Abstract
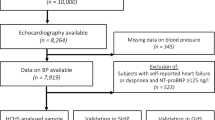
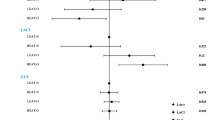
Reduced myocardial mechano-energetic efficiency (MEE), estimated as stroke volume/heart rate ratio per g of left ventricular (LV) mass (LVM), and expressed in μl s−1 g−1 (MEEi), is a strong predictor of cardiovascular (CV) events, independently of LV hypertrophy and other confounders, including type II diabetes (DM). Decreased MEEi is more frequent in patients with diabetes. In the present analysis we evaluated the interrelation among MEEi, DM and metabolic syndrome (MetS) in the setting of arterial hypertension. Hypertensive patients from the Campania Salute Network, free of prevalent CV disease and with ejection fraction >50% (n=12 503), were analysed. Coexistence of MetS and DM was ordinally categorized into 4 groups: 8235 patients with neither MetS nor DM (MetS−/DM−); 502 without MetS and with DM (MetS−/DM+); 3045 with MetS and without DM (MetS+/DM−); and 721 with MetS and DM (MetS+/DM+). After controlling for sex, systolic blood pressure, body mass index, relative wall thickness (RWT), antihypertensive medications and type of antidiabetic therapy, MEEi was 333 μl s−1 g−1 in MetS−/DM−, 328 in MetS−/DM+, 326 in MetS+/DM− and 319 in MetS+/DM+ (P for trend <0.0001). In pairwise comparisons (Sidak-adjusted), all conditions, except MetS−/DM+, were significantly different from MetS−/DM− (all P<0.02). No statistical difference was detected between MetS−/DM+ and MetS+/DM−. Both MetS and DM are associated with decreased MEEi in hypertensive patients, independently to each other, but the reduction is statistically less evident for MetS−/DM+. MetS+/DM+ patients have the lowest levels of MEEi, consistent with the alterations of energy supply associated with the combination of insulin resistance with insulin deficiency.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Change history
03 May 2016
This article has been corrected since Advance Online Publication, and a corrigendum is also printed in this issue.
References
Braunwald E . Control of myocardial oxygen consumption: physiologic and clinical considerations. Am J Cardiol 1971; 27 (4): 416–432.
Suga H . Ventricular energetics. Physiol Rev 1990; 70: 247–277.
Kolwicz SC Jr, Purohit S, Tian R . Cardiac metabolism and its interactions with contraction, growth, and survival of cardiomyocytes. Circ Res 2013; 113 (5): 603–616.
Lopaschuk GD, Ussher JR, Folmes CD, Jaswal JS, Stanley WC . Myocardial fatty acid metabolism in health and disease. Physiol Rev 2010; 90: 207–258.
de Simone G, Chinali M, Galderisi M, Benincasa M, Girfoglio D, Botta I et al. Myocardial mechano-energetic efficiency in hypertensive adults. J Hypertens 2009; 27 (3): 650–655.
Rijzewijk LJ, van der Meer RW, Lamb HJ, de Jong HW, Lubberink M, Romijn JA et al. Altered myocardial substrate metabolism and decreased diastolic function in nonischemic human diabetic cardiomyopathy: studies with cardiac positron emission tomography and magnetic resonance imaging. J Am Coll Cardiol 2009; 54 (16): 1524–1532.
Korvald C, Elvenes OP, Myrmel T . Myocardial substrate metabolism influences left ventricular energetics in vivo. Am J Physiol Heart Circ Physiol 2000; 278 (4): H1345–H1351.
de Simone G, Izzo R, Losi MA, Stabile E, Rozza F, Canciello G et al. Depressed myocardial energetic efficiency is associated with increased cardiovascular risk in hypertensive left ventricular hypertrophy. J Hypertens 2016; 34 (9): 1846–1853.
Losi MA, Izzo R, De Marco M, Canciello G, Rapacciuolo A, Trimarco V et al. Cardiovascular ultrasound exploration contributes to predict incident atrial fibrillation in arterial hypertension: the Campania Salute Network. Int J Cardiol 2015; 199: 290–295.
America Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2007; 30 (Suppl 1): S42–S47.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005; 112 (17): 2735–2752.
De Marco M, de Simone G, Izzo R, Mancusi C, Sforza A, Giudice R et al. Classes of antihypertensive medications and blood pressure control in relation to metabolic risk factors. J Hypertens 2012; 30 (1): 188–193.
Izzo R, de Simone G, Trimarco V, Gerdts E, Giudice R, Vaccaro O et al. Hypertensive target organ damage predicts incident diabetes mellitus. Eur Heart J 2013; 34 (44): 3419–3426.
de Simone G, Arnett DK, Chinali M, De Marco M, Rao DC, Kraja AT et al. Partial normalization of components of metabolic syndrome does not influence prevalent echocardiographic abnormalities: the HyperGEN study. Nutr Metab Cardiovasc Dis 2013; 23 (1): 38–45.
Mancia G, Schumacher H, Redon J, Verdecchia P, Schmieder R, Jennings G et al. Blood pressure targets recommended by guidelines and incidence of cardiovascular and renal events in the Ongoing Telmisartan Alone and in Combination WithRamipril Global Endpoint Trial (ONTARGET). Circulation 2011; 124 (16): 1727–1736.
Izzo R, de Simone G, Devereux RB, Giudice R, De Marco M, Cimmino CS et al. Initial left-ventricular mass predicts probability of uncontrolled blood pressure in arterial hypertension. J Hypertens 2011; 29: 803–808.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA et al. Recommendations for chamber quantification quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the EAE a brach of the ESC. J Am Soc Echocardiogr 2005; 18: 1440–1463.
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 1986; 57: 450–458.
de Simone G, Daniels SR, Devereux RB, Meyer RA, Roman MJ, de Divitiis O et al. Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol 1992; 20: 1251–1260.
de Simone G, Izzo R, Aurigemma GP, De Marco M, Rozza F, Trimarco V et al. Cardiovascular risk in relation to a new classification of hypertensive left ventricular geometric abnormalities. J Hypertens 2015; 33: 745–754.
de Simone G, Devereux RB, Ganau A, Hahn RT, Saba PS, Mureddu GF et al. Estimation of left venventricular chamber and stroke volume by limited M-mode echocardiography and validation by two-dimensional and Doppler echocardiography. Am J Cardiol. 1996; 78: 801–807.
de Simone G, Devereux RB, Daniels SR, Mureddu G, Roman MJ, Kimball TR et al. Stroke volume and cardiac output in normotensive children and adults. Assessment of relations with body size and impact of overweight. Circulation 1997; 95: 1837–1843.
de Simone G, Devereux RB, Kimball TR, Mureddu GF, Roman MJ, Contaldo F et al. Interaction between body size and cardiac workload: influence on left ventricular mass during body growth and adulthood. Hypertension 1998; 31: 1077–1082.
Vanoverschelde JL, Wijns W, Essamri B, Bol A, Robert A, Labar D et al. Hemodynamic and mechanical determinants of myocardial O2 consumption in normal human heart: effects of dobutamine. Am J Physiol 1993; 265: H1884–H1892.
Howard BV, Best LG, Galloway JM, Howard WJ, Jones K, Lee ET et al. Coronary heart disease risk equivalence in diabetes depends on concomitant risk factors. Diabetes Care 2006; 29 (2): 391–397.
Barnard J, Meng XL . Applications of multiple imputation in medical studies: from AIDS to NHANES. Stat Methods Med Res 1999; 8 (1): 17–36.
Mazumder PK, O'Neill BT, Roberts MW, Buchanan J, Yun UJ, Cooksey RC et al. Impaired cardiac efficiency and increased fatty acid oxidation in insulin-resistant ob/ob mouse hearts. Diabetes 2004; 53 (9): 2366–2374.
Peterson LR, Herrero P, Schechtman KB, Racette SB, Waggoner AD, Kisrieva-Ware Z et al. Effect of obesity and insulin resistance on myocardial substrate metabolism and efficiency in young women. Circulation 2004; 109 (18): 2191–2196.
Ferrannini E . Insulin resistance versus insulin deficiency in non-insulin-dependent diabetes mellitus: problems and prospects. Endocr Rev 1998; 19 (4): 477–490.
D'Andrea A, Nistri S, Castaldo F, Galderisi M, Mele D, Agricola E et al. The relationship between early left ventricular myocardial alterations and reduced coronary flow reserve in non-insulin-dependent diabetic patients with microvascular angina. Int J Cardiol 2012; 154 (3): 250–255.
Zhang Y, Lee ET, Howard BV, Best LG, Umans JG, Yeh J et al. Insulin resistance, incident cardiovascular diseases, and decreased kidney function among nondiabetic American Indians: the Strong Heart Study. Diabetes Care 2013; 36 (10): 3195–3200.
Ingelsson E, Sundström J, Arnlöv J, Zethelius B, Lind L . Insulin resistance and risk of congestive heart failure. JAMA 2005; 294 (3): 334–341.
Aasum E, Hafstad AD, Severson DL, Larsen TS . Age-dependent changes in metabolism, contractile function, and ischemic sensitivity in hearts from db/db mice. Diabetes 2003; 52: 434–441.
Hinkle PC . P/O ratios of mitochondrial oxidative phosphorylation. Biochim Biophys Acta 2005; 1706: 1–11.
Aurigemma GP, Zile MR, Gaasch WH . Contractile behavior of the left ventricle in diastolic heart failure: with emphasis on regional systolic function. Circulation 2006; 113 (2): 296–304.
Acknowledgements
We thank the nurses Nino Battaglia, Carmela Cristiano, Pietro Di Leo and Pasquale Esposito for their invaluable support in the patients’ management, and their coordinator Anna Vitiello.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Mancusi, C., Losi, M., Izzo, R. et al. Effect of diabetes and metabolic syndrome on myocardial mechano-energetic efficiency in hypertensive patients. The Campania Salute Network. J Hum Hypertens 31, 395–399 (2017). https://doi.org/10.1038/jhh.2016.88
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2016.88
This article is cited by
-
Mechano-energetic efficiency in patients with hypertrophic cardiomyopathy with and without sarcomeric mutations
Journal of Cardiovascular Translational Research (2023)
-
Assessment of carotid cross-sectional area in hypertensive patients: phenotyping and prognostic validation in The Campania Salute Network
Journal of Human Hypertension (2021)
-
Covariables of Myocardial Function in Women and Men with Increased Body Mass Index
High Blood Pressure & Cardiovascular Prevention (2020)
-
Insulin Resistance the Hinge Between Hypertension and Type 2 Diabetes
High Blood Pressure & Cardiovascular Prevention (2020)
-
Myocardial mechano-energetic efficiency and insulin resistance in non-diabetic members of the Strong Heart Study cohort
Cardiovascular Diabetology (2019)