Abstract
Objective:
To evaluate cerebral hemodynamics during dopamine treatment in hypotensive (mean arterial blood pressure (MABP)<gestational age) extremely low birth weight (ELBW) infants.
Study Design:
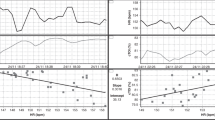
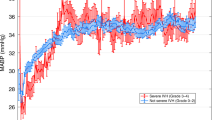
Continuous monitoring of cerebral blood flow velocity (CBFv), MABP and PCO2 was performed in hypotensive ELBW infants on the first day of life, beginning with an ∼15-min baseline reading and continued during advancing dopamine infusion until MABP was optimized. Physiological variables and CBFv reactivity were compared before and after MABP was optimized.
Result:
Fifteen hypotensive ELBW infants (625±174 g; 24 (23 to 24.8) weeks) were studied. Mean CBFv increased from 10.9±3.7 to 15.7±5.7 cm s−1 (P=0.001) simultaneously as MABP increased from 22.3±2.8 to 35.2±9.7 mm Hg (P<0.001). Mean CBFv reactivity (95% confidence interval (CI)) was 3.9 (1.6 to 6.2) %mm Hg−1. Nine infants died and/or developed severe intraventricular hemorrhage (IVH).
Conclusion:
Mean CBFv increased pressure-passively as MABP was optimized by dopamine treatment in very sick hypotensive ELBW infants on the first day of life.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Fanaroff JM, Wilson-Costello DE, Newman NS, Montpetite MM, Fanaroff AA . Treated hypotension is associated with neonatal morbidity and hearing loss in extremely low birth weight infants. Pediatrics 2006; 117: 1131–1135.
Kuint J, Barak M, Morag I, Maayan-Metzger A . Early treated hypotension and outcome in very low birth weight infants. Neonatology 2009; 95: 311–316.
Watkins AM, West CR, Cooke RW . Blood pressure and cerebral haemorrhage and ischaemia in very low birthweight infants. Early Hum Dev 1989; 19: 103–110.
Martens SE, Rijken M, Stoelhorst GMSJ, van Zwieten PHT, Zwinderman AH, Wit JM et al. Is hypotension a major risk factor for neurological morbidity at term age in very preterm infants? Early Hum Dev 2003; 75: 79–89.
Barrington KJ, Dempsey EM . Cardiovascular support in the preterm: Treatments in search of indications. J Pediatr 2006; 148: 289–291.
Batton B, Zhu X, Fanaroff J, Kirchner HL, Berlin S, Wilson-Costello D et al. Blood pressure, anti-hypotensive therapy, and neurodevelopment in extremely preterm infants. J Pediatr 2009; 154: 351–357.
Dempsey EM, Al Hazzani F, Barrington KJ . Permissive hypotension in the extremely low birth weight infant with signs of good perfusion. Arch Dis Child Fetal Neonatal Ed 2009; 94: F241–F244.
Lightburn MH, Gauss CH, Williams DK, Kaiser JR . Cerebral blood flow velocities in extremely low birth weight infants with hypotension and infants with normal blood pressure. J Pediatr 2009; 154: 824–828.
Seri I . Cardiovascular, renal, and endocrine actions of dopamine in neonates and children. J Pediatr 1995; 126: 333–344.
Sassano-Higgins S, Friedlich P, Seri I . A meta-analysis of dopamine use in hypotensive preterm infants: blood pressure and cerebral hemodynamics. J Perinatol 2011; 31: 647–655.
Munro MJ, Walker AM, Barfield CP . Hypotensive extremely low birth weight infants have reduced cerebral blood flow. Pediatrics 2004; 114: 1591–1596.
Seri I, Rudas G, Bors Z, Kanyicska B, Tulassay T . Effects of low-dose dopamine infusion on cardiovascular and renal functions, cerebral blood flow, and plasma catecholamine levels in sick preterm neonates. Pediatr Res 1993; 34: 742–749.
Zhang J, Penny DJ, Kim NS, Yu VYH, Smolich JJ . Mechanisms of blood pressure increase induced by dopamine in hypotensive preterm neonates. Arch Dis Child Fetal Neonatal Ed 1999; 81: F99–F104.
Jayasinghe D, Gill AB, Levene MI . CBF reactivity in hypotensive and normotensive preterm infants. Pediatr Res 2003; 54: 848–853.
Pellicer A, Valverde E, Elorza MD, Madero R, Gayá F, Quero J et al. Cardiovascular support for low birth weight infants and cerebral hemodynamics: A randomized, blinded, clinical trial. Pediatrics 2005; 115: 1501–1512.
Bouissou A, Rakza T, Klosowski S, Tourneux P, Vanderborght M, Storme L . Hypotension in preterm infants with significant patent ductus arteriosus: Effects of dopamine. J Pediatr 2008; 153: 790–794.
Wong F, Barfield C, Horne R, Walker A . Dopamine therapy promotes cerebral flow-metabolism coupling in preterm infants. Intensive Care Med 2009; 35: 1777–1782.
Kaiser JR, Gauss CH, Williams DK . Surfactant administration acutely affects cerebral and systemic hemodynamics and gas exchange in very low birth weight infants. J Pediatr 2004; 144: 809–814.
Kaiser JR, Gauss CH, Williams DK . The effects of hypercapnia on cerebral autoregulation in ventilated very low birth weight infants. Pediatr Res 2005; 58: 931–935.
Kaiser JR, Gauss CH, Williams DK . Tracheal suctioning is associated with prolonged disturbances of cerebral hemodynamics in very low birth weight infants. J Perinatol 2008; 28: 34–41.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: A study of infants with birth weights less than 1500 gm. J Pediatr 1978; 92: 529–534.
Joint Working Group of the British Association of Perinatal Medicine and the Research Unit of the Royal College of Physicians. Development of audit measures and guidelines for good practice in the management of neonatal respiratory distress syndrome. Arch Dis Child 1992; 67: 1221–1227.
Pryds O, Greisen G, Lou H, Friis-Hansen B . Heterogeneity of cerebral vasoreactivity in preterm infants supported by mechanical ventilation. J Pediatr 1989; 115: 638–645.
Bada HS, Hajjar W, Chua C, Sumner DS . Noninvasive diagnosis of neonatal asphyxia and intraventricular hemorrhage by Doppler ultrasound. Pediatrics 1979; 5: 775–779.
Romagnoli C, Giannantonio C, De Carolis MP, Gallini F, Zecca E, Papacci P . Neonatal color Doppler US study: normal values of cerebral blood flow velocities in preterm infants in the first month of life. Ultrasound Med Biol 2006; 32: 321–331.
Jorch G, Jorch N . Failure of autoregulation of cerebral blood flow in neonates studied by pulsed Doppler ultrasound of the internal carotid artery. Eur J Pediatr 1987; 146: 468–472.
Lou HC, Lassen NA, Friis-Hansen B . Impaired autoregulation of cerebral blood flow in the distressed newborn infant. J Pediatr 1979; 94: 118–121.
Batton BJ, Li L, Newman NS, Das A, Watterberg KL, Yoder BA et al. Feasibility study of early blood pressure management in extremely preterm infants. J Pediatr 2012; 161 (65–69): e61.
Bassan H, Gauvreau K, Newburger JW, Tsuji M, Limperopoulos C, Soul JS et al. Identification of pressure passive cerebral perfusion and its mediators after infant cardiac surgery. Pediatr Res 2005; 57: 35–41.
Pellicer A, Valverde E, Gayá F, Quero J, Cabañas F . Postnatal adaptation of brain circulation in preterm infants. Pediatr Neurol 2001; 24: 103–109.
Mosca F, Bray M, Lattanzio M, Fumagalli M, Tosetto C . Comparative evaluation of the effects of indomethacin and ibuprofen on cerebral perfusion and oxygenation in preterm infants with patent ductus arteriosus. J Pediatr 1997; 131: 549–554.
Koch J, Hensley G, Roy L, Brown S, Ramaciotti C, Rosenfeld CR . Prevalence of spontaneous closure of the ductus arteriosus in neonates at a birth weight of 1000 grams or less. Pediatrics 2006; 117: 1113–1121.
Perlman JM, McMenamin JB, Volpe JJ . Fluctuating cerebral blood-flow velocity in respiratory-distress syndrome. Relation to the development of intraventricular hemorrhage. N Engl J Med 1983; 309: 204–209.
Acknowledgements
Dr Lightburn was supported by the University of Arkansas for Medical Sciences Children’s University Medical Group. Dr Kaiser was supported by the National Institutes of Health (1K23NS43185, RR20146, and 1R01NS060674) and the University of Arkansas for Medical Sciences Translational Research Institute (1UL1RR029884). The technical assistance of Natalie C Sikes and Melanie J Mason, and the support of the University of Arkansas for Medical Sciences neonatologists, NICU nurses, respiratory therapists and ultrasound technicians, are gratefully appreciated.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This research was presented in part at the Pediatric Academic Society, Society for Pediatric Research meeting in Vancouver, British Columbia, Canada, May 2010.
Rights and permissions
About this article
Cite this article
Lightburn, M., Gauss, C., Williams, D. et al. Observational study of cerebral hemodynamics during dopamine treatment in hypotensive ELBW infants on the first day of life. J Perinatol 33, 698–702 (2013). https://doi.org/10.1038/jp.2013.44
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2013.44
Keywords
This article is cited by
-
Prevention of severe brain injury in very preterm neonates: A quality improvement initiative
Journal of Perinatology (2022)
-
Neonatal Hypotension: What Is the Efficacy of Each Anti-Hypotensive Intervention? A Systematic Review
Current Treatment Options in Pediatrics (2019)
-
Dopamine
Reactions Weekly (2014)