Abstract
Objective:
Examine how pediatric and obstetrical subspecialists view benefits and burdens of prenatal myelomeningocele (MMC) closure.
Study design:
Mail survey of 1200 neonatologists, pediatric surgeons and maternal–fetal medicine specialists (MFMs).
Results:
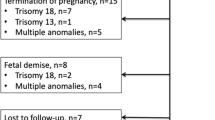
Of 1176 eligible physicians, 670 (57%) responded. Most respondents disagreed (68%, 11% strongly) that open fetal surgery places an unacceptable burden on women and their families. Most agreed (65%, 10% strongly) that denying the benefits of open maternal–fetal surgery is unfair to the future child. Most (94%) would recommend prenatal fetoscopic over open or postnatal MMC closure for a hypothetical fetoscopic technique that had similar shunt rates (40%) but decreased maternal morbidity. When the hypothetical shunt rate for fetoscopy was increased to 60%, physicians were split (49% fetoscopy versus 45% open). Views about burdens and fairness correlated with the likelihood of recommending postnatal or fetoscopic over open closure.
Conclusion:
Individual and specialty-specific values may influence recommendations about prenatal surgery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Liley AW . Intrauterine transfusion of foetus in haemolytic disease. Brit Med J 1963; 2 (5365): 1107–1109.
Harrison MR, Golbus MS, Filly RA . Management of the fetus with a correctable congenital defect. JAMA 1981; 246: 774–777.
Smajdor A . Ethical challenges in fetal surgery. J Med Ethics 2011; 37 (2): 88–91.
Flake AW . Prenatal intervention: ethical considerations for life-threatening and non-life threatening anomalies. Semin Pediatr Surg 2001; 10 (4): 212–221.
Meuli M, Meuli-Simmen C, Hutchins GM, Yingling CD . In utero surgery rescues neurological function at birth in sheep with spina bifida. Nat Med 1995; 1 (4): 342–347.
Adzick NS, Sutton LN, Crombleholme TM, Flake AW . Successful fetal surgery for spinabifida. Lancet 1998; 352 (9141): 1675–1676.
Tulipan N, Hernanz-Schulman M, Bruner JP . Reduced hindbrain herniation after intrauterine myelomeningocele repair: a report of four cases. Pediatr Neurosurg 1998; 29 (5): 274–278.
Bruner JP, Tulipan N, Paschall RL, Boehm FH, Walsh WF, Silva SR et al. Fetal surgery formyelomeningocele and the incidence of shunt-dependent hydrocephalus. JAMA 1999; 282 (19): 1819–1825.
Sutton LN, Adzick NS, Bilaniuk LT, Johnson MP, Crombleholme TM, Flake AW . Improvement in hindbrain herniation demonstrated by serial fetal magnetic resonance imagingfollowing fetal surgery for myelomeningocele. JAMA 1999; 282 (19): 1826–1831.
Copp AJ, Adzick NS, Chitty LS, Fletcher JM, Holmbeck GN, Shaw GM . Spina bifida. Nat Rev Dis Primers 2015; 1: 1–18.
Simpson JL . Fetal surgery for myelomeningocele: promise, progress, and problems. JAMA 1999; 282: 1873–1874.
Adzick NS . Fetal surgery for myelomeningocele: trials and tribulations Isabella Forshall Lecture. J Pediatr Surg 2012; ; 47 (2): 273–281.
Adzick NS, Thom EA, Spong CY, Brock JW, Burrows PK, Johnson MP et al. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med 2011; 364 (11): 993–1004.
Bruner JP, Tulipan NB, Richards WO . Endoscopic coverage of fetal open myelomeningocele in utero. Am J Obstet Gynecol 1997; 176: 256–257.
Kohl T . Percutaneous minimally invasive fetoscopic surgery for spina bifida aperta. Part I:surgical technique and perioperative outcome. Ultrasound Obstet Gynecol 2014; 44: 515–524.
Degenhardt J, Schurg R, Winarno A, Oehmke F, Khaleeva A, Kawecki A et al. Percutaneous minimal-access fetoscopic surgery for spina bifida aperta. Part II: maternal management and outcome. Ultrasound Obstet Gynecol 2014; 44: 525–531.
Pedreira DA, Zanon N, Nishikuni K, Moreira de Sá RA, Acacio GL, Chmait RH et al. Endoscopic surgery for the antenatal treatment of myelomeningocele: the CECAM trial. Am J Obstet Gynecol 2016; 214 (1): 111.e1.
Brown SD, Lyerly AD, Little MO, Lantos JD . Paediatrics-based fetal care: unanswered ethical questions. Acta Paediatr 2008; 97 (12): 1617–1619.
Dillman D, Smyth J, Christian L Internet, Mail, and Mixed-Mode Surveys: The Tailored Design Method, 3rd edn. John Wiley & Sons: Hoboken, NJ, USA, 2009.
American Association for Public Opinion ResearchStandard Definitions: Final Dispositionsof Case Codes and Outcome Rates for Surveys, 7th edn. AAPOR: Lenexa, KS, USA, 2011.
American College of Obstetricians and Gynecologists, Committee on Ethics, American Academy of Pediatrics, Committee on Bioethics. Maternal–fetal intervention and fetal care centers. Pediatrics 2011; 128 (2): e473–e478.
Flake A . Percutaneous minimal-access fetoscopic surgery for myelomeningocele - not so minimal!. Ultrasound Obstet Gynecol 2014; 44 (5): 499–500.
Brown SD, Feudtner C, Truog RD . Prenatal decision-making for myelomeningocele: can we minimize bias and variability? Pediatrics 2015; 136 (3): 409–411.
Acknowledgements
Funding was provided by a grant from the Greenwall Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Antiel, R., Collura, C., Flake, A. et al. Physician views regarding the benefits and burdens of prenatal surgery for myelomeningocele. J Perinatol 37, 994–998 (2017). https://doi.org/10.1038/jp.2017.75
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.75
This article is cited by
-
Why Are There So Few Ethics Consults in Children’s Hospitals?
HEC Forum (2018)