Abstract
α4 and β7 integrins, such as α4β1, α4β7, and αEβ7, are major integrins required for migration of leukocytes into mucosal tissues. The mechanisms responsible for coordinated expression of these three integrins have been poorly elucidated to date. We report that expression of the Itg-α4 subunit by both CD4+ and CD8+ T cells requires the retinoic acid signal. In contrast, transcription of Itg-αE genes is induced by the transforming growth factor-β1 (TGFβ1) signal. Expression of Itg-β7 is constitutive but can be further increased by TGFβ1. Consistently, expression of α4-containing integrins is severely suppressed in vitamin A deficiency with a compensatory increase of αEβ7, whereas expression of Itg-αE and Itg-β7 is decreased in TGFβ-signal deficiency with a compensatory increase in α4β1. The retinoic acid-mediated regulation of α4 integrins is required for specific migration of T cells in vitro and in vivo. These results provide central regulatory mechanisms for coordinated expression of the major mucosal integrins.
Similar content being viewed by others
Introduction
Integrin α4, a subunit of α4β1 (CD49d–CD29) and α4β7, is a major target of intervention in treating inflammatory diseases through blocking leukocyte migration.1, 2 α4β1, also known as VLA4 (very late antigen 4), is expressed by T cells, B cells, monocytes, and eosinophils.3, 4 α4β7, once called lamina propria-associated molecule 1, is expressed by T cells and B cells in mucosal tissues.5, 6 α4β1 and α4β7 each bind its major counter receptor vascular cell adhesion molecule 1 (VCAM-1) and Mad CAM-1, respectively. α4β7 also binds VCAM-1 and fibronectin, but at reduced affinity.7 The α4 integrins are involved in both rolling and firm adhesion of leukocytes on endothelial cells.8, 9 α4β1 is involved in leukocyte migration to diverse tissues including mucosal tissues, bone marrow, splenic follicles, and inflamed tissues, whereas α4β7 has a more specific role in lymphocyte migration to the gut and associated lymphoid tissues.10, 11, 12, 13, 14 αEβ7, an integrin related to α4β1 and α4β7, binds E-cadherin expressed on epithelial cells.15 αEβ7 is involved in the localization and function of both effector and regulatory T cells.16, 17
Retinoic acid, such as all-trans retinoic acid (RA), is a vitamin A metabolite and highly produced by epithelial cells and dendritic cells in the small intestine.18 RA has a number of regulatory functions in the immune system. It is required for differentiation of promyelocytes into neutrophils.19, 20, 21 It promotes the generation of small intestine-homing T and B cells.22, 23 In this regard, a severe paucity of T cells and immunoglobulin A-producing B cells occurs in the intestine because of vitamin A deficiency. These functions of RA are consistent with the increased susceptibility of vitamin A-deficient subjects to a number of infectious microbial agents.24 RA specifically induces the expression of a small intestine-homing chemokine receptor, chemokine (C-C motif) receptor 9 (CCR9), and a mucosal tissue-homing integrin molecule α4β7.22
It has been unclear how the mucosal integrins such as α4β1, α4β7, and αEβ7 are coordinately expressed. Through genome-wide gene expression and functional studies, we identified that expression of the Itg-α4 chain in T cells requires RA, whereas optimal transcription of Itg-αE and to a lesser degree Itg-β7 genes requires the transforming growth factor-β (TGFβ) signal. We provide detailed evidence that functional expression of Itg-α4- or Itg-αE-subunit-containing integrins by T cells is coordinately regulated by RA and TGFβ1. The effect of the integrin regulation pathways on T-cell migration in physiological settings is discussed.
Results
RA selectively induces the transcription of Itg-α4 gene
To understand the function of RA in regulation of mucosal integrin expression in T cells, we activated naive CD4+ T cells in the presence of exogenous RA at a physiologically relevant concentration (10 nm). As controls, we cultured the T cells without exogenous RA or in the presence of Ro41-5253 (a retinoic acid receptor-α (RARα) antagonist; hereafter simply referred to as “Ro41”) to block the effect of residual RA that is present in normal culture medium supplemented with 10% fetal bovine serum. It is estimated that 0.2–0.5 nm of RA is present in the culture medium because animal plasma–serum typically contains RA at 2–5 nm.25 We performed a genome-wide microarray study and found that the Itg-α4 gene is highly induced by the serum-derived RA present in the culture medium at low concentrations (Figure 1a). Interestingly, the microarray data revealed that expression of Itg-β1, Itg-β7, and Itg-αE was not significantly affected by different levels of RA (Figure 1b). We followed up the data with a real-time PCR assay and found that the Itg-α4 gene is responsive to RA in transcription, whereas the expression of Itg-β1 and Itg-β7 was not significantly affected by the presence or absence of the RA signal (Figure 1c). Itg-α4 transcription was further increased by exogenous RA at 1 and 10 nm. Interestingly, the real-time PCR assay revealed that Itg-αE mRNA was upregulated when Ro41 was used, which the microarray study failed to reveal.
Retinoic acid (RA)- and retinoic acid receptor-α (RARα)-dependent transcription of the Itg-α4 gene, but not Itg-β7, Itg-β1, and Itg-αE genes in CD4+ T cells. (a) A dot plot showing genes upregulated in response to high and low concentrations of RA. An Affymetrix microarray was used to determine the levels of gene expression. The x axis represents fold changes in gene expression between CD4+ T cells activated in control medium (containing low levels of RA) and CD4+ T cells cultured in the presence a RARα antagonist (Ro41-5253, abbreviated as “Ro41”). The y axis represents fold changes in gene expression between CD4+ T cells activated with exogenous RA (10 nm) and CD4+ T cells cultured in the presence a RARα antagonist (Ro41-5253). (b) Expression levels of integrin genes based on the microarray data. Error bars are differences between two independent array data sets. (c) Real-time PCR analysis of gene expression. Combined data of four independent sets are shown. The data are expressed relative to control T cells. *Significant differences from the controls. (d) Binding of RARα to retinoic acid response elements (RAREs) in the 5’ upstream regulatory region of the Itg-α4 gene. A chromatin immunoprecipitation (ChIP) assay was performed to determine RARα binding to RARE candidates on the 5’ upstream regulatory region of the Itg-α4 gene. RA (10 nm) was used. A representative data set from three independent experiments is shown. *Undetectable.
We performed a chromatin immunoprecipitation assay to assess the potential binding of nuclear RARα to the regulatory region of the Itg-α4 gene. On the basis of the DNA sequence analysis, we found a total of seven putative retinoic acid response elements (RAREs). The chromatin immunoprecipitation assay revealed that one of the putative RAREs is a real binding site for RARα (Figure 1d). RA enhanced the binding whereas Ro41 decreased the binding.
In addition to Itg-α4, many genes are up- or downregulated in T cells in response to RA. These genes are listed in Table 1 and in Supplementary Figure S1 online. Induction of CCR9 by RA, as reported previously,22 was clearly detectable. We confirmed by a real-time PCR method that growth hormone-regulated TBC protein 1 (GRTP1), cytochrome P450, family 26, subfamily b, polypeptide 1 (CYP26B1), dehydrogenase–reductase member 3 (DHRS3), and leucine zipper transcription factor-like 1 (LZTFL1) are induced by RA, whereas serine (or cysteine) proteinase inhibitor clade B member 1a (SERPINB1) is suppressed by RA (Supplementary Figure S1 online). GRTP1 is a GTPase activating protein that increases GTPase activity of Rab3A.26 CYP26B1 is a cytochrome P450 that catabolizes RA.27 DHRS3 is an enzyme that mediates the first oxidative conversion of retinol into retinal.28 LZTFL1 is a putative transcription factor with a leucine zipper domain and is a part of a transcriptional map that includes the CCR9 gene.29 SERPINB1 is an inhibitor of serine proteases such as elastase, cathepsin G, and proteinase-3.30 We focused our study in this report on regulation of the major mucosal integrins including Itg-α4.
T-cell activation in the presence of RA induces surface expression of both α4β1 and α4β7
Surface expression of integrins involves heterodimerization of integrin α and β subunits, and therefore simple expression of one subunit is not sufficient for its expression on the cell surface. It is a question of interest whether the α4 subunit induced by RA is required for all α4 subunit-containing integrins. We examined whether RA would have significant effects on surface expression of α4β1 and α4β7 (Figure 2a). T cells activated in the presence of Ro41 lost expression of Itg-α4. In contrast, Itg-β1 was expressed at high levels even with Ro41. Surface expression of Itg-β7 was enhanced with RA. Induction of surface Itg-α4 expression by RA is independent of exogenous TGFβ1 in culture. Itg-αE expression was not significantly changed by RA alone but increased with exogenous TGFβ1. These results, together with the regulation at the RNA level (Figure 1c), suggest that RA-dependent induction of Itg-α4 gene transcription is a driving force in the surface expression of both Itg-β7 and Itg-β1.
Expression of integrin proteins on the T-cell surface in response to a retinoic acid (RA) gradient. (a) Mouse CD4+ T cells were activated in the absence or presence of Ro41 or RA for 6 to 7 days and cell surface expression of selected integrins was determined by flow cytometry. Transforming growth factor-β1 (TGFβ1; 1 ng ml−1) was added to indicated cultures to determine any synergistic effects on induced FoxP3+ and FoxP3− T cells. (b) Expression of Itg-α4 and Itg-β1 by α4β7+ and α4β7− CD4+ T cells treated with RA and/or TGFβ1. (c) Effects of various retinoic acid receptor-α (RAR) agonists and antagonists on expression of Itg-α4, Itg-αE, Itg-β7, and Itg-β1 by T cells. Expression levels were calculated based on mean fluorescence intensity, which indicates levels of surface antigen expression. Graphs show combined relative expression levels after normalization with the controls (n=3–6). *Significant differences from the controls.
We also assessed the expression of the α4β7 heterodimer complex with the DATK32 antibody (Figure 2b). By gating out the α4β7+ cells, expression of the α4β1 complex by α4β7− T cells was also determined. It was apparent that expression of both α4β7 and α4β1 was increased in response to the RA signal.
To gain more insights into the RAR receptor usage, we used additional RAR agonists and antagonists such as LE540 (pan-RAR antagonist), CD2665 (RAR-β/γ antagonist), AM580 (RARα agonist), and AC55649 (RARβ2 agonist) along with RA (pan-RAR agonist) and Ro41 (RARα antagonist; Figure 2c). Although both AM580 and AC55649 induced the expression of Itg-α4, AM580 was more potent even at a lower dose (20 nm). Ro41 was more potent than CD2665. LE540 was most potent in the induction of Itg-β7 and Itg-αE. Overall, this information suggests that both the RARα and RARβ/γ receptors can regulate expression of the integrins, but RARα seems to have a larger role.
Flow cytometric determination of the perfect coexpression of Itg-αE and Itg-β7 or Itg-α4 and Itg-β7 revealed sharp needle-like double-positive populations that may be viewed as the result of autofluorescence or miscompensation in flow cytometry. Using appropriate isotype controls, we confirmed that these double-positive cells indeed have perfect coexpression of integrin subunits (Supplementary Figure S2 online).
Regular fetal bovine sera contain biologically active RA. We performed a similar culture experiment in a serum-free medium to rule out the effect of the residual RA (Supplementary Figure S3 online). We confirmed that RA induces Itg-α4. The T cells of the control group expressed Itg-α4 at levels similar to those of the Ro41-treated group. This rules out the possibility that the decreased Itg-α4 expression by Ro41 in a regular medium is because of an unexpected agonistic effect of Ro41.
We further examined the stability of the expressed integrins induced by RA using cycloheximide, a protein biosynthesis inhibitor (Supplementary Figure S4 online). We found that the induced integrins (α4β7, Itg-α4, Itg-β7, Itg-β1, and Itg-αE) were stable on the cell surface for at least 12 h after the treatment of cycloheximide.
T-cell expression of Itg-α4 is decreased in vitamin A deficiency
To confirm the regulatory role of RA in vivo, we induced vitamin A deficiency in mice and determined the expression of the integrins. We examined the integrin expression phenotype of T cells in the small intestine and spleen (a non-intestinal tissue). In the spleen, Itg-α4 was greatly decreased on both FoxP3− and FoxP3+ CD4+ T cells in vitamin A-deficient mice compared with control mice (Figure 3a). This decrease was relatively more severe on FoxP3+ T cells compared with FoxP3− T cells. Itg-β1expression was not affected by different vitamin A status. Itg-β7 was, unexpectedly, induced in vitamin A deficiency. In the small intestine, Itg-α4 was again decreased in vitamin A deficiency with almost no or minor change in the expression of Itg-β1 (Figure 3b). Itg-β7 was again strongly induced in vitamin A deficiency in the small intestine.
Expression of integrins in vitamin A deficiency. Expression of Itg-α4 and Itg-β7 by (a) spleen and (b) small intestinal lamina propria T-cell subsets in vitamin A-deficient, normal, and high mice. Expression of Itg-αE and Itg-β7 by (c) spleen and (d) small intestinal lamina propria T-cell subsets. Vitamin A-deficient, normal, and high mice were prepared, respectively, by feeding with special diets containing 0, 2,500, and 25,000 IU kg−1 for 12 to 13 weeks after birth. Representative and combined data (n=4) are shown. *Significant differences from the controls (2,500 U kg−1).
Increased surface expression of Itg-β7 in vitamin A deficiency is a mystery given the current perception that RA would induce Itg-β7 expression. We hypothesize that the enhanced expression of Itg-β7 in vitamin A deficiency would be the result of an increased expression of it's other dimerization partner, Itg-αE, in vitamin A deficiency. When we examined the expression of Itg-αE and Itg-β7, it was clear that most Itg-β7 molecules were coexpressed on T cells with the Itg-αE molecules in vitamin A deficiency (Figure 3c, d). This coexpression was evident on T cells in both spleen and small intestine. The tight coexpression of Itg-αE and Itg-β7 suggests that two subunits are probably complexed together in the same cells. Again, this regulation in vitamin A deficiency occurs on both FoxP3+ and FoxP3− T cells. Overall, there is a clear change from T cells expressing α4β1 and α4β7 in the mice with normal vitamin A status to those expressing αEβ7 in vitamin A deficiency (Supplementary Figure S5 online).
The TGFβ signal is required for functional expression of Itg-β7 and Itg-αE
A question critical for expression of both α4β7 and αEβ7 is what would regulate the transcription of the Itg-β7 gene. TGFβ is implicated in upregulation of Itg-β7 in a cytotoxic lymphoma cell line.31 We examined whether the TGFβ signal is required for expression of Itg-β7 in primary CD4+ T cells using T cells isolated from transgenic mice expressing a dominant negative form of TGFβRII (dnTGFβRII mice).32 The T cells in these mice are largely defective in reception of the TGFβ signal. Naive T cells from the dnTGFβRII mice were ineffective in surface expression of Itg-β7 in response to RA, whereas expression of Itg-α4 was induced normally (Figure 4a). The induction of Itg-β7 on wild-type FoxP3+ T cells was even higher, whereas it was defective on the transgenic FoxP3+ T cells in the presence of exogenous TGFβ1. In addition, we observed that the surface expression of Itg-αE and Itg-β7 was induced in response to TGFβ1 and Ro41 on wild-type but not on the transgenic T cells (Figure 4a). CD103–αEβ7, induced by TGFβ1 as determined in this study, is commonly viewed as a FoxP3+ T cell-specific marker. We would like to point out that this is not accurate, because the majority of CD4+ CD103+ T cells in non-lymphoid tissues such as the lung and intestine are FoxP3− T cells (Supplementary Figure S6 online). Moreover, even CD4+ FoxP3− T cells, differentiated in vitro in the presence of TGFβ1, highly expressed CD103 (Figure 4a).
Transforming growth factor-β1 (TGFβ1) signal is required for expression of Itg-β7 and Itg-αE. (a) Surface expression of α4β7 and αEβ7 in the presence and absence of TGFβ signal. A retinoic acid (RA) gradient is made with Ro41, RA (1 nm), and RA (10 nm) in 10% fetal bovine serum (FBS)-containing medium. TGFβ1 (1 ng ml−1) was added to indicated cultures. Naive CD4+ T cells, isolated from wild-type or dnTGFβRII mice, were cultured for 6 to 7 days in the different RA–TGFβ conditions. Representative data (n=4) are shown. (b) Expression of indicated Itg genes at the mRNA level is shown. Combined real-time PCR data with s.e.m. of three independent experiments is shown. (c) Expression of Itg-αE and Itg-β7 by the T cells in dnTGFβRII mice. (d) Expression of Itg-α4 and Itg-β1 by the T cells in dnTGFβRII mice. The graphs show combined data (percentage of positive cells among each T-cell subset) obtained from three different mice per group.
We next determined the expression levels of mRNA for Itg-αE and Itg-β7 in the wild-type and dnTGFβRII T cells cultured with RA or Ro41. We observed that dnTGFβRII T cells fail to express Itg-αE and Itg-β7 transcripts (Figure 4b). These results show that the TGFβ1 signal is required for expression of Itg-β7 and Itg-αE at the RNA level.
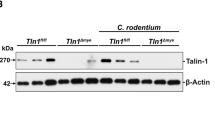
To gain insights into the function of the TGFβ signal in vivo, we determined the integrin expression phenotype of the T cells from dnTGFβRII mice. We found that expression of Itg-αE and Itg-β7 was decreased on CD4+ T cells in the spleen, small intestine, and large intestine (Figure 4c). Instead, there were increases in T cells expressing α4β1, which seems to be a compensatory response to the Itg-β7 decrease (Figure 4d). CD8+ T cells were highly similar to CD4+ T cells in expression of the integrins in dnTGFβRII mice.
Regulation of the integrins in CD8+ T cells
The results in Figure 4c, d on CD8+ T cells show that optimal expression of αEβ7 requires the TGFβ signal. We determined further whether expression of Itg-α4 and other Itg chains is induced by RA in CD8+ T cells. Similar to CD4+ T cells, Itg-α4 was strongly induced in response to RA (Figure 5a). Expression of Itg-αE and Itg-β7 was induced in response to TGFβ1. The overall Itg expression pattern of the CD8+ T cells cultured in a serum-free medium was similar to that cultured in a serum-containing medium (Figure 5b). The background expression level of Itg-α4 and Itg-β7 was higher in the serum-containing medium compared with the serum-free medium. We also observed that Itg-α4 mRNA expression was increased with the increasing RA signal (Supplementary Figure S7 online). Itg-αE transcription was increased with blocking with Ro41. Itg-β7 mRNA was highly expressed in CD8+ T cells in all conditions but was further increased by RA. This response of CD8+ T cells to RA is considered a minor difference from the CD4+ T cells.
Regulation of integrins on CD8+ T cells by retinoic acid (RA) and transforming growth factor-β1 (TGFβ1). Mouse CD8+ T cells were activated in the absence or presence of Ro41 or RA for 5 to 6 days in (a) a 10% fetal bovine serum (FBS)-containing medium or (b) a serum-free medium, and cell surface expression of selected integrins was determined by flow cytometry. The small subset of CD8+ FoxP3+ T cells were excluded from the analysis. TGFβ1 (1 ng ml−1) was added to indicated cultures to determine any synergistic effects. Graphs show combined relative expression levels after normalization for controls (n=3). *Significant differences from the controls.
The effect of RA-dependent Itg-α4 expression on T-cell migration
α4β1 binds VCAM-1 and fibronectin, and α4β7 binds MadCAM-1 and VCAM-1. Therefore, deficiency in Itg-α4 expression due to RARα blockade would have an important functional consequence on the migration of T cells. We examined whether the T cells with decreased expression of Itg-α4 due to RARα blockade would migrate normally on VCAM-1 in vitro (Figure 6a). The specificity of this migration was confirmed by PS/2 (an Itg-α4 blocking antibody)-dependent blocking of cell migration. Ro41-treated T cells were significantly defective in migration through the VCAM-1-coated Transwell membrane. This occurred not only in spontaneous migration but also in stromal cell-derived factor-1/CXCL12-induced chemotaxis (Figure 6a). To determine the effect only on α4β1, we used T cells isolated from Itg-β7 knockout mice as well. A similar reduction in migration through the VCAM-1-coated Transwell membrane was observed for Ro41-treated T cells (Figure 6b).
Functional effects of Itg-α4, induced by low concentrations of retinoic acid (RA), on migration of T cells in vitro and in vivo. (a, b) Migration of Itg-α4-low and normal T cells through vascular cell adhesion molecule 1 (VCAM1)-coated Transwells in response to stromal cell-derived factor-1 (SDF-1) or control medium was examined. Wild-type T cells can express both α4β1 and α4β7, whereas Itgβ7 (−/−) T cells express α4β1 but not α4β7. Combined data of three independent experiments are shown. Naive CD4+ T cells, isolated from (a) wild-type or (b) Itgβ7 (−/−) mice were cultured in the presence of control medium or Ro41 to prepare control and Itgα4-low T cells, respectively. PS/2, an Itg-α4 blocking monoclonal antibody, was used to block the Itg-α4-dependent migration. *Significant differences from control T cells. **Significant differences from the SDF-1 groups. (c) Surface phenotype of CD4+ T cells used for the in vivo homing study. Chemokine (C-C motif) receptor 9 (CCR9; −/−) naive CD4+ T cells were cultured in the presence of RA or Ro41 to prepare control and Itg-α4-low T cells. CCR9 (−/−) naive CD4+ T cells were used to exclude the effect of CCR9 (another trafficking receptor induced by RA) on migration. (d) Migration of Itg-α4-low T cells in vivo. A 20-h short-term in vivo homing assay to various organs including the peripheral lymph node (PLN), mesenteric lymph node (MLN), Peyer's patches (PP), small intestinal lamina propria (S-LP), and large intestinal lamina propria (L-LP) was performed. Homing indices <1 indicate decreased homing compared with control T cells. Combined data (n=4–6). (e) Intravital microscopy was performed to visualize the migrating Itg-α4-low and control CCR9 (−/−) T cells to Peyer's patches immediately after the T-cell transfer. A representative set of data of three independent experiments is shown. Error bars indicate s.d. of the number of cells per field (number of cells rolling, arrested, and migrated) in Peyer's patches in ∼20 image frames. *Significant decreases in migration.
We next assessed the in vivo migratory capacity of the Ro41-treated T cells compared with RA-treated T cells. Because CCR9, a major trafficking receptor to the small intestine,33, 34, 35, 36 is another receptor greatly induced by RA,22 we used T cells from CCR9-deficient mice to rule out the effect of CCR9 on in vivo migration of T cells (Figure 6c, d). We found that Ro41-treated CCR9-deficient T cells were defective in migration to the intestine and Peyer's patches compared with RA-treated CCR9-deficient T cells (Figure 6c). Their migration to the spleen, mesenteric lymph node, peripheral lymph node, and lung was not affected. Our intravital study revealed that there is a pronounced difference between Ro41-treated T cells and control RA-treated T cells in adhesion to the endothelium of Peyer's patches (Figure 6e). Thus, the RA-induced expression of Itg-α4 is functionally important for T-cell migration in vivo.
Discussion
Expression of integrins is regulated at several levels of biological processes, including transcription and other post-transcriptional regulatory events, translation in endoplasmic reticulum, dimerization, and transportation from endoplasmic reticulum to the cell surface.37 Transcription in response to specific induction signals has a central role in the expression of certain integrins. Another important factor for the expression of integrins is availability of heterodimerization partners because monomers cannot be expressed on the cell surface.38, 39 Availability of dimerization partners is particularly important for the coordinated expression of α4β1 and α4β7, which share the common α4 subunit. Similarly, expression of α4β7 is linked to αEβ7 because of the common β7 subunit.
We investigated the signals required for the induction of Itg-α4 and related integrins. We found that Itg-α4 is the integrin that is highly upregulated by RA (Figure 7a). Even at low residual concentrations in a regular medium containing 10% fetal bovine serum (∼0.5 nm), RA is sufficient to induce Itg-α4 transcription. This suggests that induction of Itg-α4 chain can occur widely in the body at the plasma concentration of RA. This is different from CCR9, which is induced at higher levels (>5 nm) of exogenous RA. This difference in sensitivity to RA would limit the expression of CCR9 to the small-intestinal T cells, whereas α4 integrins, particularly α4β1, is more widely expressed on antigen-primed T cells in most tissues. Because Itg-α4 is the common subunit for α4β1 and α4β7, RA provides a regulatory signal critical for the expression of the two integrin complexes. On the other hand, RA–vitamin A deficiency induces the expression of αEβ7 despite the fact that this molecule shares the Itg-β7 chain with α4β7. This confirms that RA is not required for transcription of Itg-αE and Itg-β7. Indeed, we found that Itg-αE is mainly upregulated by a different signal provided by TGFβ1. Itg-β7 is constitutively expressed and can be further induced by TGFβ1. We did not examine the roles of TGFβ isoforms other than TGFβ1 in integrin regulation. In support of our findings, it was previously reported that transcription of Itg-αE and Itg-β7 in a CD8+ leukemic T cell line (TK-1) can be increased by TGFβ1.31 Whether TGFβ1 induces the expression of Itg-αE and Itg-β7 in primary naive CD4+ T cells during antigen priming has not been determined despite the fact that natural and TGFβ1-induced FoxP3+ T cells highly express αEβ7.17, 41
Coordinated regulation of the expression of α4β1, α4β7, and αEβ7 by retinoic acid (RA) and transforming growth factor-β1 (TGFβ1) in T cells. (a) RA positively induces Itg-α4 (red lines) but RA paucity induces Itg-αE (blue lines). In contrast, Itg-αE is induced by TGFβ1 (green lines), whereas Itg-β1 is constitutively expressed by activated T cells. Itg-β7 is constitutively expressed but can be further induced by TGFβ1. In addition, RA seems to increase Itg-β7 expression in CD8+ T cells. Because of the heterodimerization requirement, expression of the three integrins is influenced by RA and TGFβ signals in combination. α4β1 can be induced by RA alone, whereas high expression of α4β7 requires both RA and TGFβ1. High expression of αEβ7 requires TGFβ1. In the intestine and other tissues, in which RA is available at optimal concentrations, high expression of α4β1 and α4β7 by T cells occurs. (b) In vitamin A deficiency, decreases in expression of α4β1 and α4β7 but increases in αEβ7 occur because of decreased Itg-α4 and increased Itg-αE expression. In a TGFβ signal deficiency, α4β1 is overexpressed because the expression of α4β7 (and αEβ7) is suppressed, freeing up Itg-α4 molecules for pairing with Itg-β1. Reciprocally, α4β7 is overexpressed when α4β1 is not expressed because of Itg-β1 deficiency.40 This regulatory mechanism operates in most T cells, including FoxP3+, CD4+, and CD8+ T cells. The size of integrins in the diagram signifies the amount of expression.
Although both Itg-β7 and Itg-β1 are upregulated on the surface of T cells in response to RA, RA seems to have no essential role in transcription of these molecules. The increased expression of α4β1 and α4β7 in response to RA is largely because of increased transcription and expression of Itg-α4. Although we observed a certain increase of Itg-β7 transcription in CD8 T cells in response to RA, this induction seems to be not important for α4β7 expression, as Itg-β7 is not a limiting factor. Thus, increased availability of Itg-α4 leads to increased assembly of integrin complexes formed between pre-existing Itg-β1 or Itg-β7 chains and the RA-induced Itg-α4 chain. This is supported by a recent publication by Shimizu group40 that levels of Itg-β1 expression can negatively affect α4β7 expression through competition for Itg-α4 molecules available for dimerization. Reciprocally, we found that decreased expression of Itg-β7, as observed in T cells of CD4-dnTβRII mice, can lead to increased expression of α4β1. In addition, we need to consider that there are many additional β1 integrins besides α4β1, which could further affect the regulation of the integrins. Thus, competition between Itg-β subunits is an important factor in the surface expression of α4 integrins (Figure 7b).
The surface expression of the Itg-β7 chain was greatly increased in response to RAR blockade or in vitamin A deficiency, because its pairing partner, the Itg-αE subunit, is greatly induced in this condition in a manner dependent on the TGFβ1 signal. This upregulation of αEβ7 in RA deficiency is probably because of increased availability of Itg-β7 molecules for pairing with Itg-αE when Itg-α4 expression is severely decreased (Figure 7b). Another mechanism is active induction of Itg-αE transcription in RA deficiency.
The two integrins α4β1 and α4β7 have critical roles in lymphocyte migration for both homeostatic and inflammatory purposes. Normal expression of α4β1 and α4β7 is required for mounting effective immunity and inducing chronic inflammation. Moreover, Itg-α4 is an effective target for treatment of inflammatory diseases.42, 43 A side effect of blocking Itg-α4 is increased susceptibility to infection.44, 45 Our results show that α4β1 and α4β7 integrins are greatly decreased on the surface of T cells in vitamin A deficiency. Decreased expression of these integrins leads to defective migration to various mucosal tissues such as the lung and intestine. It is likely that the increased susceptibility to infection in vitamin A-deficient individuals is, in part, because of the decreased expression of the α4 integrins and consequentially lowered effector functions of immune cells.46
The changes in expression levels of α4β1, α4β7, and αEβ7 in different retinoid–vitamin A status occur in all of the T-cell subsets examined in this study such as CD4+ T cells and CD8+ T cells. It is particularly notable that expression of the integrins by RA and TGFβ1 is more clearly regulated in FoxP3+ T cells. We believe that this is, in part, because of the fact that TGFβ1 is required for induction of both FoxP3 and integrins (i.e., Itg-αE and Itg-β7). Therefore, the RA- and TGFβ-dependent regulation of the integrins would have profound effects on migration and function of FoxP3+ T cells as well. Defective migration of FoxP3+ T cells can promote inflammatory diseases and explains, in part, the increased inflammation in vitamin A deficiency.47
Methods
Cell isolation and culture. CD4+ T cells were isolated from pooled single-cell suspensions of spleen, mesenteric lymph nodes, and peripheral lymph node with the CD4+ T-cell isolation kit (Miltenyi Biotec, Auburn, CA). Cells expressing CD8, CD19, CD25, CD44, and CD69 were further depleted to obtain naive CD4+ T cells (purity of ∼95%). Total CD8+ T cells were isolated using the CD8+ T-cell isolation kit (Miltenyi Biotec), and were further depleted for CD4, CD19, CD25, CD44, and CD69 cells to obtain naive (CD8+CD25−CD44−CD69−) CD8+ T cells (purity of ∼93%). Naive cells were activated for 5 to 6 days with complete RPMI-1640 medium containing concanavalin A (2.5 μg ml−1) and human interleukin-2 (100 U ml−1) in the presence or absence of one of the agonists or antagonists: RA (=At-RA; 1 or 10 nm from Sigma Aldrich, St Louis, MO), Ro41-5253 (hereafter called Ro41, 500 nm, purchased from Biomol, Farmingdale, NY), LE540 (500 nm, pan-RAR antagonist; Wako Chemical, Richmond, VA), CD2665 (500 nm, selective RAR-β/γ antagonist; Tocris Bioscience, Ellisville, MO), AM580 (20 nm, RARα agonist; Tocris), and AC55649 (100 nm, RARβ2 agonist; Tocris). Optimal concentrations of these reagents were determined by a preliminary titration study. Human TGFβ1 (1 ng ml−1) was used when indicated. For the experiment in Supplementary Figure S4 online, cycloheximide (10 μg ml−1; Enzo, Farmingdale, NY) was used. The T cells were also cultured in a serum-free medium (HL-1 from Lonza, Allendale, NJ) for 5 to 6 days with the T-cell activation–Expansion kit (anti-CD3 and CD28 beads: 6 μl per million cells; Miltenyi Biotec) and human interleukin-2 (100 U/ml−1) in the presence of RA (10 nm), Ro41 (100 nm), and/or TGFβ1 (1 ng ml−1).
Animals and generation of vitamin A-deficient or sufficient mice. All the experiments with animals in this study were approved by the Purdue animal care and use committee. CCR9-deficient mice were described previously.48 Itg-β7 (−/−) mice (C57BL/6-Itgb7tm1Cgn/J) and dominant form of TGFRII transgenic mice (B6.Cg-Tg(Cd4-TGFBR2)16Flv/J) were purchased from the Jackson Laboratory (Bar Harbor, ME). For generation of mice with excessive, normal, or deficient vitamin A status, BALB/c mice (Jackson Laboratory) were kept on custom diets based on AIN-93G containing high (25,000 IU kg−1; tenfold higher than the normal dietary range), normal (2,500 IU kg−1), or low (0 IU kg−1) (Harlon Teklad, Indianapolis, IN: TD-06528, 00158, and 07267) levels of vitamin A as previously described.49 The pups were weaned at 4 weeks of age and maintained on the same diets for additional 9 weeks. Vitamin A deficiency was verified by defective CCR9 expression by small intestinal T cells as described previously.49
Flow cytometry. Itg-α4 was stained sequentially with purified anti-mCD49d antibody (clone 9C10; BioLegend) followed by biotin anti-rat IgG2a (clone MRG2a-83; BioLegend) and Streptavidin-PerCP/Cy5.5 (BioLegend, San Diego, CA). To detect expression of Itg-β1, β7, and αE, respectively, antibodies to mCD29 (clone HMß1-1), mItg-β7 (clone FIB504), and mCD103 (clone 2E7) were used. Anti-mLPAM-1 (DATK32) was used to detect α4β7. When indicated, cells were stained for intracellular mFoxP3 with an antibody (clone FJK-16s; eBioscience, San Diego, CA). Stained cells were analyzed using a BD Canto II (BD Bioscience, San Diego, CA).
Homing experiment. Wild-type or CCR9-deficient T cells were prepared by culturing with RA or Ro41 and labeled with carboxyfluorescein diacetate succinimidyl ester (CFSE) or tetramethylrhodamine isothiocyanate (TRITC). The two cell types (5 million cells for each cell type per mouse) were co-injected through a tail vein into C57BL/6 mice. After 20 h, the mice were killed and single-cell suspensions were prepared from selected organs after collagenase digestion as previously described.50 The numbers of the injected CFSE+ or TRITC+ cells present in each organ was determined with flow cytometry. The relative homing index was determined according to the formula: homing index for organ A=(no. of TRITC+ cells in organ A)/(no. of CFSE+ cells in organ A) ÷ (no. of TRITC+ cells in input)/(no. of CFSE+ cells in input).
VCAM-1-dependent chemotaxis. Chemotaxis was performed with Transwells (3.0 μm pores; Corning, Corning, NY). The Transwells were coated with mouse VCAM-1 (100 μg ml−1; R&D Systems, Minneapolis, MN) in 50 μl of NaHCO3 (0.1 m, pH 8.0) by incubating overnight at 4 °C, and blocked with 2% bovine serum albumin for 30 min at room temperature. RA- (CFSE-labeled) and Ro41 (TRITC-labeled)-treated T cells (0.5 × 105 cells each) in 100 μl of chemotaxis buffer (RPMI-1640, 0.5% bovine serum albumin) were loaded onto the upper chamber. Stromal cell-derived factor-1α (100 ng ml−1, R&D Systems) was added to the lower chamber. Neutralizing anti-mItg-α4 monoclonal antibody (PS/2, 5 μg ml−1) was added to block the cells in the upper chamber when indicated. The cells were allowed to migrate for 4 h at 37 °C, and the cells that migrated to the lower chamber were counted with flow cytometry.
Intravital microscopy to monitor T-cell migration into gut lymphoid tissues. CCR9-deficient T cells, cultured with RA or Ro41 and labeled with CFSE or TRITC, were injected through a tail vein into C57BL/6 mice. Immediately after the injection of the labeled cell into anesthetized mice, Peyer's patches were exposed and observed in a custom-designed intravital device equipped with a Leica (Bannockburn, IL) DMI 3000B fluorescent microscope and a dynamic ultra low light fluorescence camera (Retiga-EXi; QImaging, Surrey, BC, Canada). The images were acquired every 0.5 s in sequence with the QCapture Pro6.0 software (Surrey, BC, Canada). Images were analyzed frame by frame for the presence of cells adhering to the endothelium, which include the cells under both rolling and sticking. Data from at least 30 images were averaged to obtain numbers of cells adhering to the Peyer's patch endothelium.
Microarray and data analysis. RNA, isolated from cultured CD4+ T cells, was hybridized to Mouse 430 2.0 chips (Affymetrix, Santa Clara, CA) by the Purdue Genomics Laboratory staff. These arrays contain over 39,000 complementary DNA spots corresponding to mouse sequence verified transcripts. Raw intensity values were obtained (GeneChip Operating Software, Affymetrix) and normalized with the expression values of a housekeeping gene (β-actin). Selection and filtering of high-quality genes was based on a twofold or greater differential in expression up or down between two conditions of comparison. Further selection was based on reproducibility between duplicated experiments, and transcripts without consistent results were dismissed. The gene expression values were visualized with the multiplot module of the GenePattern genomic analysis platform (www.broad.mit.edu/cancer/software/genepattern). The raw and processed array data have been deposited at http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE20500.
Chromatin immunoprecipitation assay. The chromatin immunoprecipitation assay was performed using a kit following the manufacturer's instruction (Upstate Biotechnology, Lake Placid, NY). In brief, 2 × 106 naive CD4+ T cells were cultured in the presence or absence of RA (10 nm) or Ro41 (500 nm). Concanavalin A (2.5 μg ml−1) and human interleukin-2 (25 U ml−1) were used to activate T cells. The cells were cultured for 4 to 5 days, fixed in paraformaldehyde, and made into cell lysates. The chromosomal DNA–protein complex was sonicated to generate DNA fragments with their size ranging from 200 to 1000 bp. DNA–protein complexes were immunoprecipitated using 4 μg of polyclonal antibody against mouse RARα (Santa Cruz Biotech, Santa Cruz, CA). Genomic DNA enriched with antibodies against RARα was uncross-linked and analyzed by PCR for detection of RAREs in the mouse Itg-α4 gene promoter with the following primer pairs: 5′-TACTTTGATGTCTATTTCTCTGG-3′ and 5′-GGATAGCAAGAAGTGCTGTCC-3′ (RARE1); 5′-AAGCCATCAGTGCTTCTCACC-3′ and 5′-GGAGAGACCTTGTGTCAAAGAA-3′ (RARE2); 5′-ATTCAGCTTGGCTGACAGGGA-3′ and 5′-TCC TTTTGCCTCTGCCTGCC-3′ (RARE3); 5′-TCCTATAAGCTTTGTTTTCAGCC-3′ and 5′-ACAACGTTTTATCTCATAAGTAATC-3′ (RARE4/5); 5′-AAAACTACCCATCTACTATAAACAA-3′ and 5′-CAACTCAAACTCCTATTAAGTTCT-3′ (RARE6); 5′-TCTGAACCTAGCAACTGCCAC-3′ and 5′-CCACTCCCAGTCTTTTGGAGA-3′ (RARE7). Real-time PCR detection was performed with a 7500 Sequence Detection System (Applied Biosystems, Foster City, CA) using the SYBR green Master Mix (Applied Biosystems).
Statistical analyses. Student's paired and unpaired t-tests were used to compare the significance of the differences between two groups of related or unrelated data. The P-values of ⩽0.05 were considered significant.
Accession codes
References
Linker, R.A., Kieseier, B.C. & Gold, R. Identification and development of new therapeutics for multiple sclerosis. Trends Pharmacol. Sci. 29, 558–565 (2008).
Rutgeerts, P., Vermeire, S. & Van Assche, G. Biological therapies for inflammatory bowel diseases. Gastroenterology 136, 1182–1197 (2009).
Morimoto, C., Iwata, S. & Tachibana, K. VLA-4-mediated signaling. Curr. Top. Microbiol. Immunol. 231, 1–22 (1998).
Wardlaw, A.J., Symon, F.S. & Walsh, G.M. Eosinophil adhesion in allergic inflammation. J. Allergy Clin. Immunol. 94, 1163–1171 (1994).
Andrew, D.P., Rott, L.S., Kilshaw, P.J. & Butcher, E.C. Distribution of alpha 4 beta 7 and alpha E beta 7 integrins on thymocytes, intestinal epithelial lymphocytes and peripheral lymphocytes. Eur. J. Immunol. 26, 897–905 (1996).
Fanjul, A.N. et al. 4-Hydroxyphenyl retinamide is a highly selective activator of retinoid receptors. J. Biol. Chem. 271, 22441–22446 (1996).
Pribila, J.T., Quale, A.C., Mueller, K.L. & Shimizu, Y. Integrins and T cell-mediated immunity. Annu. Rev. Immunol. 22, 157–180 (2004).
Alon, R. et al. The integrin VLA-4 supports tethering and rolling in flow on VCAM-1. J. Cell. Biol. 128, 1243–1253 (1995).
Berlin, C. et al. alpha 4 integrins mediate lymphocyte attachment and rolling under physiologic flow. Cell 80, 413–422 (1995).
von Andrian, U.H. & Engelhardt, B. Alpha4 integrins as therapeutic targets in autoimmune disease. N. Engl. J. Med. 348, 68–72 (2003).
Vermeulen, M. et al. Role of adhesion molecules in the homing and mobilization of murine hematopoietic stem and progenitor cells. Blood 92, 894–900 (1998).
Sigmundsdottir, H. & Butcher, E.C. Environmental cues, dendritic cells and the programming of tissue-selective lymphocyte trafficking. Nat. Immunol. 9, 981–987 (2008).
Hamann, A., Andrew, D.P., Jablonski-Westrich, D., Holzmann, B. & Butcher, E.C. Role of alpha 4-integrins in lymphocyte homing to mucosal tissues in vivo. J. Immunol. 152, 3282–3293 (1994).
Wolber, F.M. et al. Endothelial selectins and alpha4 integrins regulate independent pathways of T lymphocyte recruitment in the pulmonary immune response. J. Immunol. 161, 4396–4403 (1998).
Cepek, K.L. et al. Adhesion between epithelial cells and T lymphocytes mediated by E-cadherin and the alpha E beta 7 integrin. Nature 372, 190–193 (1994).
Schon, M.P. et al. Mucosal T lymphocyte numbers are selectively reduced in integrin alpha E (CD103)-deficient mice. J. Immunol. 162, 6641–6649 (1999).
Lehmann, J. et al. Expression of the integrin alpha Ebeta 7 identifies unique subsets of CD25+ as well as CD25- regulatory T cells. Proc. Natl. Acad. Sci. USA 99, 13031–13036 (2002).
Iwata, M. Retinoic acid production by intestinal dendritic cells and its role in T-cell trafficking. Semin. Immunol. 21, 8–13 (2009).
Gratas, C., Menot, M.L., Dresch, C. & Chomienne, C. Retinoid acid supports granulocytic but not erythroid differentiation of myeloid progenitors in normal bone marrow cells. Leukemia 7, 1156–1162 (1993).
Robertson, K.A., Emami, B., Mueller, L. & Collins, S.J. Multiple members of the retinoic acid receptor family are capable of mediating the granulocytic differentiation of HL-60 cells. Mol. Cell. Biol. 12, 3743–3749 (1992).
Tsai, S. & Collins, S.J. A dominant negative retinoic acid receptor blocks neutrophil differentiation at the promyelocyte stage. Proc. Natl. Acad. Sci. USA 90, 7153–7157 (1993).
Iwata, M. et al. Retinoic acid imprints gut-homing specificity on T cells. Immunity 21, 527–538 (2004).
Mora, J.R. et al. Generation of gut-homing IgA-secreting B cells by intestinal dendritic cells. Science (New York, NY) 314, 1157–1160 (2006).
Stephensen, C.B. Vitamin A, infection, and immune function. Annu. Rev. Nutr. 21, 167–192 (2001).
Napoli, J.L. Quantification of physiological levels of retinoic acid. Methods Enzymol. 123, 112–124 (1986).
Ishibashi, K., Kanno, E., Itoh, T. & Fukuda, M. Identification and characterization of a novel Tre-2/Bub2/Cdc16 (TBC) protein that possesses Rab3A-GAP activity. Genes Cells 14, 41–52 (2009).
Nelson, D.R. A second CYP26 P450 in humans and zebrafish: CYP26B1. Arch. Biochem. Biophys. 371, 345–347 (1999).
Haeseleer, F., Huang, J., Lebioda, L., Saari, J.C. & Palczewski, K. Molecular characterization of a novel short-chain dehydrogenase/reductase that reduces all-trans-retinal. J. Biol. Chem. 273, 21790–21799 (1998).
Kiss, H. et al. The LZTFL1 gene is a part of a transcriptional map covering 250 kb within the common eliminated region 1 (C3CER1) in 3p21.3. Genomics 73, 10–19 (2001).
Cooley, J., Takayama, T.K., Shapiro, S.D., Schechter, N.M. & Remold-O′Donnell, E. The serpin MNEI inhibits elastase-like and chymotrypsin-like serine proteases through efficient reactions at two active sites. Biochemistry 40, 15762–15770 (2001).
Lim, S.P., Leung, E. & Krissansen, G.W. The beta7 integrin gene (Itgb-7) promoter is responsive to TGF-beta1: defining control regions. Immunogenetics 48, 184–195 (1998).
Gorelik, L. & Flavell, R.A. Abrogation of TGFbeta signaling in T cells leads to spontaneous T cell differentiation and autoimmune disease. Immunity 12, 171–181 (2000).
Kunkel, E.J. et al. Lymphocyte CC chemokine receptor 9 and epithelial thymus-expressed chemokine (TECK) expression distinguish the small intestinal immune compartment: epithelial expression of tissue-specific chemokines as an organizing principle in regional immunity. J. Exp. Med. 192, 761–768 (2000).
Wurbel, M.A. et al. The chemokine TECK is expressed by thymic and intestinal epithelial cells and attracts double- and single-positive thymocytes expressing the TECK receptor CCR9. Eur. J. Immunol. 30, 262–271 (2000).
Hosoe, N. et al. Demonstration of functional role of TECK/CCL25 in T lymphocyte-endothelium interaction in inflamed and uninflamed intestinal mucosa. Am. J. Physiol. Gastrointest. Liver Physiol. 286, G458–466 (2004).
Stenstad, H. et al. Gut-associated lymphoid tissue-primed CD4+ T cells display CCR9-dependent and -independent homing to the small intestine. Blood 107, 3447–3454 (2006).
Humphries, M.J. Integrin structure. Biochem. Soc. Transac. 28, 311–339 (2000).
Z′Graggen, K., Walz, A., Mazzucchelli, L., Strieter, R.M. & Mueller, C. The C-X-C chemokine ENA-78 is preferentially expressed in intestinal epithelium in inflammatory bowel disease. Gastroenterology 113, 808–816 (1997).
Zeller, Y., Lohr, J., Sammar, M., Butcher, E.C. & Altevogt, P. Asp-698 and Asp-811 of the integrin alpha4-subunit are critical for the formation of a functional heterodimer. J. Biol. Chem. 273, 6786–6795 (1998).
DeNucci, C.C., Pagan, A.J., Mitchell, J.S. & Shimizu, Y. Control of alpha4beta7 integrin expression and CD4 T cell homing by the beta1 integrin subunit. J. Immunol. 184, 2458–2467 (2010).
Nakamura, K. et al. TGF-beta 1 plays an important role in the mechanism of CD4+CD25+ regulatory T cell activity in both humans and mice. J. Immunol. 172, 834–842 (2004).
Guagnozzi, D. & Caprilli, R. Natalizumab in the treatment of Crohn's disease. Biologics 2, 275–284 (2008).
Stefanelli, T., Malesci, A., De La Rue, S.A. & Danese, S. Anti-adhesion molecule therapies in inflammatory bowel disease: touch and go. Autoimmun. Rev. 7, 364–369 (2008).
Berger, J.R. & Koralnik, I.J. Progressive multifocal leukoencephalopathy and natalizumab--unforeseen consequences. N. Engl. J. Med. 353, 414–416 (2005).
Kleinschmidt-DeMasters, B.K. & Tyler, K.L. Progressive multifocal leukoencephalopathy complicating treatment with natalizumab and interferon beta-1a for multiple sclerosis. N. Engl. J. Med. 353, 369–374 (2005).
Keusch, G.T. Micronutrients and susceptibility to infection. Ann. NY Acad. Sci. 587, 181–188 (1990).
Schweigert, F.J. Inflammation-induced changes in the nutritional biomarkers serum retinol and carotenoids. Curr. Opin. Clin. Nutr. Metab. Care 4, 477–481 (2001).
Uehara, S., Grinberg, A., Farber, J.M. & Love, P.E. A role for CCR9 in T lymphocyte development and migration. J. Immunol. 168, 2811–2819 (2002).
Kang, S.G., Wang, C., Matsumoto, S. & Kim, C.H. High and low vitamin A therapies induce distinct FoxP3+ T-cell subsets and effectively control intestinal inflammation. Gastroenterology 137, 1391–1402 e1391–1396 (2009).
Kang, S.G. et al. Identification of a chemokine network that recruits FoxP3(+) regulatory T cells into chronically inflamed intestine. Gastroenterology 132, 966–981 (2007).
Acknowledgements
We thank J.S. Chang, J.H. Lee, and C.W. Wang (Purdue University) for their helpful inputs and A. Feil for her excellent service with microarray hybridization and scanning (Purdue Genomics Core Facility). This study was supported, in part, by grants from NIH (1R01AI074745, 1R56AI080769, and 1R01DK076616) and Crohn's and Colitis Foundation of America to C.H.K.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declared no conflict of interest.
Additional information
SUPPLEMENTARY MATERIAL is linked to the online version of the paper
Supplementary information
Rights and permissions
About this article
Cite this article
Kang, S., Park, J., Cho, J. et al. Complementary roles of retinoic acid and TGF-β1 in coordinated expression of mucosal integrins by T cells. Mucosal Immunol 4, 66–82 (2011). https://doi.org/10.1038/mi.2010.42
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mi.2010.42
This article is cited by
-
Fat-soluble vitamins: updated review of their role and orchestration in human nutrition throughout life cycle with sex differences
Nutrition & Metabolism (2022)
-
A ligand-independent fast function of RARα promotes exit from metabolic quiescence upon T cell activation and controls T cell differentiation
Mucosal Immunology (2021)
-
Adjuvant selection regulates gut migration and phenotypic diversity of antigen-specific CD4+ T cells following parenteral immunization
Mucosal Immunology (2018)
-
Vitamin A and D in allergy: from experimental animal models and cellular studies to human disease
Allergo Journal (2018)
-
Vitamin A and D in allergy: from experimental animal models and cellular studies to human disease
Allergo Journal International (2018)