42 Our group has used multiplex PCR reactions with detection using Luminex beads as a means to increase multiplex testing.43, 44 The future will see more multi-target amplification tests to offer syndromic testing for agents that currently require multiple testing modalities. These will include multiplex and arrayed singleplex systems, which have been recently employed to determine the etiology of respiratory infections.45, 46 Several multiplex panels for enteropathogens, including a broad enteropathogen panel and a STEC serotyping assay, have been developed.31, 47 Arrayed singleplex PCR is not limited by the available range of fluorescent dyes for differential detection in a multiplex reaction. It may also offer improved sensitivity and quantitation by avoiding competition for the available nucleic acid substrate between targets in a single reaction. Our group has developed a TaqMan Array Card-based assay for the detection of 19 diarrhea-causing enteropathogens.48
Quantitative PCR
Molecular strategies, though highly sensitive, may result in the detection of low levels of enteropathogens of unclear clinical significance, particularly in developing countries where certain enteropathogens such as Giardia, E. coli, Campylobacter, and many viruses are widespread.49 Ultimately, approaches that can offer quantitative detection may prove useful to infer clinical significance. “Real-time” PCR is a method whereby fluorescent probes emit a signal proportional to the amount of synthesized nucleic acid. The number of cycles at which the fluorescence exceeds a defined background level (quantification cycle (Cq)) is thus a proxy for nucleic acid quantity. Alternatively, mechanistic models have recently been developed that may improve quantitation by minimizing the influences of baseline adjustment errors, varying reaction efficiencies, and low initial template concentrations.50, 51 Further refinements to quantitation include use of standard curves of known quantities of targets, and use of spiked controls that control for sample-to-sample variability in nucleic acid extraction and amplification efficiency. Because stool is an inhibitory matrix, it is likely that absolute quantitation has limitations not present in other milieus, such as plasma. For example, a spiked control can be used as a marker of amplification efficiency, but inhibitors present in stool may inhibit some targets and not others, and it is possible that normalization with a spiked control will introduce bias.52 For a given target, the correlation between extrinsic control and target inhibition is likely dependent on the target concentration. For example, coliphage MS2 RNA has been used as a non-competitive control for the detection of RNA viruses in stool. Shulman et al.33 found that the correlation between MS2 and enteroviral reverse-transcription PCR inhibition increased inversely in relation to the amount of enteroviral RNA in the sample. This could lead to over-adjustment of high-level detection of the molecular target. Thus, it might be prudent to choose an extrinsic control detection cutoff Cq, above which quantification is not possible, rather than performing a log-linear normalization of the target quantity using the extrinsic control. Several groups have suggested that viral PCR results in the setting of MS2 inhibition of more than three Cq should not be quantified for clinical purposes.33, 53 Alternatively, competitive internal controls that share primer sequences with the target of interest are more likely to be inhibited to a similar extent but may have a substantial effect on assay sensitivity and are unwieldy for assays with multiple targets.54, 55
Choice of Pathogen-Specific Molecular Targets
Molecular diagnostics offer the possibility of homogenizing the test characteristics of a broad array of pathogens; however, the appropriate selection of molecular targets is critical. The ideal target would be a well-conserved gene with a known number of copies, but the identification of such a target is not always possible. Uncertainty in the target copy number, in particular for ribosomal RNA and plasmid-borne targets, may impair the accuracy of quantitation. In some cases, targets are virulence factors, which may be the only clear targets to distinguish pathogenic strains. For example, the emergence of pathogenic E. coli species likely represented the acquisition of virulence factors by previously commensal organisms.56 Various virulence factors have been described but are variably present in enteroaggregative E. coli (EAEC) isolates, and no single factor is a clear prerequisite for pathogenicity.57 Boisen et al.58 utilized genome hybridization to identify potential virulence factors among EAEC strains isolated from a case-control study of moderate-to-severe diarrhea in Mali. Neither of the molecular targets used to identify EAEC isolates, aatA and aaiC, were detected significantly more frequently in diarrheal samples. The virulence gene most strongly associated with diarrhea, sepA, was found in one-third of EAEC diarrheal isolates. However, it is likely that this gene is sufficient but not necessary to cause disease. In this context, the epidemiology of EAEC is dependent on the molecular targets chosen and is clearly dynamic, as we would expect new virulence factors to be more pathogenic when they emerge in a population. It is possible that quantitation will help here, in that the detected quantity of conserved genes may be higher when EAEC is the causative pathogen, but this has not been investigated.
Preferential Detection of Viable Pathogens
A limitation to all currently available non-culture-based diarrheal diagnostics is the inability to distinguish between viable and nonviable pathogens. Although successful isolation of a pathogen in culture is a clear marker of viability, alternate markers include evidence of metabolic activity, active RNA transcription, or intact membranes. Detection of mRNA suggests active replication, but degradation can occur due to freeze–thaw cycles or contamination with RNA-degrading enzymes. The amount of non-genomic RNA is widely variable, which hinders the interpretation of quantitative PCR results.59, 60 Alternatively, differential amplification of viable organisms can be achieved by introducing membrane-impermeant nucleic acid intercalating dyes before DNA extraction to suppress detection of DNA from cells that lack intact membranes. However, concerns persist about the sensitivity and specificity of this approach.61 We would argue that the quantity of genomic DNA or RNA is a more useful and consistent surrogate for viability, though this relies upon the assumption that viable, disease-associated pathogens should be present in a higher quantity. In settings where exposure to enteropathogens is common and multiple pathogens are frequently isolated from both symptomatic and asymptomatic specimens, quantitation may not be sufficient to implicate one pathogen over another, but the clinical data available to understand this question are very limited.
Next-Generation Sequencing
Next-generation sequencing (NGS) is characterized by the ability to rapidly and deeply sequence mixed populations of DNA or RNA genomes and has already had a substantial impact on our understanding of the epidemiology of many diarrhea-associated bacterial pathogens. Recently, whole-genome sequencing and phylogenetic analysis was used to examine the origin of the Haitian cholera outbreak.62 A similar approach suggested that two independent epidemic lineages with distinct patterns of global spread of the C. difficile 027/BI/NAP1 strain emerged almost simultaneously from North America.63 During the European outbreak of hemolytic-uremic syndrome in 2011, Mellmann et al.64 compared the complete genome sequence of an outbreak isolate with a previously-sequenced isolate as well as banked sequences of core E. coli genes. This phylogenetic analysis suggested that horizontal gene exchanged facilitated the emergency of a novel, highly virulent strain of STEC. Bielaszewska et al.65 utilized the molecular analysis of an early isolate to develop a multiplex PCR specific to the strain, which was then used for characterization of additional isolates. NGS has also been shown to be an effective approach for the identification of novel pathogens and has been used to identify several putative diarrheal pathogens.66, 67, 68, 69, 70 These findings have yet to be validated in clearly phenotyped diarrheal cases and controls, but large archives of clinical stools from multisite studies of diarrhea now exist and afford an excellent opportunity to explore this further.71 Broad molecular testing for known causes of diarrhea can pre-screen diarrheal samples and increase the efficiency of such an approach.
Ultimately, it is possible that probe-based detection will be replaced by sequencing for the detection of known pathogens as well.72, 73 This represents an even more agnostic approach, in that results will no longer be dependent on the selection of a solitary or, at best, a small number of molecular targets. 16S rRNA-based phylogenies do not provide sufficient resolution for identifying all bacterial species. Instead, multilocus sequence typing may be needed to provide a universal approach to species-level identification, but the selection of appropriate loci can be cumbersome. For example, identification of emerging Campylobacter species requires the analysis of different sets of loci depending on the species of interest.74 Alternatively, multilocus sequence typing based on ribosomal proteins can provide significantly more resolution than phylogenies based on 16S rRNA while still offering a universal set of loci for identification of all bacteria down to the level of an individual strain.75, 76 Similar approaches should be possible for other classes of pathogens.76
There is some evidence that specific diarrheal pathogens can cause characteristic changes in the composition and diversity of normal flora. This has been shown for rotavirus, where changes in Bacteroides species composition can distinguish rotavirus-infected subjects from healthy controls.77 Nelson et al.78 showed that a subset of children with norovirus-associated diarrhea had significantly altered microbiota characterized by a reduction in Bacteriodetes and an increase in Proteobacteria. A reduction in the diversity of the microbiota has been associated with an increased risk for recurrent C. difficile disease in mice and humans, and the restoration of diversity using targeted bacteriotherapy or stool transplant is profoundly effective in reducing this risk.79, 80, 81 Although it may be unlikely that a microbiotic footprint can be identified that is sufficiently sensitive or specific to be used diagnostically, measurements of diversity or the absence of certain “keystone” species might predict disease severity as well as the risk of long-term sequelae, such as malnutrition, altered gut function, and impaired mucosal immunity.
Molecular Diagnostics for Antibiotic Susceptibility Testing
Phenotypic antibiotic susceptibility testing relies on the assessment of in vitro growth in the presence of antibiotics. Molecular diagnostics, on the other hand, interrogate for known genetic markers of resistance. Resistance to many bacterial pathogens, including Shigella, Salmonella, and Campylobacter, is increasing.82 Detection of resistance markers in stool DNA extracts is challenging, because the multiplicity of organisms in stool hinders the attribution of detection of a resistance marker to a particular pathogen. However, these methods can be used on pure cultures, for example, identification of fluoroquinolone-resistant strains of E. coli and Shigella spp. via detection of gyrA and parC mutations.83 NGS may improve the virtual detection of antimicrobial resistance but will still rely upon validated correlations between specific mutations and phenotypic resistance.72 The potential for rapid identification of resistance with these approaches is more likely to complement, rather than replace, phenotypic testing. Another potential consequence of the change to non-culture diagnostic tests for infectious diarrhea is that fewer clinical isolates will be available for testing by public health laboratories to assist in outbreak detection.84 Indeed, in both cases, it is unclear how clinical laboratories will be reimbursed for continuing to culture isolates after transitioning to a new test. That said, molecular screening has been shown to substantially improve the efficiency and sensitivity of pathogen detection by guiding the conventional microbiological work-up.85
Utility of Quantitative Diagnostics for Studies of Diarrhea and Mucosal Immunology
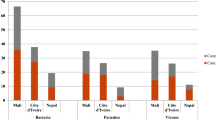
Traditionally, a host has been characterized as susceptible or resistant based on the presence or absence of detectable pathogen. However, it is becoming clear that a more nuanced understanding of pathogenesis is required, which conceives of pathogenicity as an emergent property of the dynamic interaction between host and pathogen.86 This requires a reconsideration of the basic concepts of colonization, infection, and disease.87 Casadevall and Pirofski88 have proposed a classification system for describing the relative contribution of host- and pathogen-mediated damage in disease pathogenesis. These dynamics may have implications for the relevance of pathogen quantitation. For example, if disease pathogenesis is primarily mediated by the pathogen, we might expect pathogen quantity to correlate with disease severity, although host factors may attenuate this association. If disease is primarily host mediated, the relationship between pathogen quantity and disease may be less clear (Figure 1). Therefore the association between quantity and disease will likely be host and pathogen specific. Fredericks and Relman89 have proposed a revision of Koch’s postulates for molecular diagnostics, whereby the presence of nucleic acid belonging to a putative pathogen should vary not only quantitatively but also temporally with the clinical manifestations of the disease. That is, more pathogen should be detected during the disease state at the time and location of pathology.
Relationship between pathogen load, disease pathogenesis, and disease severity. Pathogen quantity may be more clearly associated with disease for pathogen-mediated rather than host-mediated disease pathogenesis.
There are numerous examples where the quantity of pathogen in biological samples can be used to differentiate between contamination, colonization, and infection. Threshold colony counts are used to reduce false-positive urine cultures due to contamination.90 Fujisawa et al.91 showed that a real-time PCR quantitative threshold, validated against a clinical gold standard, was superior to conventional PCR for the diagnosis of Pneumocystis pneumonia in HIV-negative immunocompromised patients. In the gut, fecal egg counts have been used as markers of burden and have demonstrated clinical endpoints for anti-helminthic therapy and helminth vaccine trials.92, 93, 94, 95, 96 Several studies have examined the value of quantitative molecular diagnostics for diarrheal pathogens. Kang et al.97 demonstrated a significant correlation between rotavirus PCR Cq and disease severity in children with acute gastroenteritis. Similarly, norovirus stool viral load may help distinguish between incidental low-level carriage and higher-burden, norovirus-associated disease.98 PCR is likely to continue to detect diarrhea-associated pathogens for extended periods after disease resolves; however, the peak viral loads should associate temporally with disease. Serial samples from subjects experimentally challenged with norovirus were assayed by both EIA and PCR to determine the duration of shedding.99 EIA detected virus shedding for a median of 7 days, whereas PCR continue to detect virus for a median of 28 days. In the majority of subjects, the stool viral load peaked 1–2 days after resolution of symptoms. The stool viral load fell by 2–3 orders of magnitude by 1 week, which corresponds to a change of roughly 6–10 Cq units. The interesting observation that norovirus stool viral load frequently peaked after resolution of diarrhea could be a consequence of the dilutional effect of water present in diarrheal samples. Thus, a diarrheal stool may under detect the true quantity of a pathogen in the gut. For studies of diarrhea etiology, this could lead to a failure to detect a real difference in pathogen quantity between diarrheal and control specimens. It is also possible that dilution of inhibitors will increase the amplification efficiency in liquid stools, leading to over detection. Normalization with an extrinsic control can potentially correct for these factors. In any case, we would expect that either of these effects will be relatively small, given that the relative difference in pathogen quantity between samples can be more than a million fold. To date, it is perhaps not surprising that the value of quantitation has been demonstrated most clearly for viral pathogens given the central role of replication in viral pathogenesis.100 There is some evidence that the utility will extend to bacterial pathogens as well. Barletta et al.101 compared the quantity of the intimin gene (eaeA) of enteropathogenic E. coli isolated from healthy and diarrheal stools from Peru. They showed that the amount of eaeA DNA was higher in diarrheal samples, as well as among samples for which enteropathogenic E. coli was the only pathogen isolated.
We expect that additional evidence of the relationship between quantitation and virulence will emerge, but it is quite possible that this relationship does not exist for some diarrheal pathogens or that such a relationship is dynamic. Clearly, molecular tests will lead to a substantial increase in detection of uncertain significance. If the quantity of pathogen detected is strongly correlated with the presence of disease, quantitation may be helpful to empirically derive the cutoff detection quantity that is associated with disease (Figure 2). For example, community-matched controls in case-control studies are usually required to be diarrhea free for some period of time.102 The time frame is important, because a PCR test for many pathogens (including norovirus) would still be positive at that time, and thus detection in controls will increase. However, a quantitative comparison between cases and controls would show a significant association of high-level detection with disease (Figure 3). This may substantially improve the power of such studies for detecting a real association of less common pathogens with diarrhea. More study is needed to determine whether persistent post-disease and asymptomatic carriage of the wide range of diarrhea-associated pathogens can be differentiated based on quantity.
Hypothetical range of detection of different diagnostic modalities. Here, only quantitative PCR detects all infections above the threshold quantity associated with clinical disease. When appropriate, quantitative PCR results can be “detuned” to an empirically derived clinical threshold to avoid detection of clinically irrelevant levels of pathogen.
A hypothetical child infected over time with four enteropathogens. Periods of diarrhea are shown in grey. Mixed infection as well as asymptomatic infection is seen. Although each causative pathogen will still be detected in asymptomatic stools, the burden will be markedly lower. Controlling for age is clearly critical for inferring disease association from pathogen quantity.
Similar principles can be applied to studies of mucosal immunology. Although in mouse models, it is often possible to give direct estimates of pathogen quantity,103, 104, 105, 106 studies in humans have often been limited to binary detection of pathogen. A classic example is the increased risk for cholera and norovirus in individuals with blood group O.107, 108, 109 Below, we consider how molecular diagnostics might add to our understanding of the mucosal immunology of three specific diarrheal pathogens.
Case study 1: Rotavirus
Rotavirus vaccine efficacy has been consistently found to be lower in low socioeconomic settings.16, 18, 110 Though the basis for this reduced efficacy is unclear, it is consistent with the reduced efficacy of other oral vaccines (e.g., polio, typhoid, and cholera) in these settings. Possible reasons for this phenomenon include malnutrition, competing intestinal infection, interference by maternal antibodies, and tropical enteropathy. Concomitant helminth and viral infections appear to attenuate the immune response to vaccine challenge.111, 112 Tropical enteropathy, in part mediated by early and persistent exposure to enteropathogens, may be triggered by persistent enteropathogen exposure early in life.113 Molecular diagnostics may be helpful for our understanding of rotavirus vaccine efficacy in several ways. First, they might provide better estimates of exposure to other enteropathogens both before and at the time of immunization. Second, they can determine whether immunization is associated with complete “sterilizing” immunity or low-level, asymptomatic carriage, which has implications for disease transmission. Finally, they may alter estimates of disease burden. As discussed previously, most vaccine trials use EIA for case ascertainment and do not look for other etiologies of diarrhea. If low-level rotavirus is detected during episodes of diarrhea due to another pathogen, this theoretically could lead to overestimation of rotavirus-associated diarrhea. Braeckman et al.114 used PCR-based detection of adenovirus, astrovirus, and norovirus to show that efficacy is not impaired by co-infection with other viruses, which suggests that rotavirus was still the primary etiology in these cases. However, such a study has not been performed in a setting of reduced rotavirus efficacy and high endemicity for other enteropathogens. A re-analysis of archived stools from a rotavirus vaccination trial with a broad molecular diagnostic panel could help explore this further.
Case study 2: Cryptosporidium
Cryptosporidium is a protozoa first described in humans in 1976 from electron microscopy studies of stool from an immunocompromised patient with severe diarrhea.115 Human infection is now known to span several species, predominantly C. hominis in most studies. Human volunteer challenge studies in the 1990s established the pathogenicity of C. parvum, describing a dose-dependent association between exposure and infection, as well as a strong correlation between oocyst excretion and disease.93, 116 Disease in AIDS patients has also been associated with increased oocyst loads.117 The mechanisms of protective immunity to Cryptosporidium are uncertain. Certainly, CD4+ T cells are important in control as evidenced by the increased severity of disease in patients with advanced HIV; however, many patients with advanced HIV are asymptomatically infected, suggesting other mechanisms of protection.118 Interferon gamma and intraepithelial lymphocytes are of major importance in mouse models.119, 120 The role of antibody is even less clear. Bovine anti-cryptosporidium oocyst immunoglobulin can partly prevent or limit disease in calves,121 but the evidence for a benefit in AIDS patients is limited.122 High titers of serum antibodies to Cryptosporidium are seen in patients with HIV but are a marker of exposure and not clearly associated with protection.123 Cryptosporidium is now frequently detected using one of the several commercially available EIAs. There is some evidence that individual Cryptosporidium species as well as C. hominis subtypes induce different clinical manifestations, in which case detection of molecular subtypes will be important for understanding the immune response.124 Given the nuances associated with immunity to this organism, it is also likely that a quantitative assay would be a useful adjunct in studies of disease pathogenesis and mechanisms of protection, as well as for vaccine development.
Case study 3: C. difficile
Testing for C. difficile is now largely performed with EIA or PCR specific for toxin. A comparison of nine commercially available EIAs yielded an average sensitivity and specificity of 82.8% and 95.4%, respectively, compared with a stool culture gold standard.125 The test characteristics also appear to vary significantly by C. difficile strain type.126 Recently, PCR-based tests on stool targeting the toxin B gene have been adopted by some institutions, for use either as a stand-alone test or as confirmation after a high-sensitivity screening test. These tests are highly sensitive and specific;127 however, clinical suspicion remains an important part of the testing algorithm. Due to the increased sensitivity, the additional cases detected by PCR alone may be lower burden than those also detected by EIA. Longtin et al.128 found that cases detected by PCR alone in the setting of a surveillance program were much less likely to develop a complication, including death, intensive care unit admission, and hospital readmission. Traditionally, the pathogenesis of C. difficile–associated disease is described as a state of pathogen overgrowth and an associated increase in toxin production. In this model, the quantity of nucleic acid might help distinguish colonization from disease and provide a marker of disease severity. A non-PCR method of toxin quantitation showed a correlation between toxin concentration and disease severity, but studies of PCR-based quantitation and clinical outcomes have not been performed to our knowledge.129 It is possible that reverse-transcription PCR will be the best approach for quantitating toxin production.130 Adaptive immunity, in particular production of serum antibodies against toxin A and B, is protective against C. difficile–associated disease. This has been demonstrated by the benefit of both intravenous gamma globulin and monoclonal anti-toxin antibodies.131, 132 Quantitative diagnostics could assess the association between antibody levels and pathogen load as well as the association between load, clinical severity, and risk of disease complications.
Concluding Remarks
The advent of molecular diagnostics is bringing new insights into etiologies of infectious diarrhea. Features to be better understood include the importance of mixed infections and the role of quantitative diagnostics in studies of diarrheal disease. We expect these diagnostics to refine our understanding of the epidemiology of diarrheal disease and be of particular benefit for case ascertainment during vaccine efficacy trials. Studies of mucosal immunology should follow closely behind, offering a more nuanced and accurate picture of the pathogenesis of infectious diarrhea.
References
Walker, C.L., Aryee, M.J., Boschi-Pinto, C. & Black, R.E. Estimating diarrhea mortality among young children in low and middle income countries. PLoS One 7, e29151 (2012).
Guerrant, R.L., Oria, R.B., Moore, S.R., Oria, M.O.B. & Lima, A.A.M. Malnutrition as an enteric infectious disease with long-term effects on child development. Nutr. Rev. 66, 487–505 (2008).
Fischer Walker, C.L., Sack, D. & Black, R.E. Etiology of diarrhea in older children, adolescents and adults: a systematic review. PLoS Negl. Trop. Dis. 4, e768 (2010).
Guerrant, R.L. et al. Practice guidelines for the management of infectious diarrhea. Clin. Infect. Dis. 32, 331–351 (2001).
Haque, R., Neville, L.M., Hahn, P. & Petri, W.A. Jr. Rapid diagnosis of Entamoeba infection by using Entamoeba and Entamoeba histolytica stool antigen detection kits. J. Clin. Microbiol. 33, 2558–2561 (1995).
Kirby, A. et al. An evaluation of the RIDASCREEN and IDEIA enzyme immunoassays and the RIDAQUICK immunochromatographic test for the detection of norovirus in faecal specimens. J. Clin. Virol. 49, 254–257 (2010).
Panchalingam, S. et al. Diagnostic microbiologic methods in the GEMS-1 case/control study. Clin. Infect. Dis. 55, S294–S302 (2012).
Koplan, J.P., Fineberg, H.V., Ferraro, M.J. & Rosenberg, M.L. Value of stool cultures. Lancet 2, 413–416 (1980).
Blaser, M.J., Taylor, D.N. & Feldman, R.A. Epidemiology of Campylobacter jejuni infections. Epidemiol. Re.v 5, 157–176 (1983).
M'Ikanatha, N.M. et al. Culturing stool specimens for Campylobacter spp., Pennsylvania, USA. Emerg. Infect. Dis. 18, 484–487 (2012).
Lastovica, A.J. & Le Roux, E. Efficient isolation of Campylobacter upsaliensis from stools. J. Clin. Microbiol. 39, 4222–4223 (2001).
Man, S.M. The clinical importance of emerging Campylobacter species. Nat. Rev. Gastroenterol. Hepatol. 8, 669–685 (2011).
Bullman, S., O'Leary, J., Corcoran, D., Sleator, R.D. & Lucey, B. Molecular-based detection of non-culturable and emerging campylobacteria in patients presenting with gastroenteritis. Epidemiol. Infect. 140, 684–688 (2012).
Lastovica, A.J. Emerging Campylobacter spp.: the tip of the iceberg. Clin. Microbiol. Newsletter 28, 49–56 (2006).
Bullman, S. et al. Emerging dynamics of human campylobacteriosis in Southern Ireland. FEMS Immunol. Med. Microbiol. 63, 248–253 (2011).
Armah, G.E. et al. Efficacy of pentavalent rotavirus vaccine against severe rotavirus gastroenteritis in infants in developing countries in sub-Saharan Africa: a randomised, double-blind, placebo-controlled trial. Lancet 376, 606–614 (2010).
Cunliffe, N.A. et al. Efficacy of human rotavirus vaccine against severe gastroenteritis in Malawian children in the first two years of life: a randomized, double-blind, placebo controlled trial. Vaccine 30 (Suppl 1), A36–A43 (2012).
Madhi, S.A. et al. Effect of human rotavirus vaccine on severe diarrhea in African infants. N. Engl. J. Med. 362, 289–298 (2010).
Vesikari, T. et al. Efficacy of human rotavirus vaccine against rotavirus gastroenteritis during the first 2 years of life in European infants: randomised, double-blind controlled study. Lancet 370, 1757–1763 (2007).
Gunson, R., Miller, J., Leonard, A. & Carman, W. Importance of PCR in the diagnosis and understanding of rotavirus illness in the community. Commun. Dis. Public Health 6, 63–65 (2003).
Costantini, V. et al. Diagnostic accuracy and analytical sensitivity of IDEIA Norovirus assay for routine screening of human norovirus. J. Clin. Microbiol. 48, 2770–2778 (2010).
Gerritzen, A., Wittke, J.W. & Wolff, D. Rapid and sensitive detection of Shiga toxin-producing Escherichia coli directly from stool samples by real-time PCR in comparison to culture, enzyme immunoassay and Vero cell cytotoxicity assay. Clin. Lab. 57, 993–998 (2011).
Planche, T. et al. Diagnosis of Clostridium difficile infection by toxin detection kits: a systematic review. Lancet Infect. Dis. 8, 777–784 (2008).
Murdoch, D.R. et al. Laboratory methods for determining pneumonia etiology in children. Clin. Infect. Dis. 54 (Suppl 2), S146–S152 (2012).
Steinberg, E.B. et al. Prevalence of infection with waterborne pathogens: a seroepidemiologic study in children 6-36 months old in San Juan Sacatepequez, Guatemala. Am. J. Trop. Med. Hyg. 70, 83–88 (2004).
Priest, J.W. et al. Multiplex assay detection of immunoglobulin G antibodies that recognize Giardia intestinalis and Cryptosporidium parvum antigens. Clin. Vaccine Immunol. 17, 1695–1707 (2010).
Vlek, A.L.M., Bonten, M.J.M. & Boel, C.H.E. Direct matrix-assisted laser desorption ionization time-of-flight mass spectrometry improves appropriateness of antibiotic treatment of bacteremia. PLoS One 7, e32589 (2012).
Brinkman, C.L. et al. Polymerase chain reaction-electrospray ionization mass spectrometry for direct detection of pathogens and antimicrobial resistance from heart valves in patients with infective endocarditis. J. Clin. Microbiol. 51, 2040–2046 (2013).
Mengelle, C., Mansuy, J.M., Da Silva, I., Guerin, J.L. & Izopet, J. Evaluation of a polymerase chain reaction-electrospray ionization time-of-flight mass spectrometry for the detection and subtyping of influenza viruses in respiratory specimens. J. Clin. Virol. 57, 222–226 (2013).
Simner, P.J. et al. Broad-range direct detection and identification of fungi by use of the PLEX-ID PCR-electrospray ionization mass spectrometry (ESI-MS) system. J. Clin. Microbiol. 51, 1699–1706 (2013).
Luminex XTM Gastrointestinal Pathogen Panel. Available at http://www.luminexcorp.com/Products/Assays/ClinicalDiagnostics/xTAGGPP.
Petrich, A. et al. Multicenter comparison of nucleic acid extraction methods for detection of severe acute respiratory syndrome coronavirus RNA in stool specimens. J. Clin. Microbiol. 44, 2681–2688 (2006).
Shulman, L.M. et al. Evaluation of four different systems for extraction of RNA from stool suspensions using MS-2 coliphage as an exogenous control for RT-PCR inhibition. PLoS One 7, e39455 (2012).
Liu, J. et al. Multiplex reverse transcription PCR Luminex assay for detection and quantitation of viral agents of gastroenteritis. J. Clin. Virol. 50, 308–313 (2011).
Platts-Mills, J.A., Operario, D.J. & Houpt, E.R. Molecular diagnosis of diarrhea: current status and future potential. Curr. Infect. Dis. Rep. 14, 41–46 (2012).
Maher, M. et al. Evaluation of culture methods and a DNA probe-based PCR assay for detection of Campylobacter species in clinical specimens of feces. J. Clin. Microbiol. 41, 2980–2986 (2003).
Wolk, D.M., Schneider, S.K., Wengenack, N.L., Sloan, L.M. & Rosenblatt, J.E. Real-time PCR method for detection of Encephalitozoon intestinalis from stool specimens. J. Clin. Microbiol. 40, 3922–3928 (2002).
Amar, C.F.L. et al. Detection by PCR of eight groups of enteric pathogens in 4,627 faecal samples: re-examination of the English case-control Infectious Intestinal Disease Study (1993–1996). Eur. J. Clin. Microbiol. Infect. Dis. 26, 311–323 (2007).
Barletta, F. et al. Validation of five-colony pool analysis using multiplex real-time PCR for detection of diarrheagenic Escherichia coli. J. Clin. Microbiol. 47, 1915–1917 (2009).
Fujioka, M., Kasai, K., Miura, T., Sato, T. & Otomo, Y. Rapid diagnostic method for the detection of diarrheagenic Escherichia coli by multiplex PCR. Jpn. J. Infect. Dis. 62, 476–480 (2009).
Guion, C.E., Ochoa, T.J., Walker, C.M., Barletta, F. & Cleary, T.G. Detection of diarrheagenic Escherichia coli by use of melting-curve analysis and real-time multiplex PCR. J. Clin. Microbiol. 46, 1752–1757 (2008).
Rajendran, P. et al. Pathotypes of diarrheagenic Escherichia coli in children attending a tertiary care hospital in South India. Diagn. Microbiol. Infect. Dis. 68, 117–122 (2010).
Liu, J. et al. Simultaneous detection of six diarrhea-causing bacterial pathogens with an in-house PCR-luminex assay. J. Clin. Microbiol. 50, 98–103 (2012).
Taniuchi, M. et al. High throughput multiplex PCR and probe-based detection with Luminex beads for seven intestinal parasites. Am. J. Trop. Med. Hyg. 84, 332–337 (2011).
Kodani, M. et al. Application of TaqMan low-density arrays for simultaneous detection of multiple respiratory pathogens. J. Clin. Microbiol. 49, 2175–2182 (2011).
Rand, K.H., Rampersaud, H. & Houck, H.J. Comparison of two multiplex methods for detection of respiratory viruses: FilmArray RP and xTAG RVP. J. Clin. Microbiol. 49, 2449–2453 (2011).
Lin, A. et al. Rapid O serogroup identification of the ten most clinically relevant STECs by Luminex microbead-based suspension array. J. Microbiol. Methods 87, 105–110 (2011).
Liu, J. et al. A laboratory developed TaqMan Array Card for simultaneous detection of nineteen enteropathogens. J. Clin. Microbiol. 51, 472–480 (2013).
Haque, R. et al. Giardia assemblage A infection and diarrhea in Bangladesh. J. Infect. Dis. 192, 2171–2173 (2005).
Boggy, G.J. & Woolf, P.J. A mechanistic model of PCR for accurate quantification of quantitative PCR data. PLoS One 5, e12355 (2010).
Carr, A.C. & Moore, S.D. Robust quantification of polymerase chain reactions using global fitting. PLoS One 7, e37640 (2012).
Opel, K.L., Chung, D. & McCord, B.R. A study of PCR inhibition mechanisms using real time PCR. J. Forensic Sci. 55, 25–33 (2010).
Gregory, J.B., Litaker, R.W. & Noble, R.T. Rapid one-step quantitative reverse transcriptase PCR assay with competitive internal positive control for detection of enteroviruses in environmental samples. Appl. Environ. Microbiol. 72, 3960–3967 (2006).
Hata, A. et al. Validation of internal controls for extraction and amplification of nucleic acids from enteric viruses in water samples. Appl. Environ. Microbiol. 77, 4336–4343 (2011).
Dreier, J., Stormer, M. & Kleesiek, K. Use of bacteriophage MS2 as an internal control in viral reverse transcription-PCR assays. J. Clin. Microbiol. 43, 4551–4557 (2005).
Kaper, J.B., Nataro, J.P. & Mobley, H.L. Pathogenic Escherichia coli. Nat. Rev. Microbiol. 2, 123–140 (2004).
Estrada-Garcia, T. & Navarro-Garcia, F. Enteroaggregative Escherichia coli pathotype: a genetically heterogeneous emerging foodborne enteropathogen. FEMS Immunol. Med. Microbiol. 66, 281–298 (2012).
Boisen, N. et al. Genomic characterization of enteroaggregative Escherichia coli from children in Mali. J. Infect. Dis. 205, 431–444 (2012).
Cangelosi, G.A., Weigel, K.M., Lefthand-Begay, C. & Meschke, J.S. Molecular detection of viable bacterial pathogens in water by ratiometric pre-rRNA analysis. Appl. Environ. Microbiol. 76, 960–962 (2010).
Liang, Z. & Keeley, A. Detection of viable Cryptosporidium parvum in soil by reverse transcription-real-time PCR targeting hsp70 mRNA. Appl. Environ. Microbiol. 77, 6476–6485 (2011).
Fittipaldi, M., Nocker, A. & Codony, F. Progress in understanding preferential detection of live cells using viability dyes in combination with DNA amplification. J. Microbiol. Methods 91, 276–289 (2012).
Chin, C.S. et al. The origin of the Haitian cholera outbreak strain. N. Engl. J. Med. 364, 33–42 (2011).
He, M. et al. Emergence and global spread of epidemic healthcare-associated Clostridium difficile. Nat. Genet. 45, 109–113 (2013).
Mellmann, A. et al. Prospective genomic characterization of the German enterohemorrhagic Escherichia coli O104:H4 outbreak by rapid next generation sequencing technology. PLoS One 6, e22751 (2011).
Bielaszewska, M. et al. Characterisation of the Escherichia coli strain associated with an outbreak of haemolytic uraemic syndrome in Germany, 2011: a microbiological study. Lancet Infect. Dis. 11, 671–676 (2011).
Schlaberg, R., Simmon, K.E. & Fisher, M.A. A systematic approach for discovering novel, clinically relevant bacteria. Emerg. Infect. Dis. 18, 422–430 (2012).
Finkbeiner, S.R. et al. Metagenomic analysis of human diarrhea: viral detection and discovery. PLoS Pathog. 4, e1000011 (2008).
Rampini, S.K. et al. Broad-range 16S rRNA gene polymerase chain reaction for diagnosis of culture-negative bacterial infections. Clin. Infect. Dis. 53, 1245–1251 (2011).
Smits, S.L. et al. Calicivirus from novel Recovirus genogroup in human diarrhea, Bangladesh. Emerg. Infect. Dis. 18, 1192–1195 (2012).
Yu, G. et al. Discovery of a novel polyomavirus in acute diarrheal samples from children. PLoS One 7, e49449 (2012).
Levine, M.M., Kotloff, K.L., Nataro, J.P. & Muhsen, K. The Global Enteric Multicenter Study (GEMS): impetus, rationale, and genesis. Clin. Infect. Dis. 55, S215–S224 (2012).
Didelot, X., Bowden, R., Wilson, D.J., Peto, T.E. & Crook, D.W. Transforming clinical microbiology with bacterial genome sequencing. Nat. Rev. Genet. 13, 601–612 (2012).
Relman, D.A. Microbial genomics and infectious diseases. N. Engl. J. Med. 365, 347–357 (2011).
Miller, W.G. et al. Multilocus sequence typing methods for the emerging Campylobacter species C. hyointestinalis, C. lanienae, C. sputorum, C. concisus, and C. curvus. Front. Cell Infect. Microbiol. 2, 45 (2012).
Jolley, K.A. et al. Ribosomal multilocus sequence typing: universal characterization of bacteria from domain to strain. Microbiology 158, 1005–1015 (2012).
Taylor, J.W. & Fisher, M.C. Fungal multilocus sequence typing—it's not just for bacteria. Curr. Opin Microbiol. 6, 351–356 (2003).
Zhang, M. et al. Pattern extraction of structural responses of gut microbiota to rotavirus infection via multivariate statistical analysis of clone library data. FEMS Microbiol. Ecol. 70, 21–29 (2009).
Nelson, A.M. et al. Disruption of the human gut microbiota following Norovirus infection. PLoS One 7, e48224 (2012).
Chang, J.Y. et al. Decreased diversity of the fecal Microbiome in recurrent Clostridium difficile-associated diarrhea. J. Infect. Dis. 197, 435–438 (2008).
Lawley, T.D. et al. Targeted restoration of the intestinal microbiota with a simple, defined bacteriotherapy resolves relapsing Clostridium difficile disease in mice. PLoS Pathog. 8, e1002995 (2012).
van Nood, E. et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N. Engl. J. Med. 368, 407–415 (2013).
Kosek, M., Yori, P.P. & Olortegui, M.P. Shigellosis update: advancing antibiotic resistance, investment empowered vaccine development, and green bananas. Curr. Opin. Infect. Dis. 23, 475–480 (2010).
Kim, J. et al. Multiplex real-time polymerase chain reaction-based method for the rapid detection of gyrA and parC mutations in quinolone-resistant Escherichia coli and Shigella spp. Osong Public Health Res. Perspect. 3, 113–117 (2012).
Jones, T.F. & Gerner-Smidt, P. Nonculture diagnostic tests for enteric diseases. Emerg. Infect. Dis. 18, 513–514 (2012).
de Boer, R.F., Ott, A., Kesztyus, B. & Kooistra-Smid, A.M. Improved detection of five major gastrointestinal pathogens by use of a molecular screening approach. J. Clin. Microbiol. 48, 4140–4146 (2010).
Casadevall, A., Fang, F.C. & Pirofski, L.A. Microbial virulence as an emergent property: consequences and opportunities. PLoS Pathog. 7, e1002136 (2011).
Casadevall, A. & Pirofski, L.A. Host-pathogen interactions: basic concepts of microbial commensalism, colonization, infection, and disease. Infect. Immun. 68, 6511–6518 (2000).
Casadevall, A. & Pirofski, L.A. Host-pathogen interactions: redefining the basic concepts of virulence and pathogenicity. Infect. Immun. 67, 3703–3713 (1999).
Fredericks, D.N. & Relman, D.A. Sequence-based identification of microbial pathogens: a reconsideration of Koch's postulates. Clin. Microbiol. Rev. 9, 18–33 (1996).
Coulthard, M.G. et al. Redefining urinary tract infections by bacterial colony counts. Pediatrics 125, 335–341 (2010).
Fujisawa, T. et al. Real-time PCR is more specific than conventional PCR for induced sputum diagnosis of Pneumocystis pneumonia in immunocompromised patients without HIV infection. Respirology 14, 203–209 (2009).
Alexander, N. et al. Selection and quantification of infection endpoints for trials of vaccines against intestinal helminths. Vaccine 29, 3686–3694 (2011).
Chappell, C.L., Okhuysen, P.C., Sterling, C.R. & DuPont, H.L. Cryptosporidium parvum: intensity of infection and oocyst excretion patterns in healthy volunteers. J. Infect. Dis. 173, 232–236 (1996).
El Shazly, A.M., Soltan, D.M., El-Sheikha, H.M., Sadek, G.S. & Morsy, A.T. Correlation of ELISA copro-antigen and oocysts count to the severity of Cryptosporidiosis parvum in children. J. Egypt Soc. Parasitol. 37, 107–120 (2007).
Levecke, B., Mekonnen, Z., Albonico, M. & Vercruysse, J. The impact of baseline faecal egg counts on the efficacy of single-dose albendazole against Trichuris trichiura. Trans. R. Soc. Trop. Med. Hyg. 106, 128–130 (2012).
Levecke, B., Speybroeck, N., Dobson, R.J., Vercruysse, J. & Charlier, J. Novel insights in the fecal egg count reduction test for monitoring drug efficacy against soil-transmitted helminths in large-scale treatment programs. PLoS Negl. Trop. Dis. 5, e1427 (2011).
Kang, G. et al. Quantitation of group A rotavirus by real-time reverse-transcription-polymerase chain reaction: correlation with clinical severity in children in South India. J. Med. Virol. 73, 118–122 (2004).
Phillips, G. et al. Diagnosing norovirus-associated infectious intestinal disease using viral load. BMC Infect. Dis. 9, 63 (2009).
Atmar, R.L. et al. Norwalk virus shedding after experimental human infection. Emerg. Infect. Dis. 14, 1553–1557 (2008).
Lopez, S. & Arias, C.F. Rotavirus-host cell interactions: an arms race. Curr. Opin. Virol. 2, 389–398 (2012).
Barletta, F. et al. Quantitative real-time polymerase chain reaction for enteropathogenic Escherichia coli: a tool for investigation of asymptomatic versus symptomatic infections. Clin. Infect. Dis. 53, 1223–1229 (2011).
Kotloff, K.L. et al. The Global Enteric Multicenter Study (GEMS) of diarrheal disease in infants and young children in developing countries: epidemiologic and clinical methods of the case/control study. Clin. Infect. Dis. 55, S232–S245 (2012).
Perrigoue, J.G., Zaph, C., Guild, K., Du, Y. & Artis, D. IL-31-IL-31R interactions limit the magnitude of Th2 cytokine-dependent immunity and inflammation following intestinal helminth infection. J. Immunol. 182, 6088–6094 (2009).
Hasnain, S.Z., McGuckin, M.A., Grencis, R.K. & Thornton, D.J. Serine protease(s) secreted by the nematode Trichuris muris degrade the mucus barrier. PLoS Negl. Trop. Dis. 6, e1856 (2012).
Houpt, E. et al. Prevention of intestinal amebiasis by vaccination with the Entamoeba histolytica Gal/GalNac lectin. Vaccine 22, 611–617 (2004).
Basu, R. et al. Th22 cells are an important source of IL-22 for host protection against enteropathogenic bacteria. Immunity 37, 1061–1075 (2012).
Glass, R.I. et al. Predisposition for cholera of individuals with O blood group. Possible evolutionary significance. Am. J. Epidemiol. 121, 791–796 (1985).
Swerdlow, D.L. et al. Severe life-threatening cholera associated with blood group O in Peru: implications for the Latin American epidemic. J. Infect. Dis. 170, 468–472 (1994).
Hutson, A.M., Atmar, R.L., Graham, D.Y. & Estes, M.K. Norwalk virus infection and disease is associated with ABO histo-blood group type. J. Infect. Dis. 185, 1335–1337 (2002).
Zaman, K. et al. Efficacy of pentavalent rotavirus vaccine against severe rotavirus gastroenteritis in infants in developing countries in Asia: a randomised, double-blind, placebo-controlled trial. Lancet 376, 615–623 (2010).
Cooper, P.J. et al. Human infection with Ascaris lumbricoides is associated with suppression of the interleukin-2 response to recombinant cholera toxin B subunit following vaccination with the live oral cholera vaccine CVD 103-HgR. Infect. Immun. 69, 1574–1580 (2001).
Wang, H., Moon, S., Wang, Y. & Jiang, B. Multiple virus infection alters rotavirus replication and expression of cytokines and Toll-like receptors in intestinal epithelial cells. Virus Res. 167, 48–55 (2012).
Lagos, R. et al. Effect of small bowel bacterial overgrowth on the immunogenicity of single-dose live oral cholera vaccine CVD 103-HgR. J. Infect. Dis. 180, 1709–1712 (1999).
Braeckman, T. et al. Effectiveness of rotavirus vaccination in prevention of hospital admissions for rotavirus gastroenteritis among young children in Belgium: case-control study. BMJ 345, e4752 (2012).
Meisel, J.L., Perera, D.R., Meligro, C. & Rubin, C.E. Overwhelming watery diarrhea associated with a cryptosporidium in an immunosuppressed patient. Gastroenterology 70, 1156–1160 (1976).
DuPont, H.L. et al. The infectivity of Cryptosporidium parvum in healthy volunteers. N. Engl. J. Med. 332, 855–859 (1995).
Goodgame, R.W., Genta, R.M., White, A.C. & Chappell, C.L. Intensity of infection in AIDS-associated cryptosporidiosis. J. Infect. Dis. 167, 704–709 (1993).
Houpt, E.R. et al. Short report: asymptomatic Cryptosporidium hominis infection among human immunodeficiency virus-infected patients in Tanzania. Am. J. Trop. Med. Hyg. 73, 520–522 (2005).
Tzipori, S., Rand, W. & Theodos, C. Evaluation of a two-phase scid mouse model preconditioned with anti-interferon-gamma monoclonal antibody for drug testing against Cryptosporidium parvum. J. Infect. Dis. 172, 1160–1164 (1995).
McDonald, V., Robinson, H.A., Kelly, J.P. & Bancroft, G.J. Cryptosporidium muris in adult mice: adoptive transfer of immunity and protective roles of CD4 versus CD8 cells. Infect. Immun. 62, 2289–2294 (1994).
Fayer, R., Perryman, L.E. & Riggs, M.W. Hyperimmune bovine colostrum neutralizes Cryptosporidium sporozoites and protects mice against oocyst challenge. J. Parasitol. 75, 151–153 (1989).
Greenberg, P.D. & Cello, J.P. Treatment of severe diarrhea caused by Cryptosporidium parvum with oral bovine immunoglobulin concentrate in patients with AIDS. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 13, 348–354 (1996).
Kassa, M., Comby, E., Lemeteil, D., Brasseur, P. & Ballet, J.J. Characterization of anti-Cryptosporidium IgA antibodies in sera from immunocompetent individuals and HIV-infected patients. J. Protozool. 38, 179S–180S (1991).
Xiao, L. Molecular epidemiology of cryptosporidiosis: an update. Exp. Parasitol. 124, 80–89 (2010).
Eastwood, K., Else, P., Charlett, A. & Wilcox, M. Comparison of nine commercially available Clostridium difficile toxin detection assays, a real-time PCR assay for C. difficile tcdB, and a glutamate dehydrogenase detection assay to cytotoxin testing and cytotoxigenic culture methods. J. Clin. Microbiol. 47, 3211–3217 (2009).
Tenover, F.C. et al. Impact of strain type on detection of toxigenic Clostridium difficile: comparison of molecular diagnostic and enzyme immunoassay approaches. J. Clin. Microbiol. 48, 3719–3724 (2010).
Swindells, J., Brenwald, N., Reading, N. & Oppenheim, B. Evaluation of diagnostic tests for Clostridium difficile infection. J. Clin. Microbiol. 48, 606–608 (2010).
Longtin, Y. et al. Impact of the type of diagnostic assay on Clostridium difficile infection and complication rates in a mandatory reporting program. Clin. Infect. Dis. 56, 67–73 (2013).
Ryder, A.B. et al. Assessment of Clostridium difficile infections by quantitative detection of tcdB toxin by use of a real-time cell analysis system. J. Clin. Microbiol. 48, 4129–4134 (2010).
Matsuda, K. et al. Sensitive quantification of Clostridium difficile cells by reverse transcription-quantitative PCR targeting rRNA molecules. Appl. Environ. Microbiol. 78, 5111–5118 (2012).
Lowy, I. et al. Treatment with monoclonal antibodies against Clostridium difficile toxins. N. Engl. J. Med. 362, 197–205 (2010).
Salcedo, J. et al. Intravenous immunoglobulin therapy for severe Clostridium difficile colitis. Gut 41, 366–370 (1997).
Acknowledgements
This work was supported by a NIH U01 AI075396 and a Bill and Melinda Gates Foundation Global Health Grant OPP1019093 (to E.R.H.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declared no conflict of interest.
Rights and permissions
About this article
Cite this article
Platts-Mills, J., Liu, J. & Houpt, E. New concepts in diagnostics for infectious diarrhea. Mucosal Immunol 6, 876–885 (2013). https://doi.org/10.1038/mi.2013.50
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mi.2013.50
This article is cited by
-
Etiologic features of diarrheagenic microbes in stool specimens from patients with acute diarrhea in Thailand
Scientific Reports (2020)
-
Evaluation of the Vibrant DNA microarray for the high-throughput multiplex detection of enteric pathogens in clinical samples
Gut Pathogens (2019)
-
Association between semi-quantitative microbial load and respiratory symptoms among Thai military recruits: a prospective cohort study
BMC Infectious Diseases (2018)
-
Fecal microbial characterization of hospitalized patients with suspected infectious diarrhea shows significant dysbiosis
Scientific Reports (2017)
-
Automated nucleic acids purification from fecal samples on a microfluidic cartridge
BioChip Journal (2017)