Abstract
Objective:
A majority of the modalities of synchronized ventilation in preterm infants require the use of flow sensors that can increase dead space and may adversely affect ventilator weaning. The objective of this study was to assess the effects of flow sensor dead space during synchronized intermittent mandatory ventilation (SIMV) weaning in preterm infants.
Study Design:
Twelve preterm infants (gestational age 25±2 weeks, birth weight 705±158 g, age: 31±186 days, SIMV rate: 25±8 breaths min–1, peak inspiratory pressure 18±2 cm H2O, positive end-expiratory pressure: 5±0.5 cm H2O, pressure support: 9±3 cm H2O, fraction of inspired oxygen: 34±6%) underwent two 2.5-h weaning periods during which SIMV rate was reduced twice by 5 breaths min–1 at 30-min intervals as tolerated, with and without reduction of flow sensor dead space, in random sequence. A 30-min baseline was obtained before each weaning period. Dead space was reduced by flushing the flow sensor with a continuous gas leak flow in the endotracheal tube connector.
Result:
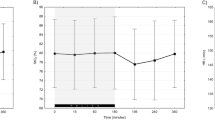
Transcutaneous CO2 tension during SIMV weaning periods without and with reduced dead space did not differ from baseline, whereas total minute ventilation and tidal volume were lower during the SIMV weaning period with reduced dead space. Three infants did not tolerate SIMV weaning without while one infant did not tolerate weaning with reduced dead space.
Conclusion:
SIMV weaning elicited a compensatory rise in spontaneous ventilation. When flow sensor dead space was reduced during SIMV weaning, gas exchange was maintained with lower minute ventilation. Instrumental dead space imposes a ventilatory burden during SIMV weaning in small preterm infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Hummler H, Gerhardt T, Gonzalez A, Claure N, Everett R, Bancalari E . Influence of different methods of synchronized mechanical ventilation on ventilation, gas exchange, patient effort and blood pressure fluctuations in premature neonates. Pediatr Pulmonol 1996; 22: 305–313.
Bernstein G, Mannino FL, Heldt GP, Callahan JD, Bull DH, Sola A et al. Randomized multicenter trial comparing synchronized and conventional intermittent mandatory ventilation in neonates. J Pediatr 1996; 128: 453–463.
Chan V, Greenough A . Randomised controlled trial of weaning by patient triggered ventilation or conventional ventilation. Eur J Pediatr 1993; 152: 51–54.
Donn SM, Nicks JJ, Becker MA . Flow-synchronized ventilation of preterm infants with respiratory distress syndrome. J Perinatol 1994; 14: 90–94.
Chen J-Y, Ling U-P, Chen J-H . Comparison of synchronized and conventional intermittent mandatory ventilation in neonates. Acta Paediatr Japonica 1997; 39: 578–583.
Figueras J, Rodriguez-Miguelez JM, Botet F, Thio M, Jimenez R . Changes in TcPCO2 regarding pulmonary mechanics due to pneumotachometer dead space in ventilated newborns. J Perinat Med 1997; 25: 333–339.
Claure N, D'Ugard C, Bancalari E . Elimination of ventilator dead space during synchronized ventilation in premature infants. J Pediatr 2003; 143: 315–320.
Numa AH, Newth CJ . Anatomic dead space in infants and children. J Appl Physiol 1996; 80: 1485–1489.
Danan C, Dassieu G, Janaud JC, Brochard L . Efficacy of dead-space washout in mechanically ventilated premature newborns. Am J Respir Crit Care Med 1996; 153: 1571–1576.
Nassabeh-Montazami S, Abubakar KM, Keszler M . The impact of instrumental dead-space in volume-targeted ventilation of the extremely low birth weight (ELBW) infant. Pediatr Pulmonol 2009; 44: 128–133.
Greenough A, Milner AD, Dimitriou G . Synchronized mechanical ventilation for respiratory support in newborn infants. Cochrane Database Syst Rev 2004; CD000456.
Chow LC, Vanderhal A, Raber J, Sola A . Are tidal volume measurements in neonatal pressure-controlled ventilation accurate? Pediatr Pulmonol 2002; 34: 196–202.
Cannon ML, Cornell J, Tripp-Hamel DS, Gentile MA, Hubble CL, Meliones JN et al. Tidal volumes for ventilated infants should be determined with a pneumotachometer placed at the endotracheal tube. Am J Respir Crit Care Med 2000; 162: 2109–2112.
Acknowledgements
The study was supported by the University of Miami ‘Project: New Born’ and The Bank of America Charitable Foundation. This study was presented in part at the 2007 meeting of the Society for Pediatric Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Drs Claure and Bancalari have a patent unrelated to the material in the present paper. The University of Miami, the assignee for this patent, has a licensing agreement with Cardinal Health, the manufacturer of the ventilators used in this study. Cardinal Health did not support the study or participate in its design, conduction and reporting.
Rights and permissions
About this article
Cite this article
Estay, A., Claure, N., D'Ugard, C. et al. Effects of instrumental dead space reduction during weaning from synchronized ventilation in preterm infants. J Perinatol 30, 479–483 (2010). https://doi.org/10.1038/jp.2009.187
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2009.187
Keywords
This article is cited by
-
Diaphragmatic activity and neural breathing variability during a 5-min endotracheal continuous positive airway pressure trial in extremely preterm infants
Pediatric Research (2021)
-
Deadspace ventilation: a waste of breath!
Intensive Care Medicine (2011)