Abstract
Background
Nasal continuous positive airway pressure, nasal intermittent positive pressure ventilation, and non-invasive neurally adjusted ventilatory assist are modes of non-invasive respiratory support. The objective was to investigate if cardiorespiratory measures performed shortly after extubation are associated with extubation outcomes and predictors of extubation success.
Methods
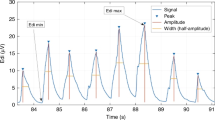
Randomized crossover trial of infants with birth weight (BW) ≤ 1250 g undergoing their first extubation. Shortly after extubation, electrocardiogram and electrical activity of the diaphragm (Edi) were recorded during 40 min on each mode. Measures of heart rate variability (HRV), diaphragmatic activity (Edi area, breath area and amplitude), and respiratory variability (RV) were computed on each mode and compared between infants with extubation success or failure (reintubation ≤ 7 days).
Results
Twenty-three extremely preterm infants with median [IQR] gestational age 25.9 weeks [25.2–26.4] and BW 760 g [595–900] were included: 14 success and 9 failures. There were significant differences for HRV (very low-frequency power and sample entropy) and RV parameters (breath areas, amplitudes and expiratory times) between groups, with moderate strength (0.75–0.80 areas under ROC curves) in predicting success. Diaphragmatic activity measures were similar between groups.
Conclusions
In extremely preterm infants receiving non-invasive respiratory support shortly after extubation, several cardiorespiratory variability parameters were associated with successful extubation with moderate predictive accuracy.
Impact:
-
Measures of cardiorespiratory variability, performed in extremely preterm infants while receiving NCPAP, NIPPV, and NIV-NAVA shortly after extubation, were significantly different between patients that succeeded or failed extubation.
-
Cardiorespiratory variability measures had a moderate predictive accuracy for extubation success and can be potentially used as biomarkers, in recently extubated infants.
-
Future investigations in this population may also consider including cardiorespiratory variability measures when assessing types of post-extubation respiratory support and promote individualized care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Research data are not shared.
References
Shalish, W. & Sant’Anna, G. M. Deciphering extubation failure in extremely preterm infants: time to embrace complexity and move forward. J. Pediatrics 194, 263 (2018).
Shalish, W., Latremouille, S., Papenburg, J. & Sant’Anna, G. M. Predictors of extubation readiness in preterm infants: a systematic review and meta-analysis. Arch. Dis. Child Fetal Neonatal Ed. 104, F89–f97 (2019).
Mehta, P., Berger, J., Bucholz, E. & Bhandari, V. Factors affecting nasal intermittent positive pressure ventilation failure and impact on bronchopulmonary dysplasia in neonates. J. Perinatol. 34, 754–760 (2014).
Ferguson, K. N., Roberts, C. T., Manley, B. J. & Davis, P. G. Interventions to improve rates of successful extubation in preterm infants: a systematic review and meta-analysis. JAMA Pediatr. 171, 165–174 (2017).
Cummings, J. J. & Polin, R. A. Noninvasive respiratory support. Pediatrics 137, https://doi.org/10.1542/peds.2015-3758 (2016).
Lemyre, B., Davis, P. G., De Paoli, A. G. & Kirpalani, H. Nasal intermittent positive pressure ventilation (Nippv) versus nasal continuous positive airway pressure (Ncpap) for preterm neonates after extubation. Cochrane Database Syst. Rev. 2, Cd003212 (2017).
Moretti, C. et al. Nasal flow-synchronized intermittent positive pressure ventilation to facilitate weaning in very low-birthweight infants: unmasked randomized controlled trial. Pediatr. Int. 50, 85–91 (2008).
Khalaf, M. N., Brodsky, N., Hurley, J. & Bhandari, V. A prospective randomized, controlled trial comparing synchronized nasal intermittent positive pressure ventilation versus nasal continuous positive airway pressure as modes of extubation. Pediatrics 108, 13–17 (2001).
Lee, B. K., Shin, S. H., Jung, Y. H., Kim, E. K. & Kim, H. S. Comparison of Niv-Nava and Ncpap in facilitating extubation for very preterm infants. BMC Pediatr. 19, 298 (2019).
Makker, K. et al. Comparison of extubation success using noninvasive positive pressure ventilation (NIPPV) versus noninvasive neurally adjusted ventilatory assist (NI-NAVA). J. Perinatol. 40, 1202–1210 (2020).
Yagui, A. C. Z. et al. Is noninvasive neurally adjusted ventilatory assistance (NIV-NAVA) an alternative to NCPAP in preventing extubation failure in preterm infants? J. Matern. Fetal Neonatal. Med. 34, 3756–3760 (2019).
Fairchild, K. D. et al. Septicemia mortality reduction in neonates in a heart rate characteristics monitoring trial. Pediatr. Res. 74, 570–575 (2013).
Goulding, R. M. et al. Heart rate variability in hypoxic ischemic encephalopathy: correlation with eeg grade and 2-Y neurodevelopmental outcome. Pediatr. Res. 77, 681–687 (2015).
Chakraborty, M., Watkins, W. J., Tansey, K., King, W. E. & Banerjee, S. Predicting extubation outcomes using heart rate characteristics index in preterm infants: a cohort study. Eur. Respir. J. 22, 22 (2020).
Goel, N., Chakraborty, M., Watkins, W. J. & Banerjee, S. Predicting extubation outcomes—a model incorporating heart rate characteristics index. J. Pediatrics 195, 53–58.e51 (2018).
Kaczmarek, J. et al. Heart rate variability and extubation readiness in extremely preterm infants. Neonatology 104, 42–48 (2013).
Silva, M. G. F., Gregorio, M. L. & de Godoy, M. F. Does heart rate variability improve prediction of failed extubation in preterm infants? J. Perinat. Med 47, 252–257 (2019).
Latremouille, S. et al. Heart rate variability in extremely preterm infants receiving nasal Cpap and non-synchronized noninvasive ventilation immediately after extubation. Respir. Care 63, 62–69 (2018).
Latremouille, S. et al. The effects of nasal continuous positive airway pressure and high flow nasal cannula on heart rate variability in extremely preterm infants after extubation: a randomized crossover trial. Pediatr. Pulmonol. 54, 788–796 (2019).
Iyer, N. P. et al. Neural breathing pattern in newborn infants pre‐and postextubation. Acta Paediatr. 106, 1928–1933 (2017).
Latremouille, S., Bhuller, M., Rao, S., Shalish, W. & Sant’Anna, G. Diaphragmatic activity and neural breathing variability during a 5-min endotracheal continuous positive airway pressure trial in extremely preterm infants. Pediatr. Res. 89, 1810–1817 (2020).
Kaczmarek, J., Kamlin, C. O., Morley, C. J., Davis, P. G. & Sant’anna, G. M. Variability of respiratory parameters and extubation readiness in ventilated neonates. Arch. Dis. Child Fetal Neonatal Ed. 98, F70–F73 (2013).
Stein, H., Hall, R., Davis, K. & White, D. B. Electrical activity of the diaphragm (Edi) values and Edi catheter placement in non-ventilated preterm neonates. J. Perinatol. 33, 707–711 (2013).
Sassi, R. et al. Advances in heart rate variability signal analysis: Joint Position Statement by the E-Cardiology Esc Working Group and the European Heart Rhythm Association Co-Endorsed by the Asia Pacific Heart Rhythm Society. Europace 17, 1341–1353 (2015).
Task Force of The European Society of Cardiology and The North American Society of Pacing and Electrophysiology. Heart Rate variability: standards of measurement, physiological interpretation and clinical use. Circulation 93, 1043–1065 (1996).
Shalish, W. et al. Patterns of reintubation in extremely preterm infants: a longitudinal cohort study. Pediatr. Res. 83, 969–975 (2018).
Latremouille, S., Bhuller, M., Shalish, W. & Sant’Anna, G. Cardiorespiratory effects of NIV-NAVA, NIPPV, and NCPAP shortly after extubation in extremely preterm infants: a randomized crossover trial. Pediatr. Pulmonol. 56, 3273–3282 (2021).
Stephan-Blanchard, E. et al. Heart rate variability in sleeping preterm neonates exposed to cool and warm thermal conditions. PLoS ONE [Electron. Resour.] 8, e68211 (2013).
De Rogalski Landrot, I. et al. Autonomic nervous system activity in premature and full-term infants from theoretical term to 7 years. Autonomic Neurosci.-Basic Clin. 136, 105–109 (2007).
Patural, H. et al. Autonomic cardiac control of very preterm newborns: a prolonged dysfunction. Early Hum. Dev. 84, 681–687 (2008).
Stephan-Blanchard, E. et al. The dynamics of cardiac autonomic control in sleeping preterm neonates exposed in utero to smoking. Clin. Neurophysiol. 127, 2871–2877 (2016).
Stock, C. et al. Autonomic dysfunction with early respiratory syncytial virus-related infection. Auton. Neurosci. 156, 90–95 (2010).
Goulding, R. M. et al. Heart rate variability in hypoxic ischemic encephalopathy during therapeutic hypothermia. Pediatr. Res. 81, 609–615 (2017).
Lucchini, M., Signorini, M. G., Fifer, W. P. & Sahni, R. Multi-parametric heart rate analysis in premature babies exposed to sudden infant death syndrome. Conf. Proc.: Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2014, 6389–6392 (2014).
Lucchini, M., Fifer, W. P., Sahni, R. & Signorini, M. G. Novel heart rate parameters for the assessment of autonomic nervous system function in premature infants. Physiol. Meas. 37, 1436–1446 (2016).
Gomes, E. et al. Autonomic responses of premature newborns to body position and environmental noise in the neonatal intensive care unit. Rev. Brasileira de. Ter. Intensiv. 31, 296–302 (2019).
Weissman, A., Zimmer, E. Z., Aranovitch, M. & Blazer, S. Heart rate dynamics during acute pain in newborns. Pflügers Arch.-Eur. J. Physiol. 464, 593–599 (2012).
Cremillieux, C., Makhlouf, A., Pichot, V., Trombert, B. & Patural, H. Objective assessment of induced acute pain in neonatology with the newborn infant parasympathetic evaluation index. Eur. J. Pain. 22, 1071–1079 (2018).
de Souza Filho, L. F. M. et al. Evaluation of the autonomic nervous system by analysis of heart rate variability in the preterm infants. BMC Cardiovasc. Disord. 19, 198 (2019).
Beuchee, A. et al. Uncorrelated randomness of the heart rate is associated with sepsis in sick premature infants. Neonatology 96, 109–114 (2009).
Lake, D. E., Richman, J. S., Griffin, M. P. & Moorman, J. R. Sample entropy analysis of neonatal heart rate variability. Am. J. Physiol. Regulatory Integr. Comp. Physiol. 283, R789–R797 (2002).
Griffin, M. P. et al. Abnormal heart rate characteristics preceding neonatal sepsis and sepsis-like illness. Pediatr. Res. 53, 920–926 (2003).
Hutten, G. J. et al. Respiratory muscle activity related to flow and lung volume in preterm infants compared with term infants. Pediatr. Res. 68, 339 (2010).
Usemann, J. et al. Variability of tidal breathing parameters in preterm infants and associations with respiratory morbidity during infancy: a cohort study. J. Pediatr. 205, e61 (2019).
Navarro, X., Porée, F., Beuchée, A. & Carrault, G. Artifact rejection and cycle detection in immature breathing: application to the early detection of neonatal sepsis. Biomed. Signal Process Control 16, 9–16 (2015).
Patel, M. et al. Clinical associations with immature breathing in preterm infants: part 2—periodic breathing. Pediatr. Res. 80, 28–34 (2016).
Funding
This work was supported by the Montreal Children’s Foundation research funds for G.S. In addition, S.L. and W.S. were both supported from Fonds de la recherche en sante du Quebec (FRQS) doctoral research awards in partnership with the Fondation Des Étoiles.
Author information
Authors and Affiliations
Contributions
S.L. assisted in patient screening and enrollment, was responsible for data acquisition, analyzed the data, and drafted the manuscript. M.B. assisted in patient screening and enrollment, and data acquisition. W.S. assisted in patient screening, enrollment, and data acquisition, and provided critical input into study design, data analyses, and writing of the manuscript. G.S. supervised the design and execution of the study, and provided critical input into the final data analyses and writing of the manuscript. All authors critically reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Informed consent was obtained from parents or legal guardians.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Latremouille, S., Bhuller, M., Shalish, W. et al. Cardiorespiratory measures shortly after extubation and extubation outcomes in extremely preterm infants. Pediatr Res 93, 1687–1693 (2023). https://doi.org/10.1038/s41390-022-02284-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02284-5
This article is cited by
-
Peri-extubation settings in preterm neonates: a systematic review and meta-analysis
Journal of Perinatology (2024)