Abstract
Objective:
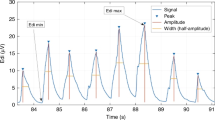
The electrical activity of the diaphragm (Edi) reflects neural respiratory drive. Edi peak correlates with inspiratory drive and Edi minimum (Edi min) correlates with the tonic activity of the diaphragm. Edi data in non-ventilated preterm neonates have not been determined.
The primary aim of this study was to determine Edi values in non-ventilated preterm neonates throughout postnatal maturation and with various types of noninvasive respiratory support. The secondary aim was to evaluate the success or complications of placement of the Edi catheter in premature neonates.
Study design:
This was a prospective observational study of non-ventilated neonates <33 weeks gestation. Data were collected weekly using an Edi catheter placed in neonates on highflow nasal cannula (HFNC), nasal cannula (NC) or room air (RA). Clinical stability was determined by measuring heart rate (HR), respiratory rate (RR) and oxygen saturation (Sats). Success and adverse events of Edi catheter placement was monitored. Statistics were obtained by analysis of variance, P<0.05 was considered significant.
Result:
Seventeen neonates were enrolled at 26 to 33 weeks postmenstrual age and studied from 1 to 10 weeks in duration. Overall Edi peak was 10.8±3.7 mcV (range 3.7 to 18.7) and Edi min was 2.8±1.1 mcV (range 0.8 to 7.6). There was no difference in Edi peak and min over postmenstrual ages within or between neonates, and no difference between those neonates on HFNC, NC or RA. HR, RR and Sats were not different over postmenstrual age or between any groups. The Edi catheter was placed successfully in 100% of these neonates. There were no adverse events noted.
Conclusion:
In clinically stable neonates, the inspiratory drive (Edi peak) and tonic activity (Edi min) do not change with postnatal maturation or with the level of noninvasive respiratory support. The Edi catheter can be placed successfully in these premature neonates. These Edi data have the potential to guide ventilatory management of premature neonates.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Beck J, Reilly M, Grasselli G, Mirabella L, Slutsky AS, Dunn MS et al. Patient-ventilator interaction during neurally adjusted ventilatory assist in low birth weight infants. Pediatr Res 2009; 65: 663–668.
Breatnach C, Conlon NP, Stack M, Healy M, O'Hare BP . A prospective crossover comparison of neurally adjusted ventilatory assist and pressure-support ventilation in a pediatric and neonatal intensive care unit population. Pediatr Crit Care Med 2010; 11: 7–11.
Luo YM, Moxham J, Polkey MI . Diaphragm electromyography using an oesophageal catheter: current concepts. Clin Sci (Lond) 2008; 115: 233–244.
Sinderby C, Spahija J, Beck J . Changes in respiratory effort sensation over time are linked to the frequency content of diaphragm electrical activity. Am J Respir Crit Care Med 2001; 163: 905–910.
Beck J, Sinderby C, Lindstrom L, Grassino A . Influence of bipolar electrode positioning on measurements of humna crural diaphragm EMG. J Appl Physiol 1996; 81: 434–449.
Rowley DD, Lowson SM, Caruso FJ . Diaphragmatic electrical activity signaling unmasks asynchrony and improves patient-ventilator interaction. Respiratory Therapy 2009; 4: 51–53.
Sinderby C, Beck J . Proportional assist ventilation and neurally adjusted ventilatory assist—better approaches to patient ventilator synchrony? Clin Chest Med 2008; 29: 329–342.
Emeriaud G, Beck J, Tucci M, Lacroix J, Sinderby C . Diaphragm electrical activity during expiration in mechanically ventilated infants. Pediatr Res 2006; 59: 705–710.
Beck J, Sinderby C . Proportional assist ventilation and neurally adjusted ventilatory assist In: Esquinas AM, (eds) Appl Technol Mech Ventilation. Karger: Basel pp 1–5 2011.
Sinderby C, Beck J . Neurally adjusted ventilatory assist (NAVA): an update and summary of experiences. Sci NY 2007; 11: 243–252.
Hutten GJ, van Eykern LA, Latzin P, Kyburz M, van Aalderen WM, Frey U . Relative impact of respiratory muscle activity on tidal flow and end expiratory volume in healthy neonates. Pediatr Pulmonol 2008; 43: 882–891.
Sinderby C, Beck J, Spahija J, de Marchie M, Lacroix J, Navalesi P et al. Inspiratory muscle unloading by neurally adjusted ventilatory assist during maximal inspiratory efforts in healthy subjects. Chest 2007; 131: 711–717.
Stein HM, Wilmoth J, Burton J . Electrical activity of the diaphragm in a small cohort of term neonates. Respir Care 2012; 57: 1483–1487.
Barwing J, Ambold M, Linden N, Quintel M, Moerer O . Evaluation of the catheter positioning for neurally adjusted ventilatory assist. Intensive Care Med 2009; 35: 1809–1814.
Beck J, Reilly M, Grasselli G, Qui H, Slutsky AS, Dunn MS et al. Charaterization of neural breathing pattern in spontaneously breathing preterm infants. Pediatr Res 2011; 70: 607–613.
Brander L, Leong-Poi H, Beck J, Brunet F, Hutchison SJ, Slutsky AS et al. Titration and implementation of neurally adjusted ventilatory assist in critically ill patients. Chest 2009; 135: 695–703.
Beck J, Sinderby C, Lindstrom L, Grassino A . Effects of lung volume on daiphragm EMG signal strength during voluntary contractions. J Appl Physiol 1998; 85: 1123–1134.
Beck J, Sinderby C, Weinberg J, Grassino A . Effects of muscle-to-electrode distance on the human diaphragm electromyogram. J Appl Physiol 1995; 79: 975–985.
Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S et al. Neural control of mechanical ventilation in respiratory failure. Nat Med 1999; 5: 1433–1436.
Barwing J, Pedroni C, Quintel M, Moerer O . Influence of body position, PEEP and intra-abdominal pressure on the catheter positioning for neurally adjusted ventilatory assist. Intensive Care Med 2011; 37: 2041–2045.
Stokowski LA . A primer on apnea of prematurity. Adv Neonatal Care 2005; 5: 155–170.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Howard Stein is a speaker for Maquet (the manufacturer of the SERVO-i ventilator). The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Stein, H., Hall, R., Davis, K. et al. Electrical activity of the diaphragm (Edi) values and Edi catheter placement in non-ventilated preterm neonates. J Perinatol 33, 707–711 (2013). https://doi.org/10.1038/jp.2013.45
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2013.45
Keywords
This article is cited by
-
Cardiorespiratory measures shortly after extubation and extubation outcomes in extremely preterm infants
Pediatric Research (2023)
-
Reference values for diaphragm electrical activity (Edi) in newborn infants
BMC Pediatrics (2022)
-
Effects of heliox and non-invasive neurally adjusted ventilatory assist (NIV-NAVA) in preterm infants
Scientific Reports (2021)
-
Diaphragmatic activity and neural breathing variability during a 5-min endotracheal continuous positive airway pressure trial in extremely preterm infants
Pediatric Research (2021)
-
Changes in pulmonary oxygen content are detectable with laser absorption spectroscopy: proof of concept in newborn piglets
Pediatric Research (2021)