Abstract
Importance
Intraventricular hemorrhage (IVH) occurs in 15–45% of all very low birth weight (VLBW) preterm infants. Despite improvements in the perinatal care, the incidence of IVH remains high. As more preterm infants survive, there will be a larger burden of neurodevelopmental abnormalities borne by former preterm infants.
Objective
The objective of this study was to develop a predictive clinical model of IVH risk within the first few hours of life in an effort to augment perinatal counseling and guide the timing of future targeted therapies aimed at preventing or slowing the progression of disease.
Design
This is a prospective observational cohort study of VLBW infants born in the NICU at John’s Hopkins Children’s Center from 2011 to 2019. The presence and severity of IVH was defined on standard head ultrasound screening (HUS) using the modified Papile classification. Clinical variables were identified as significant using absolute risk regression from a general linear model. The model predictors included clinically meaningful variables that were not collinear.
Setting
This study took place at the Johns Hopkins Children’s Center Level IV NICU.
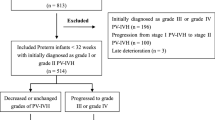
Participants
The study sample included VLBW infants treated in the neonatal intensive care unit (NICU) at John’s Hopkins Children’s Center from 2011 to 2019. A total of 683 infants included in the study had no or grade I IVH, and 115 infants had grades II through IV IVH. Exclusion criteria included admission to the JHH NICU after 24 h of age, BW > 1500 g, and failure to consent.
Main Outcome
The main outcome of this study was the presence of grades II-IV IVH on standard head ultrasound screening using the modified Papile classification [1].
Results
A total of 798 VLBW infants were studied in this cohort and 14.4% had moderate to severe IVH. Fifty four percent of the cohort was black, 33% white, and half of the cohort was male. A higher gestational age, 5-min Apgar score, hematocrit, and platelet count were significantly associated with decreased incidence of IVH in a multi-predictor model (ROC 0.826).
Conclusion and relevance
In the face of continued lack of treatments for IVH, prevention is still a primary goal to avoid long-term developmental sequela. This model can be used for perinatal counseling and may provide important information during the narrow therapeutic window for targeted prevention therapies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Request for data sharing should be submitted to the corresponding author for consideration.
References
Volpe J. Volpe’s neurology of the newborn, 6th ed. Elsevier; Volpe’s neurology of the newborn; 2018.
Pfahl S, Hoehn T, Lohmeier K, Richter-Werkle R, Babor F, Schramm D, et al. Long-term neurodevelopmental outcome following low grade intraventricular hemorrhage in premature infants. Early Hum Dev. 2018;117:62–67.
Glass HC, Costarino AT, Stayer SA, Brett CM, Cladis F, Davis PJ. Outcomes for extremely premature infants. Anesth Analg. 2015;120:1337–51.
Kobaly K, Schluchter M, Minich N, Friedman H, Taylor HG, Wilson-Costello D, et al. Outcomes of extremely low birth weight (<1 kg) and extremely low gestational age (<28 weeks) infants with bronchopulmonary dysplasia: effects of practice changes in 2000 to 2003. Pediatrics. 2008;121:73–81.
Schmidhauser J, Caflisch J, Rousson V, Bucher HU, Largo RH, Latal B. Impaired motor performance and movement quality in very-low-birthweight children at 6 years of age. Dev Med Child Neurol. 2006;48:718–22.
Mukerji A, Shah V, Shah PS. Periventricular/Intraventricular hemorrhage and neurodevelopmental outcomes: a meta-analysis. Pediatrics. 2015;136:1132–43.
Kiechl-Kohlendorfer U, Ralser E, Pupp Peglow U, Pehboeck-Walser N, Fussenegger B. Early risk predictors for impaired numerical skills in 5-year-old children born before 32 weeks of gestation. Acta Paediatr. 2013;102:66–71.
van de Bor M, den Ouden L. School performance in adolescents with and without periventricular-intraventricular hemorrhage in the neonatal period. Semin Perinatol. 2004;28:295–303.
Radic JAE, Vincer M, McNeely PD. Outcomes of intraventricular hemorrhage and posthemorrhagic hydrocephalus in a population-based cohort of very preterm infants born to residents of Nova Scotia from 1993 to 2010. J Neurosurg Pediatr. 2015;15:580–8.
Bassan H. Neurodevelopmental outcome in survivors of periventricular hemorrhagic infarction. Pediatrics. 2007;10:785–92.
Mirza H, Oh W, Laptook A, Vohr B, Tucker R, Stonestreet BS. Indomethacin prophylaxis to prevent intraventricular hemorrhage: association between incidence and timing of drug administration. J Pediatr. 2013;163:706–.e701.
Ment LR, Oh W, Ehrenkranz RA, Philip AG, Schneider K, Katz KH, et al. Risk period for intraventricular hemorrhage of the preterm neonate is independent of gestational age. Semin Perinatol. 1993;17:338–41.
Al-Abdi SY, Al-Aamri MA. A Systematic Review and Meta-analysis of the Timing of Early Intraventricular Hemorrhage in Preterm Neonates: Clinical and Research Implications. J Clin Neonatol. 2014;3:76–88.
Hand IL, Shellhaas RA, Milla SS. Routine neuroimaging of the preterm brain. Pediatrics. 2020;146:e202002908.
Robinson S, Conteh FS, Oppong AY, Yellowhair TR, Newville JC, El Demerdash N, et al. Extended combined neonatal treatment with erythropoietin plus melatonin prevents posthemorrhagic hydrocephalus of prematurity in rats. Front Cell Neurosci. 2018;12:322.
Gram M, Ekstrom C, Holmqvist B, Carey G, Wang X, Vallius S, et al. Insulin-like growth factor 1 in the preterm rabbit pup: characterization of cerebrovascular maturation following administration of recombinant human insulin-like growth factor 1/insulin-like growth factor 1-binding protein 3. Dev Neurosci. 2021;43:281–95.
Koschnitzky JE, Keep RF, Limbrick DD, McAllister JP, Morris JA, Strahle J, et al. Opportunities in posthemorrhagic hydrocephalus research: outcomes of the Hydrocephalus Association Posthemorrhagic Hydrocephalus Workshop. Fluids Barriers CNS. 2018;15:11.
Kaur A, Luu T, Shah P, Ayoub A, Auger N. Neonatal intraventricular hemorrhage and hospitalization in childhood. Pediatr Neurol. 2020;103:35–42.
Han R, McKinnon A, CreveCoeur T, Bash B, Mathur A, Smyser C, et al. Predictors of mortality for preterm infants with intraventricular hemorrhage: a population based study. Child’s Nerv Syst. 2018;34:2203–13.
Pedroza C, Troung VT. Performance of models for estimating absolute risk difference in multicenter trials with binary outcome. BMC Med Res Methodol. 2016;16:113.
Lee J, Hong M, Yum SK, Lee JH. Perinatal prediction model for severe intraventricular hemorrhage and the effect of early postnatal acidosis. Childs Nerv Syst. 2018;34:2215–22.
Andrikopoulou M, Almalki A, Farzin A, Cordeiro CN, Johnston MV, Burd I. Perinatal biomarkers in prematurity: early identification of neurologic injury. Int J Dev Neurosci. 2014;36:25–31.
Ballabh P. Intraventricular hemorrhage in premature infants: mechanism of disease. Pediatr Res. 2010;67:1–8.
Robinson S. Neonatal posthemorrhagic hydrocephalus from prematurity: pathophysiology and current treatment concepts. J Neurosurg Pediatr. 2012. https://doi.org/10.3171/2011.12.PEDS11136
He L, Zhou W, Zhao X, Liu X, Rong X, Song Y. Development and validation of a novel scoring system to predict severe intraventricular hemorrhage in very low birth weight infants. Brain Dev. 2019;41:671–7.
Poryo M, Boeckh JC, Gortner L, Zemlin M, Duppré P, Ebrahimi-Fakhari D, et al. Ante-, peri- and postnatal factors associated with intraventricular hemorrhage in very premature infants. Early Hum Dev. 2018;116:1–8.
Singh R, Gorstein SV, Bednarek F, Chou JH, McGowan EC, Visintainer PF. A predictive model for SIVH risk in preterm infants and targeted indomethacin therapy for prevention. Sci Rep. 2013;3:2539.
Luque MJ, Tapia JL, Villarroel L, Marshall G, Musante G, Carlo W, et al. A risk prediction model for severe intraventricular hemorrhage in very low birth weight infants and the effect of prophylactic indomethacin. J Perinatol. 2014;34:43–48.
Dekom S, Vachhani A, Patel K, Barton L, Ramanathan R, Noori S. Initial hematocrit values after birth and peri/intraventricular hemorrhage in extremely low birth weight infants. J Perinatol. 2018;38:1471–5.
Grevsen AK, Hviid CVB, Hansen AK, Hvas AM. The role of platelets in premature neonates with intraventricular hemorrhage: a systematic review and meta-analysis. Semin Thromb Hemost. 2020;46:366–78.
Dormann C, Elith J, Buchmann C, Gudrun C, Carre G, Garcia Marquez JR, et al. Collinearity: a review of methods to deal with it and a simulation study evaluating their performance. Ecography. 2013;36:027–46.
Curley A, Stanworth S, Phil D, Willoughby K, Fustolo-Gunnik F, Venkatesh V, et al. Randomized trial of platelet-transfusion thresholds in neonates. N Engl J Med. 2019;380:242–51.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics; 1988;44:837–45.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36.
Acknowledgements
This work is dedicated to Phoebe Marie Teng, Eli Joseph Teng, and Caleb Edward Teng who passed from IVH.
Funding
Grant funding for this project-(R01HD086058) (ADE, EMG, FJN, DV).
Author information
Authors and Affiliations
Contributions
FJN had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. RMW and FJN developed the study design, assisted with the data analysis, and interpreted the data. RMW created the tables and wrote the manuscript with support from FJN, EMG, ADE, and DV. CP assisted with data collection and ensured accuracy of the data. DV performed the data analysis and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was approved by Johns Hopkins University IRB. Information was collected under IRB 00026068 for the duration of the study. In 2018, the IRB began requiring consent from parent/guardian for inclusion in the study, and consent in both English and Spanish were obtained forthwith.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Weinstein, R.M., Parkinson, C., Everett, A.D. et al. A predictive clinical model for moderate to severe intraventricular hemorrhage in very low birth weight infants. J Perinatol 42, 1374–1379 (2022). https://doi.org/10.1038/s41372-022-01435-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01435-0



