Abstract
Objectives:
Inhaled nitric oxide (iNO) is effective in conjunction with tracheal intubation (TI) and mechanical ventilation (MV) for treating arterial pulmonary hypertension and hypoxemic respiratory failure (HRF) in near-term and term newborns. Non-invasive respiratory support with nasal continuous positive airway pressure (CPAP) is increasingly used to avoid morbidity associated with TI and MV, yet the effectiveness of iNO delivery via nasal CPAP remains unknown. To evaluate the effectiveness of iNO delivered via the bubble nasal CPAP system in term and preterm newborns with HRF.
Study design:
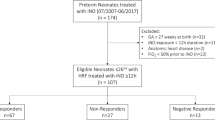
Electronic medical records from all infants admitted to the neonatal intensive care unit (NICU) during 2005 to 2014 (n=10, 895) were screened for treatment with iNO therapy for HRF. Detailed data on population characteristics and cardiorespiratory, iNO and respiratory support indices were abstracted for all infants, who were administered iNO non-invasively using bubble nasal CPAP. Change in relevant indices at baseline (before initiating non-invasive iNO) and at 3, 6, 12 and 24 h after non-invasive iNO therapy were analyzed using repeated measures analysis of variance.
Results:
Of 795 infants treated with iNO (7.3% of total NICU admissions) over a 10-year period, 107 infants (13.4% of iNO treated) with birth weight 2448±1112 g and gestational age 35.3±5.8 weeks received iNO non-invasively. 25 infants received iNO exclusively non-invasively, whereas in remaining 82 infants non-invasive route followed invasive delivery via TI and MV. Indications for using non-invasive iNO included idiopathic pulmonary hypertension (39%), congenital heart disease (37%), bronchopulmonary dysplasia (10%), meconium aspiration syndrome (9%) and congenital diaphragmatic hernia (5%). Over the 24 h following initiation of non-invasive iNO, fractional oxygen requirements decreased (0.38 to 0.32; P<0.0005) and SpO2 increased (90.7 to 91.6%; P<0.01) with no significant changes in heart rate, respiratory rate, blood pressure, pH and PaCO2. On average non-invasive iNO was initiated on day of life 9 with a maximal dose was 20 p.p.m. The average duration of iNO therapy and the duration over which it was weaned off were 134 and 51 h, respectively. Analysis of environmental gases during non-invasive iNO therapy revealed median ambient nitrogen dioxide and nitric oxide levels of 0.30 and 0.01 p.p.m., respectively.
Conclusions:
Initiation of iNO in infants on bubble nasal CPAP or continuation of iNO in infants transitioning from MV to bubble nasal CPAP is associated with improved oxygenation during HRF in term and preterm infants. Non-invasive iNO may have a synergistic effect with airway recruitment strategies such as nasal CPAP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
The Neonatal Inhaled Nitric Oxide Study Group. Inhaled nitric oxide in full-term and nearly full-term infants with hypoxic respiratory failure. N Engl J Med 1997; 336: 597–604.
Clark RH, Kueser TJ, Walker MW, Southgate WM, Huckaby JL, Perez JA et al. Low-dose nitric oxide therapy for persistent pulmonary hypertension of the newborn. Clinical Inhaled Nitric Oxide Research Group. N Engl J Med 2000; 17: 469–474.
Frostell C . Nitric oxide inhalation – future drug or an invitation to disaster? Pediatr Anesth 1994; 4: 147–150.
Roze JC, Storme L, Zupan V, Morville P, Dinh-Xuan AT, Mercier JC . Echocardiographic investigation of inhaled nitric oxide in newborn babies with severe hypoxaemia. Lancet 1994; 344: 303–305.
American Academy of Pediatrics. Committee on Fetus and Newborn. Use of inhaled nitric oxide. Pediatrics 2000; 106 (2 Pt 1): 344–345.
Macrae DJ, Field D, Mercier JC, Moller J, Stiris T, Biban P et al. Inhaled nitric oxide therapy in neonates and children: reaching a European consensus. Intensive Care Med 2004; 30: 372–380.
Cole FS, Alleyne C, Barks JD, Boyle RJ, Carroll JL, Dokken D et al. NIH Consensus Development Conference statement: inhaled nitric-oxide therapy for premature infants. Pediatrics 2011; 127 (2): 363–369.
Ballard RA, Truog WE, Cnaan A, Martin RJ, Ballard PL, Merrill JD et alNO CLD Study Group. Inhaled nitric oxide in preterm infants undergoing mechanical ventilation. N Engl J Med. 2006; 355 (4): 343–353.
Hibbs AM, Walsh MC, Martin RJ, Truog WE, Lorch SA, Alessandrini E et al. One-year respiratory outcomes of preterm infants enrolled in the Nitric Oxide (to prevent) Chronic Lung Disease trial. J Pediatr 2008; 153 (4): 525–529.
Van Marter LJ, Allred EN, Pagano M, Sanocka U, Parad R, Moore M et al. Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? The Neonatology Committee for the Developmental Network. Pediatrics 2000; 105 (6): 1194–1201.
Lindwall R, Frostell CG, Lönnqvist PA . Delivery characteristics of a combined nitric oxide nasal continuous positive airway pressure system. Paediatr Anaesth 2002; 12 (6): 530–536.
Lindwall R, Blennow M, Svensson M, Jonsson B, Berggren-Boström E, Flanby M et al. A pilot study of inhaled nitric oxide in preterm infants treated with nasal continuous positive airway pressure for respiratory distress syndrome. Intensive Care Med 2005; 31 (7): 959–964.
Lindwall R, Svensson ME, Frostell CG, Eksborg S, Gustafsson LE . Workplace NO and NO2 during combined treatment of infants with nasal CPAP and NO. Intensive Care Med 2006; 32 (12): 2034–2041.
Putensen C, Rasanen J, Lopez FA, Downs JB . Continuous positive airway pressure modulates effect of inhaled nitric oxide on the ventilation-perfusion distributions in canine lung injury. Chest 1994; 106 (5): 1563–1569.
Jones C . Inhaled nitric oxide: are the safety issues being addressed? Intensive Crit Care Nurs 1998; 14: 271–275.
Markhorst DG, Leenhoven T, Uiterwijk JW, Meulenbelt J, van Vught AJ . Occupational exposure during nitric oxide inhalational therapy in a pediatric intensive care setting. Intensive Care Med 1996; 22: 954–958.
Mourgeon E, Levesque E, Duveau C, Law-Koune JD, Charbit B, Ternissien E et al. Factors influencing indoor concentrations of nitric oxide in a Parisian intensive care unit. Am J Respir Crit Care Med 1997; 156 (5): 1692–1695.
Ivy DD, Wiggins JW, Badesch DB, Kinsella JP, Kelminson LL, Abman SH . Nitric oxide and prostacyclin treatment of an infant with primary pulmonary hypertension. Am J Cardiol 1994; 74: 414–416.
Kakuya F, Takase M, Ishii N, Kajino M, Hayashi T, Miyamoto K et al. Inhaled nitric oxide therapy via nasopharyngeal tube in an infant with end-stage pulmonary hypertension. Acta Paediatr Jpn 1998; 40: 155–158.
Channick RN, Newhart JW, Johnson FW, Williams PJ, Auger WR, Fedullo PF et al. Pulsed delivery of inhaled nitric oxide to patients with primary pulmonary hypertension: an ambulatory delivery system and initial clinical tests. Chest 1996; 109: 1545–1549.
Kinsella JP, Parker TA, Ivy DD, Abman SH . Noninvasive delivery of inhaled nitric oxide therapy for late pulmonary hypertension in newborn infants with congenital diaphragmatic hernia. J Pediatr 2003; 142: 397–401.
Schlobohm RM, Falltrick RT, Quan SF, Katz JA . Lung volumes, mechanics, and oxygenation during spontaneous positive-pressure ventilation: the advantage of CPAP over EPAP. Anesthesiology 1981; 55: 416–422.
Pesenti A, Riboni A, Marcolin R, Gattinoni L . Venous admixture (QVA/QT) and true shunt (Qs/Qt) in ARF patients: effects of PEEP at constant FIo2. Intensive Care Med 1983; 9: 307–311.
Adnot S, Radermacher P, Andrivet P, Dubois RJ, Dupeyrat A, Lemaire F . Effects of sodium-nitroprusside and urapidil on gas exchange and ventilation-perfusion relationships in patients with congestive heart failure. Eur Respir J 1991; 4: 69–75.
Carlo WA . Gentle ventilation: the new evidence from the SUPPORT, COIN, VON, CURPAP, Colombian Network, and Neocosur Network trials. Early Hum Dev 2012; 88 (Suppl 2): S81–S83.
Mattsson EJ, Geary RL, Kraiss LW, Vergel S, Liao JK, Corson MA et al. Is smooth muscle growth in primate arteries regulated by endothelial nitric oxide synthase? J Vasc Surg 1998; 28 (3): 514–521.
Sarkar R, Webb RC . Does nitric oxide regulate smooth muscle cell proliferation? A critical appraisal. J Vasc Res 1998; 35 (3): 135–142.
Kinsella JP, Parker TA, Galan H, Sheridan BC, Halbower AC, Abman SH . Effects of inhaled nitric oxide on pulmonary edema and lung neutrophil accumulation in severe experimental hyaline membrane disease. Pediatr Res 1997; 41 (4 Pt 1): 457–463.
Sato Y, Walley KR, Klut ME, English D, D'yachkova Y, Hogg JC et al. Nitric oxide reduces the sequestration of polymorphonuclear leukocytes in lung by changing deformability and CD18 expression. Am J Respir Crit Care Med 1999; 159 (5 Pt 1): 1469–1476.
Acknowledgements
This study was supported by Grant support from Mallinckrodt Pharmaceuticals (formerly Ikaria), Hampton, NJ, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sahni, R., Ameer, X., Ohira-Kist, K. et al. Non-invasive inhaled nitric oxide in the treatment of hypoxemic respiratory failure in term and preterm infants. J Perinatol 37, 54–60 (2017). https://doi.org/10.1038/jp.2016.164
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.164
This article is cited by
-
Critical role of nitric oxide in impeding COVID-19 transmission and prevention: a promising possibility
Environmental Science and Pollution Research (2022)