Abstract
Objective:
Neonatologists provide antenatal counseling to support shared decision-making for complicated pregnancies. Poor or ambiguous prognostication can lead to inappropriate treatment and parental distress. We sought to evaluate the accuracy of antenatal prognosticaltion.
Study Design:
A retrospective cohort was assembled from a prospectively populated database of all outpatient neonatology consultations. On the basis of the written consultation, fetuses were characterized by diagnosis groups (multiple anomalies or genetic disorders, single major anomaly and obstetric complications), assigned to five prognostic categories (I=survivable, IIA=uncertain but likely survivable, II=uncertain, IIB=uncertain but likely non-survivable, III non-survivable) and two final outcome categories (fetal demise/in-hospital neonatal death or survival to hospital discharge). When possible, status at last follow-up was recorded for those discharged from the hospital. Prognostic accuracy was assessed using unweighted, multi-level likelihood ratios (LRs).
Results:
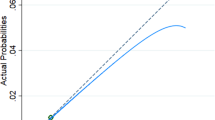
The final cohort included 143 fetuses/infants distributed nearly evenly among the three diagnosis groups. Over half (64%) were assigned an uncertain prognosis, but most of these could be divided into ‘likely survivable’ or ‘likely non-survivable’ subgroups. Overall survival for the entire cohort was 62% (89/143). All but one of the fetuses assigned a non-survivable prognosis suffered fetal demise or died before hospital discharge. The neonatologist’s antenatal prognosis accurately predicted the probability of survival by prognosis group (LR I=4.56, LR IIA=10.53, LR II=4.71, LR IIB=0.099, LR III=0.040). The LRs clearly differentiated between fetuses with high and low probability of survival. Eleven fetuses (7.7%) had misalignment between the predicted prognosis and outcome. Five died before discharge despite being given category I or IIA prognoses, whereas six infants with category IIB or III prognoses survived to discharge, though some of these were discharged to hospice care.
Conclusions:
The neonatologist’s antenatal prognosis accurately predicted fetal–neonatal outcome. Infants with non-survivable or uncertain but likely poor prognoses had a very low probability of survival, whereas those with good or uncertain prognoses had a high probability of survival. There were few cases of prognostic failure with most occurring in fetuses with one major or multiple anomalies. The few cases of prognostic failure suggest a need for caution. Honest disclosure of prognostic uncertainty and shared decision-making with families utilizing their personal values is critical in the antenatal encounter.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
American College of Obstetricians and Gynecologists, Committee on Ethics, American Academy of Pediatrics, Committee on Bioethics. Maternal-fetal intervention and fetal care centers. Pediatrics 2011; 128 (2): e473–e478.
Chock VY, Davis AS, Hintz SR . The roles and responsibilities of the neonatologist in complex fetal medicine: providing a continuum of care. Neoreviews 2015; 16 (1): e9–e15.
Tyson JE, Parikh NA, Langer J, Green C, Higgins RD . National Institute of Child Health and Human Development Neonatal Research Network. Intensive care for extreme prematurity—moving beyond gestational age. N Engl J Med 2008; 358 (16): 1672–1681.
Batton DG . Committee on fetus and newborn. Antenatal counseling regarding resuscitation at an extremely low gestational age. Pediatrics 2009; 124 (1): 422–427.
Wilkinson DJC, Thiele P, Watkins A, De Crespigny L . Fatally flawed? A review and ethical analysis of lethal congenital malformations. BJOG 2012; 119 (11): 1302–1308.
Bastek TK, Richardson DK, Zupancic JAF, Burns JP . Prenatal consultation practices at the border of viability: a regional survey. Pediatrics 2005; 116 (2): 407–413.
Brown SD, Donelan K, Martins Y, Burmeister K, Buchmiller TL, Sayeed SA et al. Differing attitudes toward fetal care by pediatric and maternal-fetal medicine specialists. Pediatrics 2012; 130 (6): e1534–e1540.
Hickman RL Jr, Daly BJ, Lee E . Decisional conflict and regret: consequences of surrogate decision making for the chronically critically ill. Appl Nurs Res 2012; 25 (4): 271–275.
Saigal S, Stoskopf B, Pinelli J, Streiner D, Hoult L, Paneth N et al. Self-perceived health-related quality of life of former extremely low birth weight infants at young adulthood. Pediatrics 2006; 118 (3): 1140–1148.
Boss RD, Hutton N, Sulpar LJ, West AM, Donohue PK . Values parents apply to decision-making regarding delivery room resuscitation for high-risk newborns. Pediatrics 2008; 122 (3): 583–589.
Wilkinson D . The self-fulfilling prophecy in intensive care. Theor Med Bioeth 2009; 30 (6): 401–410.
Kars MC, Grypdonck MHF, Beishuizen A, Meijer-van den Bergh EMM, van Delden JJM . Factors influencing parental readiness to let their child with cancer die. Pediatr Blood Cancer 2010; 54 (7): 1000–1008.
Hechler T, Blankenburg M, Friedrichsdorf S, Garske D, Hübner B, Menke A et al. Parents’ perspective on symptoms, quality of life, characteristics of death and end-of-life decisions for children dying from cancer. Klin Pädiatr 2008; 220 (3): 166–174.
Acknowledgements
We gratefully acknowledge Samantha McCully for her assistance in maintaining a database of outpatient neonatology consults in the Fetal Diagnostic Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kukora, S., Gollehon, N., Weiner, G. et al. Prognostic accuracy of antenatal neonatology consultation. J Perinatol 37, 27–31 (2017). https://doi.org/10.1038/jp.2016.171
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.171
This article is cited by
-
Infant mode of death in the neonatal intensive care unit: A systematic scoping review
Journal of Perinatology (2022)
-
Conjoined twins: an obstetrician’s guide to prenatal care and delivery management
Journal of Perinatology (2021)
-
A systematic concept analysis of ‘technology dependent’: challenging the terminology
European Journal of Pediatrics (2021)
-
The complexity of physicians’ understanding and management of prognostic uncertainty in neonatal hypoxic-ischemic encephalopathy
Journal of Perinatology (2019)