Abstract
Objective:
Post-hemorrhagic hydrocephalus (PHH) is associated with morbidity and mortality among very low birth weight (VLBW) infants. This study aimed to determine risk factors for PHH among VLBW infants with peri-intraventricular hemorrhage (PIVH).
Study Design:
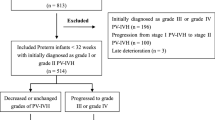
This is a population-based cohort of VLBW infants of 24 to 28 weeks gestation, born in Israel from 1995 to 2012. Infants in whom a brain ultrasound was not performed before 28 days or with major congenital malformations were excluded. Univariate and multivariable analyses identified risk factors associated with PHH.
Results:
The final study cohort comprised 2811 infants with grade 2 or higher PIVH, of whom 610 (21.7%) developed PHH. PHH was independently associated with PIVH severity, with bilateral grade 3 PIVH and PIVH grade 3 and contralateral grade 4 having the highest risks (odds ratio (OR) 12.2, 95% confidence interval (CI) 8.56 to 17.4 and OR 13.7, 95% CI 9.4 to 20.1, respectively). Unilateral grade 3 or 4 PIVH's had moderately increased risks of PHH (OR 3.50, 95% CI 2.26 to 5.42 and OR 3.79, 95% CI 2.35 to 6.12, respectively). PHH was independently associated with increasing gestational age (GA) and with neonatal morbidities including patent ductus arteriosus (OR 1.47, 95% CI 1.15 to 1.88 if medically treated and OR 3.01, 95% CI 2.11 to 4.29 if surgically treated), sepsis (OR 1.79, 95% CI 1.44 to 2.22) and necrotizing enterocolitis (OR 1.60, 95% CI 1.18 to 2.17).
Conclusions:
Among VLBW infants with PIVH, PHH was independently associated with PIVH severity group, increasing GA and acute neonatal morbidities. Unilateral grade 3 or 4 PIVH was associated with a moderate risk of developing PHH compared with bilateral severe hemorrhages.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Goldstein RF, Cotton CM, Shankaran SM, Gantz MG, Poole WK . Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Influence of gestational age on death and neurodevelopmental outcome in premature infants with severe intracranial hemorrhage. J Perinatol 2013; 33 (1): 25–32.
Bassan H, Limperopoulus C, Visconti K, Mayer DL, Feldman HA, Avery L et al. Neurodevelopmental outcome in survivors of periventricular hemorrhagic infarction. Pediatrics 2007; 120 (4): 785–792.
Hack M, Taylor HG . Perinatal brain injury in preterm infants and later neurobehavioural function. JAMA 2000; 284 (15): 1973–1974.
Maitre NL, Marshall DD, Price WA, Slaughter JC, O'Shea TM, Maxfield C et al. Neurodevelopmental outcome of infants with unilateral or bilateral periventricular hemorrhagic infarction. Pediatrics 2009; 124 (6): e1153–e1160.
Bassan H . Intracranial hemorrhage in the preterm infant: understanding it, preventing it. Clin Perinatol 2009; 36 (4): 737–762.
Horbar JD, Badger GJ, Carpenter JH, Fanaroff AA, Kilpatrick S, LaCorte M et al. Trends in mortality and morbidity for very low birth weight infants. 1991-1999. Pediatrics 2002; 110 (1 Pt 1): 143–151.
Luque MJ, Tapia JL, Villarroel L, Marshall G, Musante G, Carlo W et al. A risk prediction model for severe intraventricular hemorrhage in very low birth weight infants and the effect of prophylactic indomethacin. J Perinatol 2014; 34: 43–48.
Brouwer AJ, Groenendaal F, Benders MJNL, De Vries LS . Early and late complications of germinal matrix-intraventricular hemorrhage in the preterm infant: what is new? Neonatology 2014; 106: 296–303.
McCrea HJ, Ment LR . The diagnosis, management, and postnatal prevention of intraventricular hemorrhage in the preterm neonate. Clin Perinatol 2008; 35 (4): 772–792.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010; 126 (3): 442–458.
Shooman D, Portess H, Sparrow O . A review of the current treatment methods for posthaemorrhagic hydrocephalus of infants. Cerebrospinal Fluid Res 2009; 6: 1.
Cherian S, Whitelaw A, Thoresen M, Love S . The pathogenesis of neonatal post-hemorrhagic hydrocephalus. Brain Pathol 2004; 14: 305–311.
Whitelaw A, Jary S, Kmita G, Wroblewska J, Musialik-Swietlinska E, Mandera M et al. Randomized trial of drainage, irrigation and fibrinolytic therapy for premature infants with posthemorrhagic ventricular dilatation: developmental outcome at 2 years. Pediatrics 2010; 125: 852–858.
Robinson S . Neonatal posthemorrhagic hydrocephalus from prematurity: pathophysiology and current treatment concepts. J Neurosurg Pediatr 2012; 9: 242–258.
Linder N, Haskin O, Levit O, Klinger G, Prince T, Naor N et al. Risk factors for intraventricular hemorrhage in very low birth weight premature infants – a retrospective case control study. Pediatrics 2003; 111: e590–e595.
Weintraub Z, Solovechick M, Reichman B, Rotschild A, Waisman D, Davkin O et al. and the Israel Neonatal Network. Effect of maternal tocolysis on the incidence of severe periventricular/intraventricular haemorrhage in very low birthweight infants. Arch Dis Child Fetal Neonatal Ed 2001; 85 (1): F13–F17.
Christensen RD, Baer VL, Lambert DK, Ilstrup SJ, Eggert LD, Henry E . Association, among very-low-birthweight neonates, between red blood cell transfusions in the week after birth and severe intraventricular hemorrhage. Transfusion 2014; 54 (1): 104–108.
Chen YY, Wang HP, Lin SM, Chang JT, Hsieh KS, Huang FK et al. Taiwan Premature Infant Development Collaborative Study Group. Pulmonary hemorrhage in very low-birthweight infants: risk factors and management. Pediatr Int 2012; 54 (6): 743–747.
Tauzin L, Joubert C, Noel AC, Bouissou A, Moulies ME . Effect of persistent patent ductus arteriosus on mortality and morbidity in very low-birthweight infants. Acta Paediatr 2012; 101 (4): 419–423.
Audeh S, Smolkin T, Bental Y, Haramati Z, Blazer S, Litig E et al. Does admission hypothermia predispose to intraventricular hemorrhage in very-low-birth-weight infants? Neonatology 2011; 100 (4): 373–379.
Ahn HM, Park EA, Cho SJ, Kim YJ, Park HS . The association of histological chorioamnionitis and antenatal steroids on neonatal outcome in preterm infants born at less than thirty-four weeks' gestation. Neonatology 2012; 102 (4): 259–264.
Vermont-Oxford Neonatal Network, Database Manual of Operations, Release 2.0, Burlington, VT, 1993.
Klinger G, Sirota S, Luski A, Reichman B . The effect of bronchopulmonary dysplasia in very low birth weight infants on hospital length of stay – a national survey. J Perinatol 2006; 26: 640–644.
Dolberg A, Lusky A, Reichman B . Patent ductus arteriosus, indomethacin and necrotizing enterocolitis: a population based study. J Pediatr Gastroenterol Nutr 2005; 40: 184–188.
Kramer MS, Platt RW, Wen S, Joseph KS, Allen A, Abrahamowicz M et al. Fetal/Infant Health Study Group of the Canadian Perinatal Surveillance System. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics 2001; 108 (2): E35.
Papile LA, Burstein J, Burstein AR, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 gm. J Pediatr 1978; 92: 529–534.
Levene MI . Measurement of the growth of the lateral ventricles in preterm infants with real-time ultrasound. Arch Dis Child 1981; 56: 900–904.
Brouwer A, Groenendaal F, Van Haastert IL, Rademaker K, Hanlo P, De Vries L . Neurodevelopmental outcome of preterm infants with severe intraventricular hemorrhage and therapy for post-hemorrhagic ventricular dilatation. J Pediatr 2008; 152: 648–654.
Evans N, Moorcraft J . Effect of patency of the ductus arteriosus on blood pressure in very preterm infants. Arch Dis Child 1992; 67 (10 Spec No): 1169–1173.
Jim WT, Chiu NC, Chen MR, Hung HY, Kao HA, Hsu CH et al. Cerebral hemodynamic change and intraventricular hemorrhage in very low birth weight infants with patent ductus arteriosus. Ultrasound Med Biol 2005; 31 (2): 197–202.
Strahle J, Garton HJL, Maher CO, Muraszko KM, Keep RF, Guohua X . Mechanisms of hydrocephalus after neonatal and adult intraventricular hemorrhage. Transl Stroke Res 2012; 3 (Suppl 1): S25–S38.
Adams-Chapman I, Hansen NI, Stoll BJ, Higgins R . NICHD Research Network. Neurodevelopmental outcome of extremely low birth weight infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics 2008; 121 (5): e1167–e1177.
Acknowledgements
The Israel National VLBW infant database is partially funded by the Israel Center for Disease Control and the Israel Ministry of Health.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix A
Appendix A
The Israel Neonatal Network, which compiles the Israel national VLBW infant database, consists of these participating centers: Assaf Harofeh Medical Center, Tzrifin; Barzilai Medical Center, Ashkelon; Baruch Padeh Medical Center, Poriya, Tiberias; Bikur Cholim Hospital, Jerusalem; Bnei Zion Medical Center, Haifa; Carmel Medical Center, Haifa; Chaim Sheba Medical Center, Tel Hashomer; Emek Medical Center, Afula; French Saint Vincent de Paul Hospital, Nazareth; Hadassah University Hospital, Ein-Karem, Jerusalem; Hadassah University Hospital, Har Hazofim, Jerusalem; Hillel Yaffe Medical Center, Hadera; Holy Family Hospital, Nazareth; Kaplan Medical Center, Rehovot; Laniado Hospital, Netanya; Mayanei Hayeshua Medical Center, Bnei-Brak; Misgav Ladach Hospital, Jerusalem; Meir Medical Center, Kefar Saba; Rambam Medical Center, Haifa; Rivka Ziv Medical Center, Zefat; Schneider Children’s Medical Center of Israel and Rabin Medical Center, Beilinson Campus, Petach-Tikva; Scottish (EMMS) Hospital, Nazareth; Shaare-Zedek Medical Center, Jerusalem; Soroka Medical Center, Beer-Sheva; Sourasky Medical Center, Tel Aviv; Western Galilee Medical Center, Nahariya; Wolfson Medical Center, Holon; Yoseftal Hospital, Eilat.
Coordinating Center: Women and Children’s Health Research Unit, Gertner Institute for Epidemiology and Health Policy Research, Tel Hashomer.
Rights and permissions
About this article
Cite this article
Klinger, G., Osovsky, M., Boyko, V. et al. Risk factors associated with post-hemorrhagic hydrocephalus among very low birth weight infants of 24–28 weeks gestation. J Perinatol 36, 557–563 (2016). https://doi.org/10.1038/jp.2016.18
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.18
This article is cited by
-
Pathophysiologic mechanisms and strategies for the treatment of post-hemorrhagic hydrocephalus of prematurity
Child's Nervous System (2022)
-
Epidemiology of post-hemorrhagic ventricular dilatation in very preterm infants
Journal of Perinatology (2022)
-
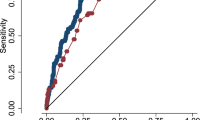
Ventricular shape evaluation on early ultrasound predicts post-hemorrhagic hydrocephalus
Pediatric Research (2019)
-
Predictors of mortality for preterm infants with intraventricular hemorrhage: a population-based study
Child's Nervous System (2018)