Abstract
Background:
Studies of outcomes of preterm infants after the receipt of extensive cardiopulmonary resuscitation (CPR) at birth have yielded varied results.
Objective:
To compare adverse outcome (death or severe morbidities) of preterm infants <32 weeks gestational age (GA) who received chest compressions with or without administration of epinephrine at birth with those who did not receive either.
Design/Method:
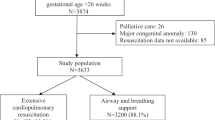
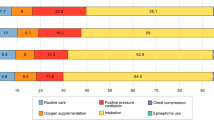
Data were retrospectively analyzed from a database for preterm infants <32 weeks GA discharged from hospital between July 2004 and October 2007. Cases: Infants who received chest compression with or without administration of epinephrine during the initial resuscitation. Matched cohort: Infants who did not receive extensive CPR at birth (matched for GA, sex and admission date). Primary outcome: Death or any of three severe morbidities (grade 3 or 4 intraventricular hemorrhage or periventricular leukomalacia; retinopathy of prematurity > stage 2 or chronic lung disease).
Result:
Sixty-six cases and 156 matched infants were identified. There were no baseline differences between groups except Apgar and severity of illness scores. Median (interquartile range) duration for chest compression (n=66) was 60 (30 to 180 s) and number of epinephrine doses (n=29) was 1 (1 to 3). Logistic regression confirmed significantly higher risk of adverse outcome among cases compared with matched controls (58 vs 37%; P=0.04, adjusted odds ratio 2.23, 95% confidence interval 1.04, 4.77).
Conclusion:
Infants born prematurely who met criteria for extensive CPR at birth experienced higher risk of combined adverse outcome, including death or severe neurological injury, severe retinopathy of prematurity or bronchopulmonary dysplasia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
International Liaison Committee on Resuscitation. The International Liaison Committee on Resuscitation (ILCOR) consensus on science with treatment recommendations for pediatric and neonatal patients: neonatal resuscitation. Pediatrics 2006; 117 (5): e978–e988.
Niermeyer S, Kattwinkel J, Van Reempts P, Nadkarni V, Phillips B, Zideman D et al. International Guidelines for Neonatal Resuscitation: an excerpt from the Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care: International Consensus on Science. Contributors and Reviewers for the Neonatal Resuscitation Guidelines. Pediatrics 2000; 106 (3): E29.
Finer NN, Horbar JD, Carpenter JH . Cardiopulmonary resuscitation in the very low birth weight infant: the Vermont Oxford Network experience. Pediatrics 1999; 104 (3 Pt 1): 428–434.
Deulofeut R, Sola A, Lee B, Rogido M . Delivery room cardiopulmonary resucitation of very preterm infant is associated with adverse short- and long-term outcomes. An Pediatr (Barc) 2007; 66 (1): 31–37.
Jankov RP, Asztalos EV, Skidmore MB . Favourable neurological outcomes following delivery room cardiopulmonary resuscitation of infants < or=750 g at birth. J Paediatr Child Health 2000; 36 (1): 19–22.
Sanchez-Torres AM, Garcia-Alix A, Cabanas F, Elorza MD, Madero R, Perez J et al. Impact of cardiopulmonary resuscitation on extremely low birth weight infants. An Pediatr (Barc) 2007; 66 (1): 38–44.
Lantos JD, Miles SH, Silverstein MD, Stocking CB . Survival after cardiopulmonary resuscitation in babies of very low birth weight. Is CPR futile therapy? N Engl J Med 1988; 318 (2): 91–95.
Finer NN, Tarin T, Vaucher YE, Barrington K, Bejar R . Intact survival in extremely low birth weight infants after delivery room resuscitation. Pediatrics 1999; 104 (4): e40.
Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M et al. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics 2001; 108 (2): E35.
The CRIB (clinical risk index for babies) score: a tool for assessing initial neonatal risk and comparing performance of neonatal intensive care units. The International Neonatal Network. Lancet. 342 (8865): 193–198.
Lee SK, Zupancic JA, Pendray M, Thiessen P, Schmidt B, Whyte R et al. Transport risk index of physiologic stability: a practical system for assessing infant transport care. J Pediatr 2001; 139 (2): 220–226.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM . Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics 1988; 82 (4): 527–532.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 g. J Pediatr 1978; 92 (4): 529–534.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg 1978; 187 (1): 1–7.
Sims DG, Heal CA, Bartle SM . Use of adrenaline and atropine in neonatal resuscitation. Arch Dis Child Fetal Neonatal Ed 1994; 70 (1): F3–F9.
Davis DJ . How aggressive should delivery room cardiopulmonary resuscitation be for extremely low birth weight neonates? Pediatrics 1993; 92 (3): 447–450.
Schmidt B, Asztalos EV, Roberts RS, Robertson CM, Sauve RS, Whitfield MF . Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months: results from the trial of indomethacin prophylaxis in preterms. JAMA 2003; 289 (9): 1124–1129.
Jefferies AL, Kelly EN . Need for resuscitation at birth does not predict outcome for very preterm infants. Pediatr Res 1994; 35: 274A.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shah, P., Shah, P. & Tai, K. Chest compression and/or epinephrine at birth for preterm infants <32 weeks gestational age: matched cohort study of neonatal outcomes. J Perinatol 29, 693–697 (2009). https://doi.org/10.1038/jp.2009.70
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2009.70
Keywords
This article is cited by
-
Neonatal resuscitation with continuous chest compressions and high frequency percussive ventilation in preterm lambs
Pediatric Research (2024)
-
Outcomes of neonates born at <26 weeks gestational age who receive extensive cardiopulmonary resuscitation compared with airway and breathing support
Journal of Perinatology (2020)
-
Do transport factors increase the risk of severe brain injury in outborn infants <33 weeks gestational age?
Journal of Perinatology (2020)
-
The SURV1VE trial—sustained inflation and chest compression versus 3:1 chest compression-to-ventilation ratio during cardiopulmonary resuscitation of asphyxiated newborns: study protocol for a cluster randomized controlled trial
Trials (2019)
-
Current Challenges in Neonatal Resuscitation: What is the Role of Adrenaline?
Pediatric Drugs (2018)