Abstract
Objective:
Identifying a platelet count as abnormal (thrombocytopenia or thrombocytosis) can facilitate recognizing various disease states. However, the published reference ranges for platelet counts in neonates may be imprecise, as they were generated from relatively small sample sizes and compiled before modern platelet enumeration methods.
Study design:
We derived new neonatal reference ranges for platelet counts and mean platelet volume (MPV) measurements using electronic data accumulated during a recent 6-year period from a multihospital healthcare system.
Result:
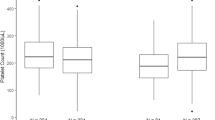
Platelet counts were obtained between the first and the 90th day after birth, from 47 291 neonates delivered at 22 to 42 weeks gestation. The first platelet counts obtained in the first 3 days of life, increased over the range of 22 to 42 weeks gestation. In those born ⩽32 weeks gestation, the lower reference range (5th percentile) was 104 200 μl−1, but it was 123 100 μl−1 in late-preterm and -term neonates. Advancing postnatal age had a significant effect on platelet counts; during the first 9 weeks, the counts fit a sinusoidal pattern with two peaks; one at 2 to 3 weeks and a second at 6 to 7 weeks. The upper limit of expected counts (95th percentile) during these peaks were as high as 750 000 μl−1.
Conclusion:
The figures herein describe reference ranges for platelet counts and MPV determinations of neonates at various gestational ages during their first 90 days. Expected values differ substantially from the 150 000 μl−1 to 450 000 μl−1 range previously used to define neonatal thrombocytopenia and thrombocytosis. The new definitions will render the diagnoses of neonatal thrombocytopenia and thrombocytosis less commonly than when the old definitions were used, because the new ranges are wider than 150 000 μl−1 to 450 000 μl−1.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Sola MC . Evaluation and treatment of severe and prolonged thrombocytopenia in neonates. Clin Perinatol 2004; 31 (1): 1–14.
McPherson RJ, Juul S . Patterns of thrombocytosis and thrombocytopenia in hospitalized neonates. J Perinatol 2005; 25 (3): 166–172.
Henry E, Walker D, Wiedmeier SE, Christensen RD . Hematological abnormalities during the first week of life among neonates with Down syndrome: data from a multihospital healthcare system. Am J Med Genet A 2007; 143 (1): 42–50.
O’Shea J, Sherlock M, Philip R . Thrombocytosis in childhood. Acta Haematol 2005; 113 (3): 212.
Nakayama H, Ihara K, Hikino S, Yamamoto J, Nagatomo T, Takemoto M et al. Thrombocytosis in preterm infants: a possible involvement of thrombopoietin receptor gene expression. J Mol Med 2005; 83 (4): 316–320.
Sutor AH . Thrombocytosis in childhood. Semin Thromb Hemost 1995; 21 (3): 330–339.
Sekhon SS, Roy V . Thrombocytopenia in adults: a practical approach to evaluation and management. S Med J 2006; 99: 491–497.
Christensen RD . Expected hematologic values for term and preterm neonates. In: Christensen RD (ed). Hematologic Problems of the Neonate. WB Saunders Co.: Philadelphia, 2000, pp 120–122.
Chakravorty S, Murray N, Roberts I . Neonatal thrombocytopenia. Early Hum Dev 2005; 81 (1): 35–41.
Haque KN, Bahakim HM . Percentile curves for various hematologic measurements at birth in Arab preterm babies of different gestational ages. AJDC 1991; 145: 645–649.
Thurlbeck SM, McIntosh N . Preterm blood counts vary with sampling site. Arch Dis Child 1987; 62: 74–75.
Appleyard WJ, Brinton A . Venous platelet counts in low birth weight infants. Biol Neonate 1971; 17: 30–34.
Bourner G, Dhaliqai J, Sumner J . Performance evaluation of the latest fully automated hematology analyzers in a large, commercial laboratory setting: a 4-way, side-by-side study. Lab Hematol 2005; 11: 285–297.
Christensen RD, Henry E, Wiedmeier SE, Stoddard RA, Sola-Visner MC, Lambert DK et al. Thrombocytopenia among extremely low birth weight neonates: data from a multihospital healthcare system. J Perinatol 2006; 26 (6): 348–353.
Arad ID, Alpan G, Sznajderman SD, Eldor A . The mean platelet volume (MPV) in the neonatal period. Am J Perinatol 1986; 3 (1): 1–3.
Hathaway WE, Bonnar J . Perinatal Coagulation. Grune and Stratton: New York, 1978.
Kaushansky K, Roth GJ . Platelets and megakaryocytes. In: Greer JP, Forester J, Luken J, Rodgers GM, Paraskevas F, Glader B (eds). Wintrobe's Clinical Hematology. Lippincott Williams & Wilkins: Philadelphia, PA, 2004, pp 605–650.
Van den Hof MC, Nicolaides KH . Platelet count in normal, small, and anemic fetuses. Am J Obstet Gynecol 1990; 162 (3): 735–739.
Forestier F, Daffos F, Galacteros F, Bardakjian J, Rainaut M, Beuzard Y . Hematological values of 163 normal fetuses between 18 and 30 weeks of gestation. Pediatr Res 1986; 20 (4): 342–346.
Forestier F, Daffos F, Catherine N, Renard M, Andreux J-P . Developmental hematopoiesis in normal human fetal blood. Blood 1991; 77 (11): 2360–2363.
Hohlfeld P, Forestier F, Kaplan C, Tissot J-D, Daffos F . Fetal thrombocytopenia: a retrospective survey of 5,194 fetal blood samplings. Blood 1994; 84 (6): 1851–1856.
Aballi AJ, Puapondh Y, Desposito F . Platelet counts in thriving premature infants. Pediatrics 1968; 42: 685–689.
Sell EJ, Corrigan Jr JJ . Platelet counts, fibrinogen concentrations, and factor V and factor VIII levels in healthy infants according to gestational age. J Pediatr 1973; 82: 1028–1032.
Obladen M, Diepold K, Maier RF . Venous and arterial hematologic profiles of very low birth weight infants. European Multicenter rhEPO Study Group. Pediatrics 2000; 106 (4): 707–711.
Sasanakul W, Singalavanija S, Hathirat P, Mahaphan W, Chuansumrit A . Hemogran in normal newborn babies with special reference to platelet count. Southeast Asian J Trop Med Public Health 1993; 24 (Suppl 1): 237–240.
Appleyard WJ, Brinton A . Venous platelet counts in low birth weight infants. Biol Neonate 1971; 17: 30–34.
Matsubara K, Baba K, Nigami H, Harigaya H, Ishiguro A, Kato T et al. Early elevation of serum thrombopoietin levels and subsequent thrombocytosis in healthy preterm infants. Br J Haematol 2001; 115: 963–968.
Saxonhouse MA, Sola MC, Pastos KM, Ignatz ME, Hutson AD, Christensen RD et al. Reticulated platelet percentages in term and preterm neonates. J Pediatr Hematol Oncol 2004; 26 (12): 797–802.
Kaushansky K . Thrombopoietin. N Engl J Med 1998; 339: 746–754.
Walka MM, Sonntag J, Dudenhausen JW, Obladen M . Thrombopoietin concentrations in umbilical cord of healthy term newborns is higher than in adult controls. Biol Neonate 1999; 75 (1): 54–58.
Sola MC, Juul SE, Meng YG, Garg S, Sims P, Calhoun DA et al. Thrombopoietin (Tpo) in the fetus and neonate: Tpo concentration in preterm and term neonates, and organ distribution of Tpo and its receptor (c-mpl) during human fetal development. Early Hum Dev 1999; 53 (3): 239–250.
Ishiguro A, Nakahata T, Matsubara K, Hayashi Y, Kato T, Suzuki Y et al. Age-related changes in thrombopoietin levels. Br J Haematol 1999; 106: 884–888.
Sola MC, Christensen RD, Hutson AD, Tarantal AF . Pharmacokinetics, pharmacodynamics, and safety of administering pegylated recombinant megakaryocyte growth and development factor to newborn rhesus monkeys. Pediatr Res 2000; 47 (2): 208–214.
Dame C, Sutor AH . Primary and secondary thrombocytosis in childhood. Br J Haematol 2005; 129: 165–177.
Ohls RK . Evaluation and treatment of anemia in the neonate. In: Christensen RD (ed). Hematologic Problems of the Neonate. WB Saunders Co.: Philadelphia, 2000, pp 137–138.
Karpatkin S . Heterogeneity of human platelets. I. Metabolic and kinetic evidence suggestive of young and old platelets. J Clin Invest 1969; 48 (6): 1073–1082.
Karpatkin S . Heterogeneity of human platelets. II. Functional evidence of young and old platelets. J Clin Invest 1969; 48 (6): 1083–1087.
Karpatkin S . Heterogeneity of human platelets. VI. Correlation of platelet function with platelet volume. Blood 1978; 51: 307–314.
Corash L, Tan H, Gralmick HR . Heterogeneity of human whole blood platelet subpopulations. I. Relationship between buoyant density, cell volume, and ultrastructure. Blood 1977; 49: 71–87.
Thompson CB, Love DG, Quinn PG, Valeri CR . Platelet size does not correlate with platelet age. Blood 1983; 62 (2): 487–494.
Thompson CB, Jakubowski JA, Quinn PG, Deykin D, Valeri CR . Platelet size and age determine platelet function independently. Blood 1984; 63 (6): 1372–1375.
Thompson CB, Jakubowski JA . The pathophysiology and clinical relevance of platelet heterogeneity. Blood 1988; 72 (1): 1–8.
Martin JF, Bath PMW . Influence of platelet size on outcome after myocardial infarction. Lancet 1991; 338 (8780): 1409–1411.
Endler G, Klimesch A, Sunder-Plassmann H . Mean platelet volume is an independent risk factor for myocardial infarction but not for coronary artery disease. Br J Haematol 2002; 117: 399–404.
Bath P, Algert C, Chapman N, Neal B, PROGRESS Collaborative Group. Association of mean platelet volume with risk of stroke among 3134 individuals with history of cerebrovascular disease. Stroke 2004; 35: 622–626.
Park Y, Schoene N, Harris W . Mean platelet volume as an indicator of platelet activation: methodological issues. Platelets 2002; 13: 301–306.
Patrick CH, Lazarchick J . The effect of bacteremia on automated platelet measurements in neonates. Am J Clin Pathol 1990; 93 (3): 391–394.
Beverley DW, Inwood MJ, Chance GW, Schaus M, O’Keefe B . ‘Normal’ haemostasis parameters: a study in a well-defined inborn population of preterm infants. Early Hum Dev 1984; 9 (3): 249–257.
Kipper SL, Sieger L . Whole blood platelet volumes in newborn infants. J Pediatr 1982; 101 (5): 763–766.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wiedmeier, S., Henry, E., Sola-Visner, M. et al. Platelet reference ranges for neonates, defined using data from over 47 000 patients in a multihospital healthcare system. J Perinatol 29, 130–136 (2009). https://doi.org/10.1038/jp.2008.141
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2008.141
Keywords
This article is cited by
-
Neonatal hematological parameters: the translational aspect of developmental hematopoiesis
Annals of Hematology (2023)
-
Capillary blood reference intervals for platelet parameters in healthy full-term neonates in China
BMC Pediatrics (2020)
-
Hematological reference intervals among full-term newborns in Ethiopia: a cross-sectional study
BMC Pediatrics (2020)
-
Erythropoietin prevents necrotizing enterocolitis in very preterm infants: a randomized controlled trial
Journal of Translational Medicine (2020)
-
Impaired platelet activity and hypercoagulation in healthy term and moderately preterm newborns during the early neonatal period
Pediatric Research (2019)