Abstract
Treatment for chronic myeloid leukemia (CML) has evolved from chemotherapy (busulfan, hydroxyurea) to interferon-α (IFNα), and finally to tyrosine kinase inhibitors such as imatinib. Although imatinib has profoundly improved outcomes for patients with CML, it has limitations. Most significantly, imatinib cannot eradicate CML primitive progenitors, which likely accounts for the high relapse rate when imatinib is discontinued. IFNα, unlike imatinib, preferentially targets CML stem cells. Early studies with IFNα in CML demonstrated its ability to induce cytogenetic remission. Moreover, a small percentage of patients treated with IFNα were able to sustain durable remissions after discontinuing therapy and were probably cured. The mechanisms by which IFNα exerts its antitumor activity in CML are not well understood; however, activation of leukemia-specific immunity may have a role. Some clinical studies have demonstrated that the combination of imatinib and IFNα is superior to either therapy alone, perhaps because of their different mechanisms of action. Nonetheless, the side effects of IFNα often impede its administration, especially in combination therapy. Here, we review the role of IFNα in CML treatment and the recent developments that have renewed interest in this once standard therapy for patients with CML.
Similar content being viewed by others
Introduction to chronic myeloid leukemia
Chronic myeloid leukemia (CML) is characterized by excessive myeloid proliferation and a recurrent cytogenetic abnormality known as the Philadelphia chromosome (Ph). The abnormality results from a balanced translocation between chromosomes 9 and 22, t(9;22)(q34; q11.2), which fuses the breakpoint cluster region (BCR) gene on chromosome 22 to the ABL gene on chromosome 9.1, 2 The resultant BCR-ABL oncogene encodes a constitutively active fusion BCR-ABL p210 oncoprotein. The activity of BCR-ABL is central to the pathogenesis of CML because it alters the proliferation, natural death processes and migration of the neoplastic cells.3, 4, 5 As a consequence, the leukemic clone gradually replaces normal hematopoiesis. Residual normal hematopoiesis is present in the vast majority of patients with CML, but since it is suppressed, most of the blood cells are Ph+.
Overview of treatments for CML
Until the early 1980s, CML therapy was based on busulfan or hydroxyurea, which had a negligible effect on the natural course of the disease. Talpaz et al.6, 7 carried out the first pilot clinical trial of partially pure IFNα for the management of CML followed by a larger study. The pivotal finding was that IFNα induced cytogenetic responses, which were more durable and reproducible than those induced by chemotherapy. Although initially used in the partially pure form, recombinant forms—α2a (Hoffman La Roche, Basel, Switzerland) and α2b (Merck & Co. Inc. (formerly Schering Plough), Whitehouse Station, NJ, USA)—became the dominant IFNs used in clinical studies at doses similar to those used with partially pure IFNα (that is, 2–5 MU/m2 daily). Recombinant IFNα therapy achieved response rates similar to those observed with the purified human product.8, 9, 10, 11, 12, 13 Results from over 1500 randomized patients demonstrated that although both IFNα and chemotherapy (hydroxyurea or busulfan) could induce hematological responses in CML, IFNα significantly improved patient survival, with a 5-year survival rate of 50–59% compared with 29–44% for patients receiving busulfan or hydroxyurea.14, 15, 16, 17, 18 In a study of 1303 IFN-treated patients, median survival was 8.2 years for low-risk patients, 5.4 years for intermediate-risk patients and 3.5 years for high-risk patients.19 The studies of single-agent IFNα are summarized in Table 1. In an effort to improve outcomes, IFNα was also combined with chemotherapeutic agents, such as cytarabine, hydroxyurea and busulfan, and even with intensive chemotherapy regimens (Table 2).20, 21, 22, 23, 24, 25, 26, 27, 28 With the exception of cytarabine, the combination therapies were not usually superior to IFNα alone.
To improve its pharmacokinetic characteristics, IFNα has been attached to polyethylene glycol, which protects it from proteolytic breakdown. The resulting pegylated IFNα (PegIFNα) has been approved for the treatment of chronic hepatitis B and C and melanoma. In addition, a phase I trial evaluated escalating doses of PegIFNα-2a±cytarabine in patients with IFNα-resistant chronic phase CML (CML-CP).29 Dose-limiting toxicity was not observed at the highest dose of 630 μg per week. The safety profile of PegIFNα was similar to that of unmodified IFNα. While phase I trials suggested that PegIFNα induced better response rates compared with the unmodified form,29, 30 randomized trials showed mixed results.31, 32
By 1990, the constitutive tyrosine kinase activity of BCR-ABL was linked to the pathogenesis of CML. This discovery spurred the development of the molecular-targeted therapy imatinib (Gleevec/Glivec; Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA), which proved selective for killing cells expressing the BCR-ABL protein.33 Clinical trials with imatinib followed and demonstrated impressive response rates in patients who had not responded to IFNα therapy. Of the patients in late CML-CP, 95% achieved a complete hematological remission (CHR), 60% a major cytogenetic response (MCyR) and 41% a complete cytogenetic response (CCyR).34, 35
Initiated in June of 2000, the phase III International Randomized Study of Interferon and STI571 (IRIS) was the first large-scale trial to compare imatinib (400 mg daily) with IFNα plus low-dose cytarabine, the standard of care at that time.36 The results in 1106 patients with newly diagnosed CML-CP demonstrated that imatinib was better tolerated and induced higher CHR and CCyR rates that resulted in longer progression-free survival than IFNα. The IRIS study did not report survival differences between the treatments because 90% of patients in the IFNα arm eventually crossed over to imatinib. However, comparison with IFNα-treated historical controls indicated a significant survival advantage with imatinib.37, 38, 39 The US Food and Drug Administration subsequently approved imatinib for the treatment of newly diagnosed patients with CML-CP. In 2010, the Food and Drug Administration approved the second-generation tyrosine kinase inhibitors (TKIs) dasatinib (100 mg daily) and nilotinib (300 mg twice daily) as front-line therapies for patients with CML-CP. Recent studies indicate that both dasatinib and nilotinib are superior to standard-dose imatinib with regard to CCyR, major molecular response (MMR), and prevention of progression to accelerated and blast phases.40, 41 Current therapeutic guidelines also recommend the use of nilotinib or dasatinib in patients intolerant or resistant to imatinib therapy and state that IFNα ‘should no longer be considered as initial therapy for CML’, but could be considered in ‘rare patients unable to tolerate imatinib, dasatinib or nilotinib’.42, 43
Another treatment option for this patient population is hematopoietic stem cell transplantation, which was introduced in the 1970s. Although associated with significant morbidity and mortality, this therapy cured a substantial percentage of the patients with CML who qualified for it. In fact, transplantation is still perceived as the only curative treatment for CML. In 2007, the German CML Study Group conducted a randomized clinical trial comparing primary allogeneic hematopoietic stem cell transplantation with best available drug therapy (IFNα-based, but many patients were switched to imatinib over the course of the study) for patients with early CML-CP.44 For the first 8 years, the drug treatment arm demonstrated better survival curves than those of the transplant arm. Beyond 8 years, the survival curves became less distinct. These results suggested that drug therapy should serve as first-line treatment for patients with CML-CP.
Limitations of TKI treatment in CML and emerging roles for IFNα
The phenomenal outcomes of the IRIS study notwithstanding, a significant number of patients will require second-line therapy as a result of intolerance to or failure of imatinib therapy. After 8 years, 45% of patients in the IRIS trial randomized to receive imatinib were no longer receiving imatinib because of toxicity (6%), suboptimal response/failure (16%) or other reasons (23%).45 Furthermore, a small fraction of patients taking imatinib continue to progress to accelerated or blast phase every year.45
Another significant limitation of imatinib is the inability of most CML patients to discontinue therapy and maintain their remission.46 Rousselot et al.47 reported that even though disease could not be detected for a median of 32 months in 12 CML patients who received imatinib, once therapy was stopped the BCR-ABL transcript was detectable in six of the patients within 1–5 months. Furthermore, the six patients who did not immediately relapse had previously taken IFNα for 29–152 months. Other studies, including IRIS, have also demonstrated improved outcomes with imatinib in patients who received or responded to prior IFNα treatment.48, 49, 50, 51 More recently, Mahon et al.52 demonstrated that among patients who sustained a complete molecular response to imatinib for at least 2 years (a subset of patients that constitutes a minority of all treated patients), 40% did not relapse when therapy was discontinued. In a similar patient population, Ross et al.53 used highly sensitive nested quantitative polymerase chain reaction (PCR) and found that patients who maintained a complete molecular response after stopping imatinib harbored a stable level of BCR-ABL. Taken together, these results suggest that imatinib therapy can induce durable remissions in a small subset of patients with CML and that the addition of IFNα may broaden imatinib’s therapeutic potential in CML.
Evaluating therapy with IFNα
Kinetics and predictors of response to IFNα
Patients respond more quickly to imatinib than to IFNα. Patients on IFNα therapy achieve CCyR at a median time of 19 months compared with 6 months on imatinib treatment.54, 55 This variation may be because of the different mechanisms of action of the two drugs.
Response to IFNα depends on the phase and duration of CML disease. In general, IFNα therapy best benefitted patients with early-stage disease and favorable prognostic factors. A low-risk prognostic profile included <1 year since diagnosis, no peripheral blood basophilia, no additional cytogenetic abnormalities, Caucasian descent and age <60 years; such patients achieved higher hematologic and cytogenetic response rates with IFNα than their high-risk counterparts.56 In addition, patients in accelerated phase and blast crisis did not typically respond to IFNα. IFNα also had limited effects in late CML-CP.
Toxicities
Acute side effects to IFNα therapy commonly present as flu-like symptoms (anorexia, fever, chills, myalgias and headaches); these are not typically dose limiting and usually resolve in a few days. Chronic side effects include fatigue, weight loss, myalgias/arthralgias, depression and immune-mediated complications, such as autoimmune hemolytic anemia/thrombocytopenia, collagen vascular disorders, hypothyroidism and immune-mediated nephritic syndrome. Cases of cardiac dysfunction, including dysrhythmias and congestive heart failure, are rare but require immediate discontinuation of IFNα. Chronic fatigue and neurotoxicity, such as depression and cognitive impairment, are common dose-limiting side effects and typically worsen with continued treatment.57 As these toxicities have hindered compliance with therapy, three joint prospective studies examined whether a lower dose of IFNα at 3 MU/m2 five times a week would be as effective as the standard dose of 5 MU/m2 daily.58 The studies found that overall survival and response rates did not dramatically differ between groups.
Significance of cytogenetic responses to IFNα
The critical finding of the IFNα trials was the correlation between cytogenetic response and survival. IFNα treatment led to MCyR in 10–40% of patients and CCyR in 5–30% of patients.28, 59 A group of European investigators created a registry of 317 patients with CML in CCyR after starting IFNα alone or with hydroxyurea.54 The median time to first CCyR was 19 months. After 10 years, 72% of these patients were alive and 46% were in continuous CCyR. Similarly, Kantarjian et al.60 analyzed the long-term significance of cytogenetic responses to IFNα-based therapies. Of the 512 patients in early chronic phase, 27% achieved a CCyR within a median time of 16 months. These responders had a survival rate of 78% at a median follow-up of 127+ months (range, 88+ to 191+ months). The induced CCyR was durable; patients who maintained cytogenetic remission for more than 2 years on IFNα therapy remained in remission for an average of 6 years after discontinuing treatment. These results, along with an additional study,61 confirmed that CCyR predicts long-term survival in patients with CML and that IFNα can induce stable remissions in some patients with CML.
IFNα mechanisms of action in CML
Although IFNα has been around for many years, we still do not know how it exerts its antileukemic effects. According to in vitro studies, IFNα modulates gene expression, promotes cell differentiation and apoptosis, directly inhibits cell growth and proliferation, restores regulation by the bone marrow microenvironment and induces an immunomodulatory response. Microarray analyses have shown that IFNα can induce expression of over 300 different genes.62 These genes encode apoptotic proteins (i.e., TRAIL, Fas, caspase-4, caspase-8 and XAF-1), anti-viral proteins (that is, PKR, 2′5′A oligoadenylate synthetase and Mx proteins), immunomodulatory proteins (that is, MHC I and II, LMP-2 and C1 inhibitor), host defense proteins (that is, PKR, IRF 1–9, interleukin-15 and interleukin-6) and transcription factors (that is, signal transducer and activator of transcription 1, signal transducer and activator of transcription 2, ISGF3-γ and IRF1–7).63 The precise function of many of the gene products induced by IFNα remains unknown; however, several of the identified genes encode well-known pro-apoptotic proteins, including TRAIL/Apo2L and Fas/CD95.63 In CML progenitor cells, IFNα enhances the expression of the Fas receptor, thereby increasing cell sensitivity to Fas ligand.64 In addition to activating apoptosis, IFNα directly targets key regulators of the cell cycle, including retinoblastoma protein, cdc25A, cyclins (cyclin D3, cyclin E and cyclin A) and cyclin-dependent kinases (cdk4 and cdk6). Such targeting can block and/or lengthen the cell cycle phases, allowing cells to differentiate or undergo apoptosis.65, 66
In bone marrow hematopoietic progenitors, IFNα directly inhibits proliferation by suppressing the production of hematopoietic stimulatory cytokines, such as granulocyte–macrophage colony-stimulating factor and interleukin-1β. It also increases the synthesis of inhibitory cytokines, including interleukin-1 receptor antagonist and transforming growth factor-β.67 In addition, IFNα may inhibit the proliferation of CML progenitors by restoring normal hematopoietic mechanisms. In normal progenitors, β1-integrin receptors mediate cell adhesion to the bone marrow stroma, and stimulation of these receptors transmits antiproliferation signals. These two regulatory mechanisms are defective in CML progenitors, but Bhatia et al.68 have shown that IFNα can restore them. Lastly, the growth-inhibitory effects of IFNα seem to require activation of the mitogen-activated protein kinase p38 in CML progenitors.69, 70 IFNα treatment activates p38 by phosphorylation, which in turn leads to the transcription of IFNα-inducible genes.
In addition to directly inhibiting cell proliferation, IFNα may attenuate CML by activating host immune cells, including B and T lymphocytes, natural killer cells and antigen-presenting dendritic cells.71, 72, 73, 74 The increased incidence of immune-mediated complications with IFNα therapy supports such immune activation.75 Addition of IFNα both in vitro and in vivo caused CML mononuclear cells to differentiate into dendritic cells; the dendritic cells then served as antigen-presenting cells for CML-specific peptides.76 Similarly, in the presence of IFNα and granulocyte–macrophage colony-stimulating factor in vitro, CML bone marrow mononuclear cells differentiated into dendritic cells with specific antileukemia function.74 This may have clinical relevance because addition of granulocyte–macrophage colony-stimulating factor to treatment with IFNα in patients who failed to achieve an MCyR (n=14) improved cytogenetic responses for half of the patients.77 Lastly, IFNα (but not imatinib) induces cytotoxic T cells (CTLs) specific for CML progenitors.78
Given the potential benefits of combination therapy with imatinib and IFNα, a recent study investigated the effect of BCR-ABL signaling on IFNα activity in a CML cell line.79 The study showed that expression of BCR-ABL in non-CML cells attenuated IFN signaling; however, pre-treatment of CML cells with imatinib augmented the antigrowth effects of IFNα exposure. In addition, imatinib pre-treatment enhanced signal transducer and activator of transcription 1 phosphorylation induced by IFNα. These results, in addition to providing insights into the mechanism of action of the combination therapy, may translate into a clinical strategy to increase the sensitivity of CML cells to IFNα.
Using minimal residual disease to determine treatment plan
With the introduction of reverse transcriptase-polymerase chain reaction (RT–PCR) analysis, residual leukemic clones could be detected in patients thought to be in complete remission. In fact, RT–PCR is sensitive enough to detect one BCR-ABL+ cell per 1 × 105–1 × 106 normal cells.80, 81, 82 Lee et al.83 demonstrated that all 29 patients with a CCyR to IFNα harbored some residual Ph+ cells. Even so, 21 of the patients maintained their CCyR at a median follow-up of 13 months after RT–PCR analysis. These findings suggested that PCR positivity for BCR-ABL does not predict immediate disease relapse. A clinical trial with longer follow-up of IFNα treatment revealed that cytogenetic remission can last for years, even when MRD resides in the early hematopoietic progenitor cells of patients with CML.84 One explanation is that IFNα puts tumor cells in a dormant state, which prevents residual leukemia cells from regenerating clinically significant leukemia.
Regardless of how remission is maintained in the presence of residual disease, the studies evaluating RT–PCR analysis raised the following two questions: (1) how long should patients continue IFNα therapy once they achieve a CCyR, and (2) can RT–PCR analysis guide the decision to discontinue therapy? To address these questions, Hochhaus et al.85 continuously monitored BCR-ABL transcript levels by RT–PCR in 54 patients who were treated with IFNα and achieved CCyR. Over a median observation period of 1.9 years, the 14 patients who relapsed demonstrated a significantly higher median BCR-ABL:ABL ratio than those who maintained a CCyR (0.49% vs 0.021%; P<0.0001). These findings suggested that the degree of residual disease could predict the probability of relapse. When IFNα was withdrawn in six of the patients, one patient relapsed and was subsequently found to possess increasing levels of MRD; thus, the authors advised that IFNα be continued at least until low levels of BCR-ABL transcripts were achieved.
The IRIS trial was the first randomized trial to evaluate molecular disease by RT–PCR in patients with CML. The results showed that BCR-ABL transcript levels fell by 3 log or greater (defined as MMR) in 57% of patients with a CCyR after 12 months of imatinib treatment. In comparison, only 24% of patients with a CCyR in the IFNα group had at least a 3-log reduction in BCR-ABL transcripts.86 Importantly, all patients who achieved an MMR remained progression free at the 24-month follow-up. A long-term follow-up of the IRIS trial examined patients who achieved a CCyR with imatinib (163 out of 553 patients at 18-month follow-up).87 Of these patients, 127 achieved an MMR by 18 months and none had CML progression at the 84-month follow-up.87 The authors concluded that once a CCyR was reached, RT–PCR assessment of molecular disease could replace cytogenetic analysis of patient response. In support of this, Kantarjian et al.60 reported that all 20 patients with persistent PCR-negative CML-CP maintained an MCyR at the last long-term follow-up 10 years from the first CCyR. Altogether, these studies validated molecular testing in CML and redefined how clinicians should measure patient responses and predict clinical outcomes.
To determine whether patients with sustained undetectable BCR-ABL transcript levels were fully cured or continued to generate leukemic stem cells in their bone marrow, a recent study was conducted in patients who achieved undetected MRD for >3 years with IFNα (n=3), imatinib after IFNα failure (n=2) or dasatinib after imatinib intolerance (n=1).88 In all patients, leukemic stem cells expressing BCR-ABL were identified. At this time, whether undetected MRD correlates with risk of disease relapse is not known and warrants further investigation.
Potential re-emergence of IFNα use in CML: current developments and future strategies
Durable responses after discontinuation of IFNα
Several cases of continuous cytogenetic remission after the cessation of IFNα therapy have generated excitement about the curative potential of IFNα.61, 89 These patients usually maintained a CCyR for more than 24 months before discontinuing IFNα and maintained remission for an average of 6 years after discontinuing therapy. Outside of allogeneic hematopoietic stem cell transplantation, this represents the closest evidence of a clinical ‘cure’ for CML. Note that only approximately 20% of patients who receive IFNα achieve a durable CCyR, but those who reach this milestone demonstrate prolonged survival.
Several preclinical studies provide possible reasons why imatinib may not be sufficient to cure CML. First, primitive CML cells/leukemic stem cells do not readily undergo apoptosis when exposed to imatinib, even after prolonged exposure.90, 91 Second, CML early progenitor/stem cells persist in patients who achieve a CCyR with imatinib.92 Thus, since imatinib does not eliminate the malignant progenitors that cause the disease, it is probably not curative in the majority of cases. These progenitors may escape imatinib toxicity because they do not depend on BCR-ABL mechanisms for survival and proliferation.93 In support of this, a recent in vitro study demonstrated that while imatinib does inhibit the BCR-ABL kinase and its downstream signaling in CML primitive progenitors, the drug fails to facilitate death in these cells.94 This finding implies that CML stem cells are not ‘addicted’ to the BCR-ABL oncogene.
In contrast to therapy with imatinib, evidence suggests that IFNα actually targets the residual leukemic stem cells that cause disease relapse. Short-term colony-forming and long-term culture-initiating cell assays showed that IFNα was more active against primitive CML progenitors, whereas imatinib preferentially targeted more mature, differentiated CML progenitors.95 These findings may explain why the clinical responses to IFNα are slower but more durable than those to imatinib. Imatinib acts quickly on the more differentiated progenitors that make up the bulk of the leukemia. By contrast, since IFNα targets the rare CML stem cell (<1% of the CML population), its effects may not manifest as early on in treatment. More recent data in mice have shown that IFNα administered to dormant stem cells activates and thereby sensitizes them to subsequent killing by chemotherapeutic agents.96
A small clinical trial investigating the value of prior IFNα treatment in maintaining remission after discontinuing imatinib therapy is currently ongoing (ClinicalTrials.gov, Identifier: NCT01073436).
Combining IFNα with imatinib and second-generation TKIs
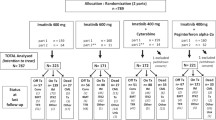
To identify optimal imatinib-based regimens for CML-CP, two large multicenter, randomized treatment optimization studies were initiated: the German CML-Study IV (imatinib 400 mg vs imatinib plus IFNα (1.5–3 MU thrice weekly) vs imatinib plus cytosine arabinoside vs imatinib after IFNα failure vs imatinib 800 mg; n=1022)97 and the French STI571 Prospective Randomized Trial (SPIRIT; imatinib 400 mg vs imatinib 600 mg vs imatinib plus cytosine arabinoside vs imatinib plus PegIFNα; n=636).98 Of note, the German CML-Study IV used IFNα, whereas the French study used PegIFNα-2a (Pegasys; Hoffmann-La Roche Inc., Nutley, NJ, USA).
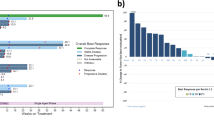
In the German CML-Study IV, recruitment to the imatinib plus cytosine arabinoside and the imatinib after IFNα failure study arms was terminated early because of feasibility and compliance issues. At 12 months, a higher rate of MMR was observed with tolerability-adapted imatinib 800 mg compared with the imatinib 400 mg±IFNα arms (P=0.003; Table 3). Significantly higher rates of CCyR were also observed with imatinib 800 mg over the first 24 months, as well as superior molecular responses at the 1, 0.1 and 0.01% BCR-ABL transcript levels according to the International Scale (IS). Treatment approaches were well tolerated with similar grade 3 and 4 adverse events. The investigators suggested that the superior remission rates in the high-dose imatinib arm were a result of the strategy applied (high dose early on and maintenance around 600 mg per day according to tolerability). The earlier and faster remissions with tolerability-adapted high-dose imatinib are expected to translate into better survival with longer follow-up.
In contrast to the German CML-Study IV, the French SPIRIT study reported significantly faster and better molecular response rates with the combination of imatinib plus PegIFNα-2a compared with imatinib alone (400 and 600 mg per day) and combined with cytarabine (Table 3).98 Specifically, the 12-, 18- and 24-month rates and cumulative incidences of major and superior (>4-log reduction in BCR-ABL:ABL transcripts) molecular responses were significantly higher in this group. Enrollment in the imatinib 600 mg and imatinib plus cytosine arabinoside arms was stopped primarily because of low rates of molecular responses and observed toxicity, respectively. Furthermore, 45% of patients discontinued PegIFNα-2a in the first year primarily because of adverse effects; however, when the dose was reduced from 90 to 45 μg per week, treatment was better tolerated. A major finding of the study was that longer duration of imatinib plus PegIFNα-2a (particularly more than 12 months) correlated with a better rate of molecular responses. However, event-free survival did not differ across all the arms of the study after 4 years of follow-up. The second part of the trial will focus on whether the earlier and faster response rates with this combination translate into better survival.
At 12-month follow-up, the incidence of MMR with imatinib 400 mg per day was 31% in CML-Study IV and 38% in SPIRIT, both of which were comparable with the 39% MMR rate observed in IRIS. In contrast, the 12-month MMR rate in the imatinib plus IFNα arm of CML-Study IV was 35% compared with 57% in the imatinib plus PegIFNα-2a arm of SPIRIT. The patient populations in the two studies were not different, and it is possible that use of the pegylated form of IFNα, which was designed to have a longer half-life in the blood, improved the efficacy of the combination in the SPIRIT trial.
Three smaller phase II studies of imatinib plus PegIFNα-2b (PegIntron; Merck) reported discordant results. The Nordic group study (n=112) compared the combination of PegIFNα-2b 50 μg per week and imatinib 400 mg per day with imatinib 400 mg per day alone in patients with low- or intermediate-risk CML.99 The MMR rate was significantly higher in the combination arm (82%) compared with the monotherapy arm (54%) at 12 months. Even a short exposure to PegIFNα-2b (3–6 months) improved response to imatinib. Notably, 34 of the 56 patients in the combination arm discontinued PegIFNα-2b, mainly owing to adverse events, such as neutropenia and constitutional symptoms. To manage adverse events, the starting dose of PegIFNα-2b (50 μg per week) was lowered to 30 μg per week. Of those who continued therapy with PegIFNα-2b for more than 12 months, 91% achieved an MMR vs 58% in the imatinib monotherapy arm. The second two-arm study (n=94) examined the addition of PegIFNα-2b (0.5 μg/kg per week) and granulocyte–macrophage colony-stimulating factor to high-dose imatinib (800 mg per day) vs the continuation of high-dose imatinib alone in patients with early CML-CP.100 Unlike the Nordic and SPIRIT trials, this study found no differences in the cytogenetic or molecular response rates between the two arms. Owing to treatment-related toxicity, the combination arm had a high dropout rate, which may have hampered potential benefits of the immunotherapy. Adherence to PegIFNα-2b was also very low (13%) in an earlier study of imatinib plus PegIFNα-2b conducted by the Italian Cooperative Study Group.101, 102 The starting doses of PegIFNα-2b (50, 100 and 150 μg per week) were likely too high in combination with imatinib, leading to grade 3 or 4 neutropenia in 63% and grade 3 or 4 non-hematologic adverse events in 52% of patients. The German, SPIRIT and Nordic studies, which used lower doses of IFNα, reported comparatively fewer grade 3 and 4 hematological and non-hematological adverse events in patients taking imatinib plus IFNα. A retrospective analysis of the Italian study showed that CCyR and MMR rates were higher in patients receiving the combination at early time points, but were comparable with the imatinib-only arm at longer times. The durability of responses, event-free survival and overall survival were also similar between the two arms.102, 103
Interestingly, the early and fast response rates with imatinib 800 mg and with imatinib plus PegIFNα are similar to those recently reported for the second-generation TKIs dasatinib41 and nilotinib.40 Studies investigating the combination of IFNα with nilotinib or dasatinib are ongoing. A phase I German study (NICOLI) is investigating the maximum-tolerated dose of low-dose IFNα in combination with nilotinib in patients with imatinib-resistant CML-CP (ClinicalTrials.gov, Identifier: NCT01220648). The phase II French NILOPEG trial (ClinicalTrials.gov, Identifier: NCT01294618) is studying the efficacy of nilotinib plus PegIFNα-2a (45 μg per week) in the first-line setting. The phase II German CML-Study V (ClinicalTrials.gov, Identifier: NCT01657604; EudraCT, Number: 2010-024262-22), which was activated in August 2012, is comparing nilotinib, nilotinib plus IFNα, maintenance with nilotinib and maintenance with IFNα (four arms). Two small phase II studies are investigating the value of adding PegIFNα-2a (45 μg per week in one study and 180 μg per week in the other) for 2 years to the treatment regimen of patients who achieved CCyR and ⩽0.5% BCR-ABL:ABL transcript with imatinib, nilotinib or dasatinib (ClinicalTrials.gov, Identifier: NCT01392170 and NCT00573378).
Value of IFNα in patients with the T315I mutation
Treatment of patients with the T315I mutation (threonine-to-isoleucine mutation at amino acid 315) in BCR-ABL is challenging, as this mutation confers resistance to treatment with imatinib, as well as second-generation TKIs. The frequency of this mutation ranges from 2–20% of imatinib-resistant CML patients. The National Comprehensive Cancer Network guidelines recommend hematopoietic stem cell transplantation, if applicable, or participation in a clinical trial for this patient population.104 Currently, a number of agents are under investigation, including ponatinib105 (a reversible Abl-Src inhibitor), DCC-2036 (a switch-pocket inhibitor) and homoharringtonine (omacetaxine).106
Although no clinical studies have investigated the value of IFNα in treating patients with the T315I mutation, two case reports have recently been published. One patient with the T315I mutation achieved a CCyR after 12 months of treatment with imatinib (400 mg per day), but developed resistance after 18 months of treatment. The patient was treated with a combination of imatinib and IFNα (6 MU per week). After 51 months of combination treatment, he achieved MMR, and the T315I mutation was not detected by direct sequencing or pyrosequencing. While the patient experienced grade 2 anemia and grade 1 neutropenia and thrombocytopenia, he could continue the treatment with no dose reduction.107 In the second case, the patient was treated with KW-2449, a T315I-specific inhibitor, after losing the CCyR induced by 800 mg per day imatinib. While KW-2449 appeared to reverse the T315I mutation, his response did not improve; furthermore, he developed the F359I mutation. On switching to combination treatment with dasatinib (50 mg twice daily) and PegIFNα (9 MU per day), the patient achieved a CCyR and an MMR with a BCR-ABL:ABL ratio of 0.05 after 4 months.108 These reports point to the potential value of IFNα in eradicating resistance to TKI treatment in the presence of the T315I mutation. More robust data are needed to confirm these treatment benefits.
Induction of CML-specific immunity by IFNα and implications for maintenance therapy
As mentioned above, IFNα is known to activate leukemia-specific immunity, but the underlying mechanism is still not well understood. One current hypothesis is based on early work by Molldrem et al.109 examining the immunogenicity of proteinase 3, a serine protease highly expressed in various myeloid leukemia cells, including CML. A peptide derived from proteinase 3 known as PR1 was identified with high affinity for HLA-A.2.1. Of significance, CTLs specific for PR1 eliminated CML progenitors, but not normal marrow cells. A subsequent investigation detected circulating PR1-specific CD8+ T cells in 11 out of 12 IFNα responders, but not in non-responders (0 of 7).73 Kanodia et al.110 recently hypothesized that IFNα induces stable remissions at least in part by increasing the expression of PR1 in CML cells. As IFNα induces the expansion of self-renewing memory CTLs specific for PR1, the PR1-expressing CML progenitors become a prime target for immune-mediated killing.110 In support of this, PR1-CTLs were found to be increased in CML patients with a CCyR after IFNα cessation. Moreover, the PR1-CTLs secreted IFNγ in response to stimulation with PR1 peptide. By contrast, PR1-CTLs from the three patients who relapsed after IFNα withdrawal lost their ability to secrete IFNγ.110 These findings suggest that loss of functional PR1-CTLs may contribute to relapse in patients with CML.
Given the potential for developing imatinib resistance and/or intolerance with continued imatinib treatment, maintenance therapy with IFNα may allow patients to discontinue imatinib by keeping CML progenitors suppressed. A recent report on the use of PegIFNα-2a maintenance after induction treatment with imatinib and PegIFNα-2a demonstrated sustained remission in 15 out of 20 CML-CP patients at a median of 2.4 years after imatinib discontinuation.111 This impressive outcome was thought to involve a T-cell response because proteinase 3 mRNA levels and frequencies of PR1-CTLs increased during maintenance therapy with IFNα. To minimize toxicity from long-term IFNα use, a later study administered PegIFNα 9 months before and 3 months after imatinib discontinuation.112 This regimen improved the remission status of 5 of the 11 patients over a median follow-up of 47 months. These studies support further exploration of the role of IFNα consolidation or maintenance therapy after TKI induction.
Optimizing therapy: early response predictors
Before the imatinib era, the Hasford or Euro score (developed from a study of 1303 IFNα-treated patients) was used to predict prognosis at diagnosis based on spleen size, percent blasts, age, platelet count, eosinophilia and basophilia.19 A new prognostic score called EUTOS (European Treatment and Outcome Study score) has since been developed to predict clinical responses to imatinib.113 The score was developed from a study of 2060 patients treated with imatinib, including imatinib at 800 mg and in combination with IFNα. Using only two variables (spleen size and basophil percentage in peripheral blood), the score discriminates between high- and low-risk groups and predicts that 34% of high-risk patients will fail to achieve CCyR. This score predicts treatment failure with better sensitivity and specificity than the Sokal or Euro scores.113
A further advance is response prediction at 3 months. CML patients at risk of progression are candidates for change of therapy, including addition of IFNα to front-line TKI treatments. Identifying patient response to a drug early on in the treatment is key for optimizing treatment protocols.114 Early response predictors for CML are summarized in Table 4. Patients who achieve a cytogenetic remission (CCyR or MCyR) or reach a BCR-ABL level of <10% (IS) after 3 months have significantly better overall survival after 5 years (95% vs 87%).55, 115, 116 This will likely replace the current definition of optimal response to imatinib at 3 months, which requires CHR and <95% Ph+ metaphases.42 For newly diagnosed patients treated with IFNα, achievement of CHR within 3 months predicted MCyR.117
Conclusions
The reduced tolerability and slower response kinetics of IFNα compared with TKIs have reduced the enthusiasm for this therapy. However, therapy with imatinib and other TKIs may be limited by drug resistance, intolerance and, when therapy is discontinued, relapse. In contrast to targeted therapies, IFNα has a broad range of therapeutic effects that may reduce the likelihood of resistance or relapse, especially when used in combination with other CML therapies. These factors along with the proven efficacy of pegylated forms of IFNα, even at low doses, have revived interest in IFNα therapy for CML.
References
Nowell PC . The minute chromosome (Phl) in chronic granulocytic leukemia. Blut 1962; 8: 65–66.
Rowley JD . Letter: a new consistent chromosomal abnormality in chronic myelogenous leukaemia identified by quinacrine fluorescence and Giemsa staining. Nature 1973; 243: 290–293.
de Klein A, van Kessel AG, Grosveld G, Bartram CR, Hagemeijer A, Bootsma D et al. A cellular oncogene is translocated to the Philadelphia chromosome in chronic myelocytic leukaemia. Nature 1982; 300: 765–767.
Heisterkamp N, Jenster G, ten Hoeve J, Zovich D, Pattengale PK, Groffen J . Acute leukaemia in bcr/abl transgenic mice. Nature 1990; 344: 251–253.
Daley GQ, Van Etten RA, Baltimore D . Induction of chronic myelogenous leukemia in mice by the P210bcr/abl gene of the Philadelphia chromosome. Science 1990; 247: 824–830.
Talpaz M, McCredie KB, Mavligit GM, Gutterman JU . Leukocyte interferon-induced myeloid cytoreduction in chronic myelogenous leukemia. Blood 1983; 62: 689–692.
Talpaz M, Kantarjian HM, McCredie KB, Keating MJ, Trujillo J, Gutterman J . Clinical investigation of human alpha interferon in chronic myelogenous leukemia. Blood 1987; 69: 1280–1288.
Talpaz M, Kantarjian H, Kurzrock R, Trujillo JM, Gutterman JU . Interferon-alpha produces sustained cytogenetic responses in chronic myelogenous leukemia. Philadelphia chromosome-positive patients. Ann Intern Med 1991; 114: 532–538.
Kantarjian HM, Deisseroth A, Kurzrock R, Estrov Z, Talpaz M . Chronic myelogenous leukemia: a concise update. Blood 1993; 82: 691–703.
Ozer H, George SL, Schiffer CA, Rao K, Rao PN, Wurster-Hill DH et al. Prolonged subcutaneous administration of recombinant alpha 2b interferon in patients with previously untreated Philadelphia chromosome-positive chronic-phase chronic myelogenous leukemia: effect on remission duration and survival: Cancer and Leukemia Group B study 8583. Blood 1993; 82: 2975–2984.
Alimena G, Morra E, Lazzarino M, Liberati AM, Montefusco E, Inverardi D et al. Interferon alpha-2b as therapy for patients with Ph'-positive chronic myelogenous leukemia. Eur J Haematol Suppl 1990; 52: 25–28.
Thaler J, Gastl G, Fluckinger T, Niederwieser D, Huber H, Seewann H et al. The Austrian Biological Response Modifier (BRM) Study Group. Treatment of chronic myelogenous leukemia with interferon alfa-2c: response rate and toxicity in a phase II multicenter study. Semin Hematol 1993; 30: 17–19.
Niederle N, Kloke O, Wandl UB, Becher R, Moritz T, Opalka B . Long-term treatment of chronic myelogenous leukemia with different interferons: results from three studies. Leuk Lymphoma 1993; 9: 111–119.
Italian Cooperative Study Group on Chronic Myeloid Leukemia. Interferon alfa-2a as compared with conventional chemotherapy for the treatment of chronic myeloid leukemia. N Engl J Med 1994; 330: 820–825.
Hehlmann R, Heimpel H, Hasford J, Kolb HJ, Pralle H, Hossfeld DK et al. The German CML Study Group. Randomized comparison of interferon-alpha with busulfan and hydroxyurea in chronic myelogenous leukemia. Blood 1994; 84: 4064–4077.
Ohnishi K, Ohno R, Tomonaga M, Kamada N, Onozawa K, Kuramoto A et al. The Kouseisho Leukemia Study Group. A randomized trial comparing interferon-alpha with busulfan for newly diagnosed chronic myelogenous leukemia in chronic phase. Blood 1995; 86: 906–916.
Allan NC, Richards SM, Shepherd PC, on behalf of the UK Medical Research Council’s Working Parties for Therapeutic Trials in Adult Leukaemia. UK Medical Research Council randomised, multicentre trial of interferon-alpha n1 for chronic myeloid leukaemia: improved survival irrespective of cytogenetic response. Lancet 1995; 345: 1392–1397.
Chronic Myeloid Leukemia Trialists’ Collaborative Group. Interferon alfa versus chemotherapy for chronic myeloid leukemia: a meta-analysis of seven randomized trials. J Natl Cancer Inst 1997; 89: 1616–1620.
Hasford J, Pfirrmann M, Hehlmann R, Allan NC, Baccarani M, Kluin-Nelemans JC et al. Writing Committee for the Collaborative CML Prognostic Factors Project Group. A new prognostic score for survival of patients with chronic myeloid leukemia treated with interferon alfa. J Natl Cancer Inst 1998; 90: 850–858.
Kantarjian HM, Talpaz M, Keating MJ, Estey EH, O’Brien S, Beran M et al. Intensive chemotherapy induction followed by interferon-alpha maintenance in patients with Philadelphia chromosome-positive chronic myelogenous leukemia. Cancer 1991; 68: 1201–1207.
Kantarjian HM, Keating MJ, Estey EH, O’Brien S, Pierce S, Beran M et al. Treatment of advanced stages of Philadelphia chromosome-positive chronic myelogenous leukemia with interferon-alpha and low-dose cytarabine. J Clin Oncol 1992; 10: 772–778.
Wetzler M, Kantarjian H, Kurzrock R, Talpaz M . Interferon-alpha therapy for chronic myelogenous leukemia. Am J Med 1995; 99: 402–411.
Hehlmann R, Berger U, Pfirrmann M, Hochhaus A, Metzgeroth G, Maywald O et al. The German CML-Study Group. Randomized comparison of interferon α and hydroxyurea with hydroxyurea monotherapy in chronic myeloid leukemia (CML-study II): prolongation of survival by the combination of interferon α and hydroxyurea. Leukemia 2003; 17: 1529–1537.
Kantarjian HM, O’Brien S, Smith TL, Rios MB, Cortes J, Beran M et al. Treatment of Philadelphia chromosome-positive early chronic phase chronic myelogenous leukemia with daily doses of interferon alpha and low-dose cytarabine. J Clin Oncol 1999; 17: 284–292.
Arthur CK, Ma DD . Combined interferon alfa-2a and cytosine arabinoside as first-line treatment for chronic myeloid leukemia. Acta Haematol 1993; 89: 15–21.
Lindauer M, Domkin D, Döhner H, Kolb HJ, Neubauer A, Huhn D et al. Efficacy and toxicity of IFN-α2b combined with cytarabine in chronic myelogenous leukaemia. Br J Haematol 1999; 106: 1013–1019.
Guilhot F, Chastang C, Michallet M, Guerci A, Harousseau JL, Maloisel F et al. for the French Chronic Myeloid Leukemia Study Group. Interferon alfa-2b combined with cytarabine versus interferon alone in chronic myelogenous leukemia. N Engl J Med 1997; 337: 223–229.
Baccarani M, Rosti G, de Vivo A, Bonifazi F, Russo D, Martinelli G et al. for the Italian Cooperative Study Group on Myeloid Leukemia. A randomized study of interferon-α versus interferon-α and low-dose arabinosyl cytosine in chronic myeloid leukemia. Blood 2002; 99: 1527–1535.
Talpaz M, Rakhit A, Rittweger K, O’Brien S, Cortes J, Fettner S et al. Phase I evaluation of a 40-kDa branched-chain long-acting pegylated IFN-α-2a with and without cytarabine in patients with chronic myelogenous leukemia. Clin Cancer Res 2005; 11: 6247–6255.
Talpaz M, O’Brien S, Rose E, Gupta S, Shan J, Cortes J et al. Phase 1 study of polyethylene glycol formulation of interferon α-2B (Schering 54031) in Philadelphia chromosome-positive chronic myelogenous leukemia. Blood 2001; 98: 1708–1713.
Lipton JH, Khoroshko N, Golenkov A, Abdulkadyrov K, Nair K, Raghunadharao D et al. on behalf of the Pegasys CML Study Group. Phase II, randomized, multicenter, comparative study of peginterferon-α-2a (40 kD) (Pegasys®) versus interferon α-2a (Roferon®-A) in patients with treatment-naïve, chronic-phase chronic myelogenous leukemia. Leuk Lymphoma 2007; 48: 497–505.
Michallet M, Maloisel F, Delain M, Hellmann A, Rosas A, Silver RT et al. for the PEG-Intron CML Study Group. Pegylated recombinant interferon alpha-2b vs recombinant interferon alpha-2b for the initial treatment of chronic-phase chronic myelogenous leukemia: a phase III study. Leukemia 2004; 18: 309–315.
Druker BJ, Tamura S, Buchdunger E, Ohno S, Segal GM, Fanning S et al. Effects of a selective inhibitor of the Abl tyrosine kinase on the growth of Bcr-Abl positive cells. Nat Med 1996; 2: 561–566.
Druker BJ, Talpaz M, Resta DJ, Peng B, Buchdunger E, Ford JM et al. Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med 2001; 344: 1031–1037.
Kantarjian H, Sawyers C, Hochhaus A, Guilhot F, Schiffer C, Gambacorti-Passerini C et al. for the International STI571 CML Study Group. Hematologic and cytogenetic responses to imatinib mesylate in chronic myelogenous leukemia. N Engl J Med 2002; 346: 645–652.
O’Brien SG, Guilhot F, Larson RA, Gathmann I, Baccarani M, Cervantes F et al. for the IRIS Investigators. Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 2003; 348: 994–1004.
Kantarjian HM, O’Brien S, Cortes J, Giles FJ, Rios MB, Shan J et al. Imatinib mesylate therapy improves survival in patients with newly diagnosed Philadelphia chromosome-positive chronic myelogenous leukemia in the chronic phase: comparison with historic data. Cancer 2003; 98: 2636–2642.
Kantarjian HM, Talpaz M, O’Brien S, Jones D, Giles F, Garcia-Manero G et al. Survival benefit with imatinib mesylate versus interferon-alpha-based regimens in newly diagnosed chronic-phase chronic myelogenous leukemia. Blood 2006; 108: 1835–1840.
Roy L, Guilhot J, Krahnke T, Guerci-Bresler A, Druker BJ, Larson RA et al. Survival advantage from imatinib compared with the combination interferon-α plus cytarabine in chronic-phase chronic myelogenous leukemia: historical comparison between two phase 3 trials. Blood 2006; 108: 1478–1484.
Saglio G, Kim DW, Issaragrisil S, le Coutre P, Etienne G, Lobo C et al. for the ENESTnd Investigators. Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med 2010; 362: 2251–2259.
Kantarjian H, Shah NP, Hochhaus A, Cortes J, Shah S, Ayala M et al. Dasatinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 2010; 362: 2260–2270.
Baccarani M, Cortes J, Pane F, Niederwieser D, Saglio G, Apperley J et al. Chronic myeloid leukemia: an update of concepts and management recommendations of European LeukemiaNet. J Clin Oncol 2009; 27: 6041–6051.
National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology: Chronic Myelogenous Leukemia. National Comprehensive Cancer Network. 2011. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp (accessed 25 August 2011).
Hehlmann R, Berger U, Pfirrmann M, Heimpel H, Hochhaus A, Hasford J et al. Drug treatment is superior to allografting as first-line therapy in chronic myeloid leukemia. Blood 2007; 109: 4686–4692.
Deininger M, O’Brien SG, Guilhot F, Goldman JM, Hochhaus A, Hughes TP et al. International randomized study of interferon vs STI571 (IRIS) 8-year follow up: sustained survival and low risk for progression or events in patients with newly diagnosed chronic myeloid leukemia in chronic phase (CML-CP) treated with imatinib. Blood 2009; 114, abstract 1126.
Cortes J, O’Brien S, Kantarjian H . Discontinuation of imatinib therapy after achieving a molecular response. Blood 2004; 104: 2204–2205.
Rousselot P, Huguet F, Rea D, Legros L, Cayuela JM, Maarek O et al. Imatinib mesylate discontinuation in patients with chronic myelogenous leukemia in complete molecular remission for more than 2 years. Blood 2007; 109: 58–60.
Guilhot F, Druker B, Larson RA, Gathmann I, So C, Waltzman R et al. High rates of durable response are achieved with imatinib after treatment with interferon alpha plus cytarabine: results from the International Randomized Study of Interferon and STI571 (IRIS) trial. Haematologica 2009; 94: 1669–1675.
Alimena G, Breccia M, Luciano L, Quarantelli F, Diverio D, Izzo B et al. Imatinib mesylate therapy in chronic myeloid leukemia patients in stable complete cytogenic response after interferon-alpha results in a very high complete molecular response rate. Leuk Res 2008; 32: 255–261.
Branford S, Hughes T, Milner A, Koelmeyer R, Schwarer A, Arthur C et al. Efficacy and safety of imatinib in patients with chronic myeloid leukemia and complete or near-complete cytogenetic response to interferon-alpha. Cancer 2007; 110: 801–808.
Takahashi N, Kyo T, Maeda Y, Sugihara T, Usuki K, Kawaguchi T et al. Discontinuation of imatinib in Japanese patients with chronic myeloid leukemia. Haematologica 2012; 97: 903–906.
Mahon FX, Réa D, Guilhot J, Guilhot F, Huguet F, Nicolini F et al. on behalf of the Intergroupe Français des Leucémies Myéloïdes Chroniques (FILMC). Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre Stop Imatinib (STIM) trial. Lancet Oncol 2010; 11: 1029–1035.
Ross DM, Branford S, Seymour JF, Schwarer AP, Arthur C, Bartley PA et al. Patients with chronic myeloid leukemia who maintain a complete molecular response after stopping imatinib treatment have evidence of persistent leukemia by DNA PCR. Leukemia 2010; 24: 1719–1724.
Bonifazi F, de Vivo A, Rosti G, Guilhot F, Guilhot J, Trabacchi E et al. for the European Study Group on Interferon in Chronic Myeloid Leukemia. Chronic myeloid leukemia and interferon-α: a study of complete cytogenetic responders. Blood 2001; 98: 3074–3081.
Jabbour E, Kantarjian H, O’Brien S, Shan J, Quintas-Cardama A, Faderl S et al. The achievement of an early complete cytogenetic response is a major determinant for outcome in patients with early chronic phase chronic myeloid leukemia treated with tyrosine kinase inhibitors. Blood 2011; 118: 4541–4546, quiz 4759.
Kantarjian HM, Smith TL, McCredie KB, Keating MJ, Walters RS, Talpaz M et al. Chronic myelogenous leukemia: a multivariate analysis of the associations of patient characteristics and therapy with survival. Blood 1985; 66: 1326–1335.
Jonasch E, Haluska FG . Interferon in oncological practice: review of interferon biology, clinical applications, and toxicities. Oncologist 2001; 6: 34–55.
Kluin-Nelemans HC, Buck G, le Cessie S, Richards S, Beverloo HB, Falkenburg JH et al. for the UK CML Working Group of NCRI and the HOVON trials group. Randomized comparison of low-dose versus high-dose interferon-alfa in chronic myeloid leukemia: prospective collaboration of 3 joint trials by the MRC and HOVON groups. Blood 2004; 103: 4408–4415.
Kantarjian HM, O’Brien S, Anderlini P, Talpaz M . Treatment of myelogenous leukemia: current status and investigational options. Blood 1996; 87: 3069–3081.
Kantarjian HM, O’Brien S, Cortes JE, Shan J, Giles FJ, Rios MB et al. Complete cytogenetic and molecular responses to interferon-alpha-based therapy for chronic myelogenous leukemia are associated with excellent long-term prognosis. Cancer 2003; 97: 1033–1041.
Mahon FX, Delbrel X, Cony-Makhoul P, Fabères C, Boiron JM, Barthe C et al. Follow-up of complete cytogenetic remission in patients with chronic myeloid leukemia after cessation of interferon alfa. J Clin Oncol 2002; 20: 214–220.
Der SD, Zhou A, Williams BR, Silverman RH . Identification of genes differentially regulated by interferon α, β, or γ using oligonucleotide arrays. Proc Natl Acad Sci USA 1998; 95: 15623–15628.
Chawla-Sarkar M, Lindner DJ, Liu YF, Williams BR, Sen GC, Silverman RH et al. Apoptosis and interferons: role of interferon-stimulated genes as mediators of apoptosis. Apoptosis 2003; 8: 237–249.
Selleri C, Sato T, Del Vecchio L, Luciano L, Barrett AJ, Rotoli B et al. Involvement of Fas-mediated apoptosis in the inhibitory effects of interferon-α in chronic myelogenous leukemia. Blood 1997; 89: 957–964.
Kumar R, Atlas I . Interferon α induces the expression of retinoblastoma gene product in human Burkitt lymphoma Daudi cells: role in growth regulation. Proc Natl Acad Sci USA 1992; 89: 6599–6603.
Subramaniam PS, Cruz PE, Hobeika AC, Johnson HM . Type I interferon induction of the Cdk-inhibitor p21WAF1 is accompanied by ordered G1 arrest, differentiation and apoptosis of the Daudi B-cell line. Oncogene 1998; 16: 1885–1890.
Peschel C, Aulitzky WE, Huber C . Influence of interferon-α on cytokine expression by the bone marrow microenvironment—impact on treatment of myeloproliferative disorders. Leuk Lymphoma 1996; 22: 129–134.
Bhatia R, Verfaillie CM . The effect of interferon-α on beta-1 integrin mediated adhesion and growth regulation in chronic myelogenous leukemia. Leuk Lymphoma 1998; 28: 241–254.
Zou X, Calame K . Signaling pathways activated by oncogenic forms of Abl tyrosine kinase. J Biol Chem 1999; 274: 18141–18144.
Mayer IA, Verma A, Grumbach IM, Uddin S, Lekmine F, Ravandi F et al. The p38 MAPK pathway mediates the growth inhibitory effects of interferon-α in BCR-ABL-expressing cells. J Biol Chem 2001; 276: 28570–28577.
Andrews DF, Singer JW, Collins SJ . Effect of recombinant α-interferon on the expression of the bcr-abl fusion gene in human chronic myelogenous human leukemia cell lines. Cancer Res 1987; 47: 6629–6632.
Yanagisawa K, Yamauchi H, Kaneko M, Kohno H, Hasegawa H, Fujita S . Suppression of cell proliferation and the expression of a bcr-abl fusion gene and apoptotic cell death in a new human chronic myelogenous leukemia cell line, KT-1, by interferon-α. Blood 1998; 91: 641–648.
Molldrem JJ, Lee PP, Wang C, Felio K, Kantarjian HM, Champlin RE et al. Evidence that specific T lymphocytes may participate in the elimination of chronic myelogenous leukemia. Nat Med 2000; 6: 1018–1023.
Weng K, Xie X, Qiu G, Gu W . Clinical reagents of GM-CSF and IFN-α induce the generation of functional chronic myeloid leukemia dendritic cells in vitro. Cytotechnology 2012; 64: 75–81.
Sacchi S, Kantarjian H, O’Brien S, Cohen PR, Pierce S, Talpaz M . Immune-mediated and unusual complications during interferon alfa therapy in chronic myelogenous leukemia. J Clin Oncol 1995; 13: 2401–2407.
Paquette RL, Hsu N, Said J, Mohammed M, Rao NP, Shih G et al. Interferon-α induces dendritic cell differentiation of CML mononuclear cells in vitro and in vivo. Leukemia 2002; 16: 1484–1489.
Cortes J, Kantarjian H, O’Brien S, Kurzrock R, Keating M, Talpaz M . GM-CSF can improve the cytogenetic response obtained with interferon-alpha therapy in patients with chronic myelogenous leukemia. Leukemia 1998; 12: 860–864.
Burchert A, Wölfl S, Schmidt M, Brendel C, Denecke B, Cai D et al. Interferon-α, but not the ABL-kinase inhibitor imatinib (STI571), induces expression of myeloblastin and a specific T-cell response in chronic myeloid leukemia. Blood 2003; 101: 259–264.
Bhattacharya S, Zheng H, Tzimas C, Carroll M, Baker DP, Fuchs SY . Bcr-abl signals to desensitize chronic myeloid leukemia cells to IFNα via accelerating the degradation of its receptor. Blood 2011; 118: 4179–4187.
Lee MS, Chang KS, Freireich EJ, Kantarjian HM, Talpaz M, Trujillo JM et al. Detection of minimal residual bcr/abl transcripts by a modified polymerase chain reaction. Blood 1988; 72: 893–897.
Lee MS, LeMaistre A, Kantarjian HM, Talpaz M, Freireich EJ, Trujillo JM et al. Detection of two alternative bcr/abl mRNA junctions and minimal residual disease in Philadelphia chromosome positive chronic myelogenous leukemia by polymerase chain reaction. Blood 1989; 73: 2165–2170.
Kawasaki ES, Clark SS, Coyne MY, Smith SD, Champlin R, Witte ON et al. Diagnosis of chronic myeloid and acute lymphocytic leukemias by detection of leukemia-specific mRNA sequences amplified in vitro. Proc Natl Acad Sci USA 1988; 85: 5698–5702.
Lee MS, Kantarjian H, Talpaz M, Freireich EJ, Deisseroth A, Trujillo JM et al. Detection of minimal residual disease by polymerase chain reaction in Philadelphia chromosome-positive chronic myelogenous leukemia following interferon therapy. Blood 1992; 79: 1920–1923.
Talpaz M, Estrov Z, Kantarjian H, Ku S, Foteh A, Kurzrock R . Persistence of dormant leukemic progenitors during interferon-induced remission in chronic myelogenous leukemia. Analysis by polymerase chain reaction of individual colonies. J Clin Invest 1994; 94: 1383–1389.
Hochhaus A, Reiter A, Saussele S, Reichert A, Emig M, Kaeda J et al. for the German CML Study Group and the UK MRC CML Study Group. Molecular heterogeneity in complete cytogenetic responders after interferon-α therapy for chronic myelogenous leukemia: low levels of minimal residual disease are associated with continuing remission. Blood 2000; 95: 62–66.
Hughes TP, Kaeda J, Branford S, Rudzki Z, Hochhaus A, Hensley ML et al. for the International Randomised Study of Interferon versus STI571 (IRIS) Study Group. Frequency of major molecular responses to imatinib or interferon alfa plus cytarabine in newly diagnosed chronic myeloid leukemia. N Engl J Med 2003; 349: 1423–1432.
Hughes TP, Hochhaus A, Branford S, Müller MC, Kaeda JS, Foroni L et al. on behalf of the IRIS investigators. Long-term prognostic significance of early molecular response to imatinib in newly diagnosed chronic myeloid leukemia: an analysis from the International Randomized Study of Interferon and STI571 (IRIS). Blood 2010; 116: 3758–3765.
Chomel JC, Bonnet ML, Sorel N, Bertrand A, Meunier MC, Fichelson S et al. Leukemic stem cell persistence in chronic myeloid leukemia patients with sustained undetectable molecular residual disease. Blood 2011; 118: 3657–3660.
Veneri D, Tecchio C, De Matteis G, Paviati E, Benati M, Franchini M et al. Long-term persistence of molecular response after discontinuation of interferon-alpha in two patients with chronic myeloid leukaemia. Blood Transfus 2012; 10: 233–234.
Graham SM, Jørgensen HG, Allan E, Pearson C, Alcorn MJ, Richmond L et al. Primitive, quiescent, Philadelphia-positive stem cells from patients with chronic myeloid leukemia are insensitive to STI571 in vitro. Blood 2002; 99: 319–325.
Copland M, Hamilton A, Elrick LJ, Baird JW, Allan EK, Jordanides N et al. Dasatinib (BMS-354825) targets an earlier progenitor population than imatinib in primary CML but does not eliminate the quiescent fraction. Blood 2006; 107: 4532–4539.
Bhatia R, Holtz M, Niu N, Gray R, Snyder DS, Sawyers CL et al. Persistence of malignant hematopoietic progenitors in chronic myelogenous leukemia patients in complete cytogenetic remission following imatinib mesylate treatment. Blood 2003; 101: 4701–4707.
Deininger M, Buchdunger E, Druker BJ . The development of imatinib as a therapeutic agent for chronic myeloid leukemia. Blood 2005; 105: 2640–2653.
Corbin AS, Agarwal A, Loriaux M, Cortes J, Deininger MW, Druker BJ . Human chronic myeloid leukemia stem cells are insensitive to imatinib despite inhibition of BCR-ABL activity. J Clin Invest 2011; 121: 396–409.
Angstreich GR, Matsui W, Huff CA, Vala MS, Barber J, Hawkins AL et al. Effects of imatinib and interferon on primitive chronic myeloid leukaemia progenitors. Br J Haematol 2005; 130: 373–381.
Essers MA, Offner S, Blanco-Bose WE, Waibler Z, Kalinke U, Duchosal MA et al. IFNα activates dormant haematopoietic stem cells in vivo. Nature 2009; 458: 904–908.
Hehlmann R, Lauseker M, Jung-Munkwitz S, Leitner A, Müller MC, Pletsch N et al. Tolerability-adapted imatinib 800 mg/d versus 400 mg/d versus 400 mg/d plus interferon-α in newly diagnosed chronic myeloid leukemia. J Clin Oncol 2011; 29: 1634–1642.
Preudhomme C, Guilhot J, Nicolini FE, Guerci-Bresler A, Rigal-Huguet F, Maloisel F et al. for the SPIRIT Investigators and France Intergroupe des Leucémies Myéloïdes Chroniques (Fi-LMC). Imatinib plus peginterferon alfa-2a in chronic myeloid leukemia. N Engl J Med 2010; 363: 2511–2521.
Simonsson B, Gedde-Dahl T, Markevärn B, Remes K, Stentoft J, Almqvist A et al. for the Nordic CML Study Group. Combination of pegylated IFN-α2b with imatinib increases molecular response rates in patients with low- or intermediate-risk chronic myeloid leukemia. Blood 2011; 118: 3228–3235.
Cortes J, Quintás-Cardama A, Jones D, Ravandi F, Garcia-Manero G, Verstovsek S et al. Immune modulation of minimal residual disease in early chronic phase chronic myelogenous leukemia: a randomized trial of frontline high-dose imatinib mesylate with or without pegylated interferon alpha-2b and granulocyte-macrophage colony-stimulating factor. Cancer 2011; 117: 572–580.
Palandri F, Iacobucci I, Castagnetti F, Testoni N, Poerio A, Amabile M et al. on behalf of the GIMEMA Working Party on CML. Front-line treatment of Philadelphia positive chronic myeloid leukemia with imatinib and interferon-α: 5-year outcome. Haematologica 2008; 93: 770–774.
Baccarani M, Martinelli G, Rosti G, Trabacchi E, Testoni N, Bassi S et al. for the GIMEMA Working Party on Chronic Myeloid Leukemia. Imatinib and pegylated human recombinant interferon-α2b in early chronic-phase chronic myeloid leukemia. Blood 2004; 104: 4245–4251.
Palandri F, Castagnetti F, Iacobucci I, Martinelli G, Amabile M, Gugliotta G et al. The response to imatinib and interferon-α is more rapid than the response to imatinib alone: a retrospective analysis of 495 Philadelphia-positive chronic myeloid leukemia patients in early chronic phase. Haematologica 2010; 95: 1415–1419.
National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology: Chronic Myelogenous Leukemia, version 2.2012. National Comprehensive Cancer Network 2012. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp (accessed 4 May 2012).
Cortes JE, Kantarjian H, Shah NP, Bixby D, Mauro MJ, Flinn I et al. Ponatinib in refractory Philadelphia chromosome-positive leukemias. N Engl J Med 2012; 367: 2075–2088.
Burke AC, Swords RT, Kelly K, Giles FJ . Current status of agents active against the T315I chronic myeloid leukemia phenotype. Expert Opin Emerg Drugs 2011; 16: 85–103.
Itonaga H, Tsushima H, Hata T, Matsuo E, Imanishi D, Imaizumi Y et al. Successful treatment of a chronic-phase T-315I-mutated chronic myelogenous leukemia patient with a combination of imatinib and interferon-alfa. Int J Hematol 2012; 95: 209–213.
Cornelison AM, Welch MA, Koller C, Jabbour E . Dasatinib combined with interferon-alfa induces a complete cytogenetic response and major molecular response in a patient with chronic myelogenous leukemia harboring the T315I BCR-ABL1 mutation. Clin Lymphoma Myeloma Leuk 2011; 11: S111–S113.
Molldrem J, Dermime S, Parker K, Jiang YZ, Mavroudis D, Hensel N et al. Targeted T-cell therapy for human leukemia: cytotoxic T lymphocytes specific for a peptide derived from proteinase 3 preferentially lyse human myeloid leukemia cells. Blood 1996; 88: 2450–2457.
Kanodia S, Wieder E, Lu S, Talpaz M, Alatrash G, Clise-Dwyer K et al. PR1-specific T cells are associated with unmaintained cytogenetic remission of chronic myelogenous leukemia after interferon withdrawal. PLoS One 2010; 5: e11770.
Burchert A, Müller MC, Kostrewa P, Erben P, Bostel T, Liebler S et al. Sustained molecular response with interferon alfa maintenance after induction therapy with imatinib plus interferon alfa in patients with chronic myeloid leukemia. J Clin Oncol 2010; 28: 1429–1435.
Hardan I, Stanevsky A, Volchek Y, Tohami T, Amariglio N, Trakhtenbrot L et al. Treatment with interferon alpha prior to discontinuation of imatinib in patients with chronic myeloid leukemia. Cytokine 2012; 57: 290–293.
Hasford J, Baccarani M, Hoffmann V, Guilhot J, Saussele S, Rosti G et al. Predicting complete cytogenetic response and subsequent progression-free survival in 2060 patients with CML on imatinib treatment: the EUTOS score. Blood 2011; 118: 686–692.
Müller MC, Cross NC, Erben P, Schenk T, Hanfstein B, Ernst T et al. Harmonization of molecular monitoring of CML therapy in Europe. Leukemia 2009; 23: 1957–1963.
Hanfstein B, Müller MC, Hehlmann R, Erben P, Lauseker M, Fabarius A et al. Early molecular and cytogenetic response is predictive for long-term progression-free and overall survival in chronic myeloid leukemia (CML). Leukemia 2012; 26: 2096–2102.
Marin D, Ibrahim AR, Lucas C, Gerrard G, Wang L, Szydlo RM et al. Assessment of BCR-ABL1 transcript levels at 3 months is the only requirement for predicting outcome for patients with chronic myeloid leukemia treated with tyrosine kinase inhibitors. J Clin Oncol 2012; 30: 232–238.
Mahon FX, Fabères C, Pueyo S, Cony-Makhoul P, Salmi R, Boiron JM et al. Response at three months is a good predictive factor for newly diagnosed chronic myeloid leukemia patients treated by recombinant interferon-α. Blood 1998; 92: 4059–4065.
Fabarius A, Leitner A, Hochhaus A, Müller MC, Hanfstein B, Haferlach C et al. for the Schweizerische Arbeitsgemeinschaft für Klinische Krebsforschung (SAKK) and the German CML Study Group. Impact of additional cytogenetic aberrations at diagnosis on prognosis of CML: long-term observation of 1151 patients from the randomized CML Study IV. Blood 2011; 118: 6760–6768.
Acknowledgements
Editorial assistance was provided by Meenakshi Subramanian, PhD, CMPP, of Evidence Scientific Solutions, and funded by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co. Inc., Whitehouse Station, NJ, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
JC is a consultant for and has received research funding from BMS, Novartis, Ariad and Chemgenex. MT has chaired a satellite symposium for Merck and has received drugs from Merck for clinical studies. The remaining authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Talpaz, M., Hehlmann, R., Quintás-Cardama, A. et al. Re-emergence of interferon-α in the treatment of chronic myeloid leukemia. Leukemia 27, 803–812 (2013). https://doi.org/10.1038/leu.2012.313
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2012.313
Keywords
This article is cited by
-
Nanotechnology in leukemia: diagnosis, efficient-targeted drug delivery, and clinical trials
European Journal of Medical Research (2023)
-
Control of Ph+ and additional chromosomal abnormalities in chronic myeloid leukemia by tyrosine kinase inhibitors
Medical Oncology (2023)
-
The HSP90 inhibitor KW-2478 depletes the malignancy of BCR/ABL and overcomes the imatinib-resistance caused by BCR/ABL amplification
Experimental Hematology & Oncology (2022)
-
Compromised anti-tumor–immune features of myeloid cell components in chronic myeloid leukemia patients
Scientific Reports (2021)
-
Improving outcomes in chronic myeloid leukemia through harnessing the immunological landscape
Leukemia (2021)