Abstract
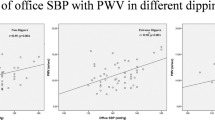
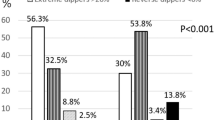
The clinical relevance of nocturnal hypertension (NH) in comparison with non-dipping status has not been clarified yet, as regards subclinical target organ damage. We aimed to elucidate whether NH or dipping status reflects better organ damage. The study population included 319 newly diagnosed hypertensive patients. Subclinical organ damage was evaluated to all participants. On the basis of nocturnal blood pressure (BP) levels the population was divided into two groups: NH and nocturnal normotension. Also, individuals were defined as dippers and non-dippers according to systolic BP fall. Patients with NH were characterized by increased arterial pulse wave velocity (PWV; 9.1±1.7 vs 8.4±1.5 m s−1, P=0.0001) and carotid intima-media thickness (0.77±0.18 vs 0.69±0.15 mm, P=0.016) compared with normotensive subjects. Notably, they also exhibited higher values of left ventricular mass index (88.1±22.9 vs 82.8±16.6 g m−2 P=0.043). On the contrary, non-dipping status was associated only with differences in PWV (9.26±0.2 vs 8.64±0.2 m s−1, P=0.031, 8) and in creatinine clearance (95±3 vs 106±4, P=0.025) in the group of NH. The presence of NH is accompanied by subclinical atherosclerosis, as well as structural abnormalities of the left ventricle. Therefore, NH rather than non-dipping status could be preferably integrated with the risk of organ damage.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL et al. Seventh report of the Joint National Committee on prevention, detection, evaluation and treatment of high blood pressure. Hypertension 2003; 42: 1206–1252.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G et al. 2007 Guidelines for the Management of Arterial Hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105–1187.
Verdecchia P . Prognostic value of ambulatory blood pressure: current evidence and clinical implications. Hypertension 2000; 35: 844–851.
Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension 2008; 51: 55–61.
Routledge F, McFetridge-Durdle J . Nondipping blood pressure patterns among individuals with essential hypertension: a review of the literature. Eur J Cardiovasc Nurs 2007; 6: 9–26.
Liu M, Takahashi H, Morita Y, Maruyama S, Mizuno M, Yuzawa Y et al. Non-dipping is a potent predictor of cardiovascular mortality and is associated with autonomic dysfunction I haemodialysis patients. Nephrol Dial Transplant 2003; 18: 563–569.
Rahman M, Griffin V, Heyka R, Hoit B . Diurnal variation of blood pressure; reproducibility and association with left ventricular hypertrophy in hemodialysis patients. Blood Press Monit 2005; 10: 25–32.
Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA . Predictive role of the nighttime blood pressure. Hypertension 2011; 57: 3–10.
Xu T, Zhang Y, Tan X . Estimate of nocturnal blood pressure and detection of non-dippers based on clinical or ambulatory monitoring in the inpatient setting. BMC Cardiovasc Disord 2013; 13: 37.
Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M et al2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31: 1281–1357.
Devereux RB, Reichek N . Echocardiographic determination of left ventricular mass in man: anatomic validation of the method. Circulation 1997; 55: 613–619.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005; 18: 1440–1463.
Tousoulis D, Antoniades C, Stefanadis C . Evaluating endothelial function in humans: a guide to invasive and non-invasive techniques. Heart 2005; 91: 553–558.
Cooney MT, Dudina A, Graham I . SCORE and HeartScore coordinating centres. HeartScore predicts surrogate markers of cardiovascular disease in individuals aged below 40 years. Eur J Cardiovasc Prev Rehabil 2009; 16: 513.
Cuspidi C, Meani S, Salerno M, Valerio C, Fusi V, Severgnini B et al. Cardiovascular target organ damage in essential hypertensives with or without reproducible nocturnal fall in blood pressure. J Hypertens 2004; 22: 273–280.
Kikuya M, Ohkubo T, Asayama K, Metoki H, Obara T, Saito S et al. Ambulatory blood pressure and 10-year risk of cardiovascular and noncardiovascular mortality: the Ohasama study. Hypertension 2005; 45: 240–245.
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet 2007; 370: 1219–1229.
Tsioufis C, Andrikou I, Thomopoulos C, Petras D, Manolis A, Stefanadis C . Comparative prognostic role of nighttime blood pressure and nondipping profile on renal outcomes. Am J Nephrol 2011; 33: 277–288.
Chatzistamatiou EI, Moustakas GN, Veioglanis S, Papoutsis D, Memo G, Tsioufis C et al. Nocturnal hypertension: poor correlation with office blood pressure but strong prognostic factor for target organ damage. Hellenic J Cardiol 2012; 53: 263–272.
Tsioufis C, Syrseloudis D, Dimitriadis K, Thomopoulos C, Tsiachris D, Pavlidis P et al. Disturbed circadian blood pressure rhythm and C-reactive protein in essential hypertension. J Hum Hypertens 2008; 22: 501–508.
de la Sierra A, Redon J, Banegas JR, Segura J, Parati G, Gorostidi M et al. Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension 2009; 53: 466–472.
Cuspidi C, Macca G, Sampieri L, Fusi V, Severgnini B, Michev I et al. Target organ damage and non-dipping pattern defined by two sessions of ambulatory blood pressure monitoring in recently diagnosed essential hypertensive patients. J Hypertens 2001; 19: 1539–1545.
Cuspidi C, Lonati L, Sampieri L, Macca G, Valagussa L, Zaro T et al. Impact of nocturnal fall in blood pressure on early cardiovascular changes in essential hypertension. J Hypertens 1999; 17: 1339–1344.
Cuspidi C, Giudici V, Negri F, Sala C . Nocturnal nondipping and left ventricular hypertrophy in hypertension: an updated review. Expert Rev Cardiovasc Ther 2010; 8: 781–792.
Cuspidi C, Sala C, Valerio C, Negri F, Mancia G . Nocturnal hypertension and organ damage in dippers and nondippers. Am J Hypertens 2012; 25: 869–875.
Yokota H, Imai Y, Tsuboko Y, Tokumaru AM, Fujimoto H, Harada K . Nocturnal blood pressure pattern affects left ventricular remodeling and late gadolinium enhancement in patients with hypertension and left ventricular hypertrophy. PLoS ONE 2013; 8: e67825.
Jerrard-Dunne P, Mahmud A, Feely J . Circadian blood pressure variation: relationship between dipper status and measures of arterial stiffness. J Hypertens 2007; 25: 1233–1239.
Vasunta RL, Kesäniemi YA, Ylitalo A, Ukkola O . Nondipping pattern and carotid atherosclerosis in a middle-aged population: OPERA Study. Am J Hypertens 2012; 25: 60–66.
de la Sierra A, Gorostidi M, Banegas JR, Segura J, de la Cruz JJ, Ruilope LM . Nocturnal hypertension or nondipping: which is better associated with the cardiovascular risk profile? Am J Hypertens 2014; 27: 680–687.
Turak O, Ozcan F, Tok D, Işleyen A, Sökmen E, Taşoğlu I et al. Serum uric acid, inflammation, and nondipping circadian pattern in essential hypertension. J Clin Hypertens (Greenwich) 2013; 15: 7–13.
Erdogan D, Icli A, Aksoy F, Akcay S, Ozaydin M, Ersoy I et al. Relationships of different blood pressure categories to indices of inflammation and platelet activity in sustained hypertensive patients with uncontrolled office blood pressure. Chronobiol Int 2013; 30: 973–980.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest
Rights and permissions
About this article
Cite this article
Androulakis, E., Papageorgiou, N., Chatzistamatiou, E. et al. Improving the detection of preclinical organ damage in newly diagnosed hypertension: nocturnal hypertension versus non-dipping pattern. J Hum Hypertens 29, 689–695 (2015). https://doi.org/10.1038/jhh.2015.5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2015.5
This article is cited by
-
Non-Dipping Blood Pressure or Nocturnal Hypertension: Does One Matter More?
Current Hypertension Reports (2024)
-
Clinical Significance of Nocturnal Hypertension and Nighttime Blood Pressure Dipping in Hypertension
Current Hypertension Reports (2024)
-
The effects of Olmesartan/amlodipine administered in the Morning or At Night on nocturnal blood pressure reduction in Chinese patients with mild-moderate essential hypertension (OMAN Trial): study protocol for a prospective, multicenter, randomized, open-label clinical trial {1}
Trials (2023)